Application of High Epidural Combined General Anesthesia in Laparoscopic Liver Resection
-
摘要:
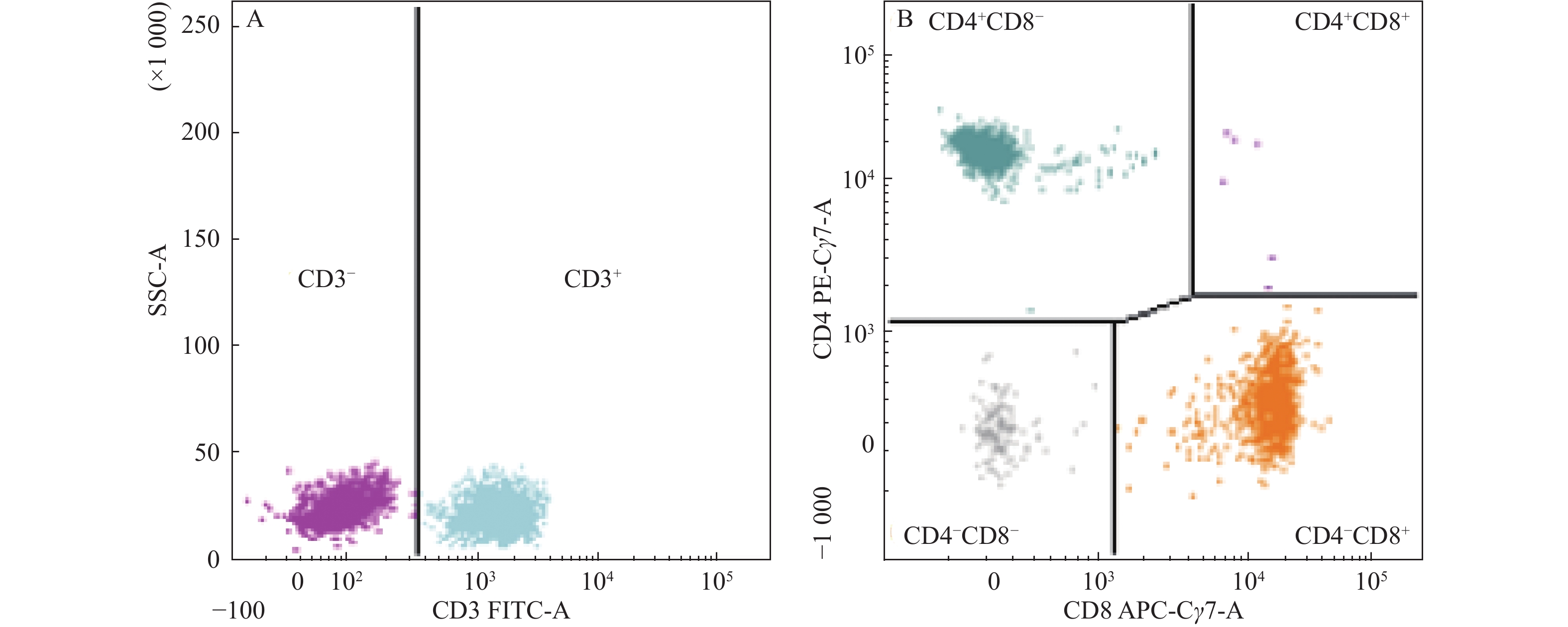
目的 探讨高位硬膜外复合全麻在腹腔镜肝脏切除术中的应用。 方法 随机选取曲靖市第二人民医院2020年3月至2022年9月间,腹腔镜肝脏切除术患者86例为对象,采用数字表法均分为2组各43例。对照组围术期行全身麻醉;观察组采用高位硬膜外复合全麻。记录2组围术期血流动力学水平、T淋巴细胞亚群、术中出血量及麻醉相关并发症情况。 结果 2组围术期血流动力学呈先上升后下降趋势;2组T1、T2时间点SBP、DBP及HR水平高于T0时间点,差异有统计学意义(P < 0.05);观察组T1、T2时间点SBP、DBP及HR水平低于对照组,差异有统计学意义(P < 0.05);2组术后48 h T淋巴细胞水平出现不同程度下降;观察组CD3+、CD4+、CD4+/CD8+水平高于对照组,差异有统计学意义(P < 0.05);2组呼吸暂停、苏醒延迟、低氧血症、呼吸抑制及尿潴留发生率比较,差异无统计学意义(P > 0.05)。 结论 高位硬膜外复合全麻用于腹腔镜肝脏切除术中,能稳定血流动力学水平,还能降低患者中心静脉压,且未增加术中出血,对T淋巴细胞亚群水平影响较小,麻醉安全性较高,值得推广应用。 Abstract:Objective To investigate the application of high epidural combined general anesthesia in laparoscopic liver resection. Methods A total of 86 patients with laparoscopic hepatectomy in the Second People’s Hospital of Qujing City from March 2020 to September 2022 were randomly selected and divided into 2 groups with 43 cases in each group by the number table method. The control group received general anesthesia during perioperative period, while the observation group received high epidural combined general anesthesia. The perioperative hemodynamic level, Perioperative hemodynamic level, T lymphocyte subsets, intraoperative blood loss and anesthesia related complications were recorded in the two groups. Results The perioperative hemodynamics of the two groups increased first and then decreased. The levels of SBP, DBP and HR at T1 and T2 in the two groups were higher than those at T0, and the differences were statistically significant (P < 0.05 ). The levels of SBP, DBP and HR at T1 and T2 in the observation group were lower than those in the control group, and the differences were statistically significant ( P < 0.05 ). The level of T lymphocytes in the two groups decreased in different degrees at 48 h after operation. The levels of CD3+, CD4+ and CD4+/CD8+ in the observation group were significantly higher than those in the control group (P < 0.05 ). There was no significant difference being found in the comparison of the incidences of apnea, delayed recovery, hypoxemia, respiratory depression and urinary retention between the two groups (P > 0.05 ). Conclusion The application of high epidural combined general anesthesia in laparoscopic liver resection can stabilize the hemodynamic level, reduce the central venous pressure of patients, and does not increase intraoperative bleeding, has little effect on the level of T lymphocyte subsets, and has high anesthesia safety, which is worthy of promotion and application. -
Key words:
- High epidural /
- General anesthesia /
- Laparoscopic liver resection /
- T lymphocyte subsets /
- Security
-
表 1 2组血流动力学比较(
$\bar x \pm s $ )Table 1. Hemodynamic comparison between the two groups (
$\bar x \pm s $ )组别 血流动力学 T0 T1 T2 T3 T4 观察组(n=43) SBP(mmHg) 132.59 ± 12.65 143.24 ± 14.69*# 148.68 ± 16.54*# 142.21 ± 15.43 134.51 ± 12.68 DBP(mmHg) 83.24 ± 6.73 88.51 ± 7.82*# 92.39 ± 8.92*# 90.13 ± 8.43 87.31 ± 7.52 HR(次/min) 71.23 ± 4.52 78.95 ± 6.41*# 82.13 ± 7.04*# 79.43 ± 6.63 77.51 ± 6.34 对照组(n=43) SBP(mmHg) 132.62 ± 12.68 151.59 ± 15.53* 161.43 ± 18.82* 143.42 ± 15.48 135.64 ± 12.69 DBP(mmHg) 83.41 ± 6.75 90.45 ± 7.49* 96.41 ± 8.95* 92.14 ± 8.67 89.56 ± 7.81 HR(次/min) 71.25 ± 4.54 86.43 ± 6.79* 97.84 ± 9.15* 81.24 ± 6.68 78.39 ± 6.52 与T0时间点比较,*P < 0.05;与对照组比较,#P < 0.05。 表 2 2组T淋巴细胞水平及术中出血量比较(
$\bar x \pm s $ )Table 2. Comparison of T lymphocyte level and intraoperative blood loss between the two groups (
$\bar x \pm s $ )组别 n CD3+ CD4+ CD4+/CD8+ 术中出血量(mL) 麻醉前 术后48 h 麻醉前 术后48 h 麻醉前 术后48 h 观察组 43 68.68 ± 6.73 65.63 ± 5.67* 39.68 ± 4.36 34.32 ± 3.96* 1.34 ± 0.31 1.30 ± 0.29* 172.31 ± 21.69 对照组 43 68.74 ± 6.76 62.15 ± 5.39* 39.70 ± 4.41 31.49 ± 3.98* 1.36 ± 0.34 1.23 ± 0.23* 175.29 ± 22.13 t 1.593 6.672 0.985 5.471 1.102 7.436 0.614 P 0.714 0.001 0.341 0.001 0.698 0.001 0.328 与麻醉前比较,*P < 0.05。 表 3 2组麻醉相关并发症比较[n(%)]
Table 3. Comparison of anesthesia related complications between the two groups [n(%)]
组别 n 呼吸暂停 苏醒延迟 低氧血症 呼吸抑制 尿潴留 发生率 观察组 43 1(2.33) 0(0.00) 1(2.33) 0(0.00) 1(2.33) 3(6.98) 对照组 43 1(2.33) 2(4.65) 1(2.33) 1(2.33) 1(2.33) 6(13.95) χ2 0.001 2.048 0.001 1.012 0.001 1.117 P 1.000 0.152 1.000 0.314 1.000 0.291 -
[1] 肖亮,周乐杜. 肝脏膜结构再认识及在腹腔镜肝切除术中的应用[J]. 中国普通外科杂志,2022,31(1):1-7. [2] 陆晓燕,时萍,吴卉,等. 患者参与在腹腔镜肝脏切除加速康复外科护理中的应用[J]. 腹腔镜外科杂志,2020,25(8):588,617. doi: 10.13499/j.cnki.fqjwkzz.2020.08.588 [3] 中华医学会外科学分会肝脏外科学组,中华医学会数字医学分会,中国医师协会肝癌专业委员会,等. 增强与混合现实技术在腹腔镜复杂性肝切除术中应用的中国专家共识[J]. 中华外科杂志,2022,60(6):517-523. doi: 10.3760/cma.j.cn112139-20220328-00127 [4] Hasanin A,Mostafa M,Abdulatif M. Combined Thoracic Spinal-Epidural Anesthesia in Laparoscopic Sleeve Gastrectomy: a Risk–Benefit Assessment[J]. Obesity Surgery,2022,32(6):2092-2093. doi: 10.1007/s11695-022-06034-8 [5] 程琪,朱鹏,廖威,等. 肝下下腔静脉阻断技术在机器人辅助腹腔镜肝切除术中的应用效果[J]. 中华外科杂志,2021,59(1):18-23. [6] 谭志国,朱岱阳,孙增鹏,等. 右肝蒂Glisson鞘外阻断在腹腔镜右半肝切除术中的应用初探[J]. 肝胆胰外科杂志,2020,32(8):449-452. [7] 高峻峰,雷义高,秦小杰,等. 全身麻醉联合硬膜外麻醉在腹腔镜胆囊切除术高血压患者中的应用效果观察[J]. 现代生物医学进展,2020,20(7):1355-1359. doi: 10.13241/j.cnki.pmb.2020.07.034 [8] Fan Y,Liu X,Wu S,et al. The risk factors for cognitive dysfunction in elderly patients after laparoscopic surgery: A retrospective analysis[J]. Medicine,2021,100(2):e23977-e23977. doi: 10.1097/MD.0000000000023977 [9] 戴志慧,杜金林,王建平,等. 改良横结肠保护性造口及皮下腹腔外造口关闭在腹腔镜中低位直肠癌前切除术的应用[J]. 中华胃肠外科杂志,2020,23(7):714-716. doi: 10.3760/cma.j.cn.441530-20191014-00451 [10] 谢卫玲,金娟娟,周辉,等. 小剂量纳洛酮对腹腔镜子宫切除术后地佐辛静脉自控镇痛效果的影响[J]. 中国医师杂志,2022,24(7):1104-1107. doi: 10.3760/cma.j.cn431274-20210416-00437 [11] Xu Z Z,Li H J,Li M H,et al. Epidural Anesthesia–Analgesia and Recurrence-free Survival after Lung Cancer Surgery: A Randomized Trial[J]. Anesthesiology,2021,135(3):419-432. doi: 10.1097/ALN.0000000000003873 [12] 郭志唐,龙奎,王琳,等. 精准肝切除理念在腹腔镜下Ⅰ型肝血管瘤剥除术中的应用[J]. 重庆医学,2021,50(5):749-752. doi: 10.3969/j.issn.1671-8348.2021.05.007 [13] 边长荣,王冬梅. 全身麻醉复合硬膜外麻醉与静吸复合全身麻醉在腹腔镜子宫切除术中应用观察[J]. 贵州医药,2020,44(6):898-900. doi: 10.3969/j.issn.1000-744X.2020.06.022 [14] 廉海光,李建,吴红发,等. 脊椎硬膜外麻醉联合静吸复合全身麻醉在老年腹腔镜下全子宫切除术中的应用观察[J]. 老年医学与保健,2020,26(6):980-983. doi: 10.3969/j.issn.1008-8296.2020.06.022 [15] Bouras A F,Decanter G,Marin H,et al. Postoperative Outcomes After Laparoscopic Liver Resections in Low and High-Volume Centers: A Multicentric Case-Matched Comparative Study[J]. World Journal of Surgery,2022,46(2):362-369. doi: 10.1007/s00268-021-06369-w [16] 齐英军,冯英博. 全身麻醉复合硬膜外阻滞麻醉在腹腔镜手术治疗老年直肠癌中的应用效果及对应激反应的影响[J]. 癌症进展,2020,18(19):2016-2018. [17] 王岩. 单纯全身麻醉与全身麻醉联合硬膜外麻醉在妇科腹腔镜手术患者中的临床应用价值[J]. 中国妇幼保健,2020,35(20):3892-3894. doi: 10.19829/j.zgfybj.issn.1001-4411.2020.20.057 [18] 鲍春燕. 硬膜外阻滞复合全身麻醉对腹腔镜子宫切除术围术期疼痛介质的影响[J]. 检验医学与临床,2020,17(8):1047-1050. doi: 10.3969/j.issn.1672-9455.2020.08.011 [19] 陈亚进,曹君. 从创新到标准化:腹腔镜肝切除术进展和展望(1990-2020)[J]. 中国实用外科杂志,2020,40(2):158-162. -






 下载:
下载: