Clinical Data Analysis of 108 Patients with Primary Hyperparathyroidism
-
摘要:
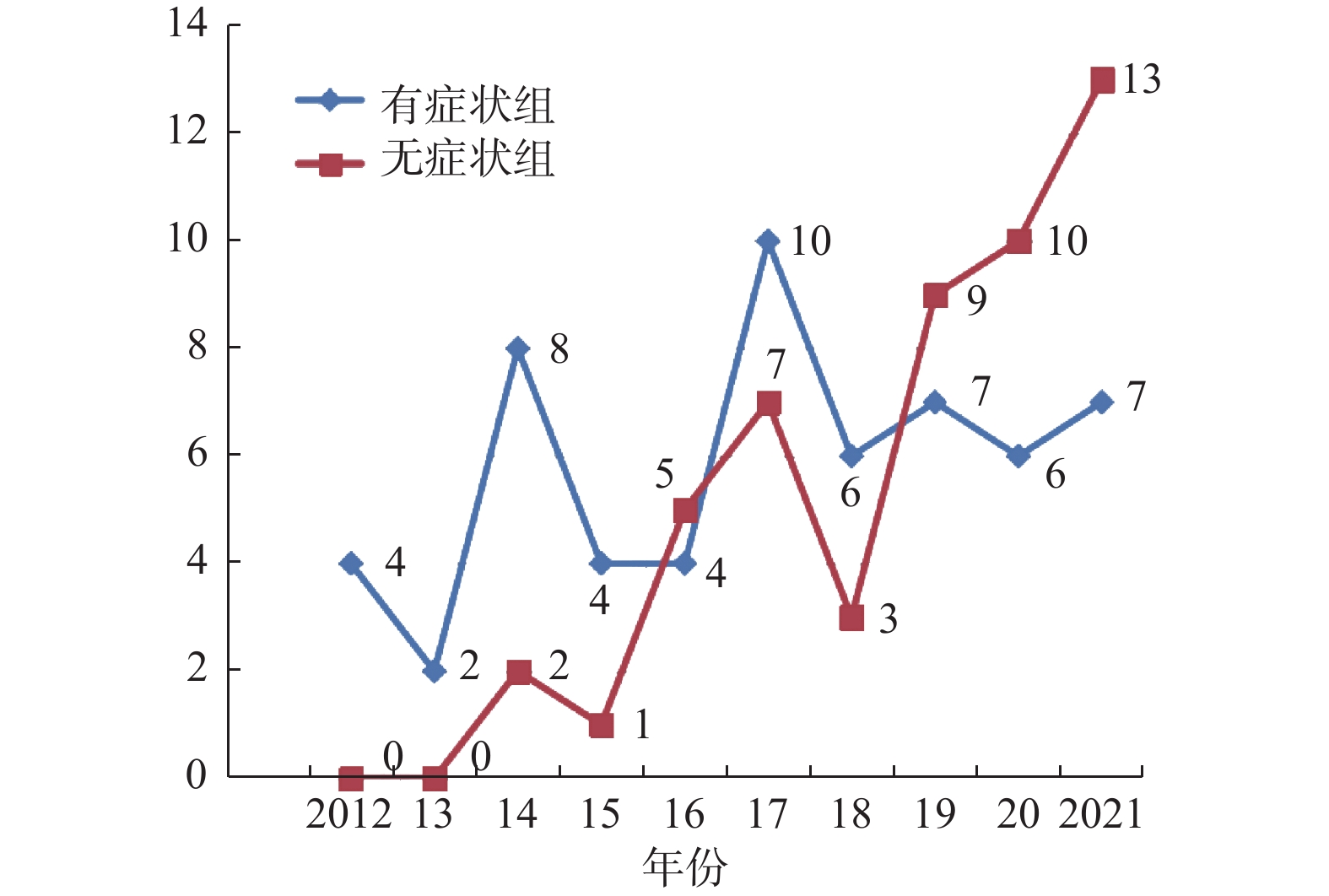
目的 分析云南省肿瘤医院原发性甲状旁腺功能亢进症(PHPT)患者的临床资料,总结临床特点,提高临床工作者对该病的认识及诊治水平。 方法 回顾性整理分析云南省肿瘤医院2012年1月至2021年12月收治的108例PHPT患者的相关资料,比较症状型与无症状型PHPT的临床差异。 结果 108例PHPT患者中,症状组58例(53.7%),无症状组50例(46.3%)。2组患者中男性发病年龄均早于女性,差异有统计学意义(P = 0.001);症状组中男性占比高于女性,差异有统计学意义(P = 0.002)。症状组患者的发病年龄较无症状组更早(P = 0.001),病程更长(P < 0.001)。PHPT就诊呈增长趋势,且2018年后无症状组就诊增长趋势较症状组更明显。症状组患者以骨骼系统受损最常见(84.5%),而无症状组患者多因意外发现血钙升高或颈部超声发现可疑病灶就诊。99mTc-MIBI病灶定位的准确性(94.44%)高于颈部超声(78.7%)或颈部增强CT(78.7%),但99mTc-MIBI联合颈部超声检查可提高术前定位的准确性(97.22%)。 结论 PHPT就诊呈增长趋势,且近年来无症状型患者就诊增加趋势较症状型更明显;PHPT患者中,男性较女性的病情更重,且发病年龄更早;99mTc-MIBI术前定位准确性最高,联合颈部超声可进一步提高定位的准确性。 -
关键词:
- 原发性甲状旁腺功能亢进症 /
- 无症状型 /
- 临床特点 /
- 甲状旁腺切除术
Abstract:Objective To analyze the clinical data of patients with PHPT in Yunnan Cancer Hospital, to explore the clinical characteristics, and improve the understanding, diagnosis and treatment of this disease. Methods The clinical data of 108 PHPT patients admitted to Yunnan Cancer Hospital from January 2012 to December 2021 were retrospectively analyzed, and the clinical differences between symptomatic PHPT and asymptomatic PHPT were compared. Results Among 108 patients with PHPT, 58 (53.7%) were in the symptomatic group and 50 (46.3%) were in the asymptomatic group. The age of onset was earlier in males than in females, the difference was statistically significant (P = 0.001). The proportion of men in the symptom group was higher than that of women, the difference was statistically significant (P = 0.002). Patients of sPHPT had an earlier onset age (P = 0.001) and longer disease duration than those of aPHPT (P < 0.001). PHPT visits were increasing, and the increasing trend was more pronounced in aPHPT after 2018 than in sPHPT. Impairment of the skeletal system (84.5%)was the most common patient in the symptomatic group, while patients in the asymptomatic group often had unexpected findings of blood calcium elevation or suspicious lesions found by neck ultrasound.The accuracy of 99mTc-MIBI lesion localization (94.44%)is higher than neck ultrasound (78.7%)or neck contrast-enhanced CT, but 99mTc-MIBI combined with neck ultrasound examination may improve the accuracy of preoperative localization (97.22%). Skeletal system damage was the most common in sPHPT (84.5%), while in aPHPT group, patients were more likely to seek medical treatment due to accidental discovery of elevated blood calcium or suspicious lesions found by cervical ultrasound. The accuracy of 99mTc-MIBI lesion localization (94.44%) was higher than that of cervical ultrasound (78.7%) or cervical contrast CT (78.7%), but 99mTc-MIBI combined with cervical ultrasound could improve the accuracy of preoperative localization (97.22%). Conclusion There is an increasing trend for PHPT visits. In recent years, the increase trend of aPHPT patients is more obvious than that of sPHPT; Male patients were more severely ill than female patients and had an earlier onset in PHPT. The localization accuracy of 99mTc-MIBI is the highest, and the combination of neck ultrasound can improve the localization accuracy. -
表 1 男女患者一般资料比较
Table 1. Comparison of general data between male and female patients
变量 男(n = 28) 女(n = 80) t/Z/χ2 P 症状(有/无) 22/6 36/44 9.402 0.002* 年龄(岁) 38.07 ± 12.22 47.76 ± 12.68 −3.512 0.001* 病程(月) 5(2,21) 3(0.54,12) 1.822 0.068 *P < 0.05。 表 2 症状组与无症状组一般资料比较
Table 2. Comparison of sPHPT and aPHPT general data
变量 症状组
(n = 58)无症状组
(n = 50)t/Z/χ2 P 性别(男/女) 22/36 6/44 9.402 0.002* 年龄(岁) 41.45 ± 13.38 49.66 ± 11.67 −3.372 0.001* 病程(月) 6(3,24) 1(0.33,3) 5.806 < 0.001* 收缩压(mmHg) 124.88 ± 20.16 123.62 ± 14.37 0.368 0.713 舒张压(mmHg) 84.36 ± 12.01 81.76 ± 9.04 1.255 0.212 *P < 0.05。 表 3 术前各定位检查的准确性
Table 3. Accuracy of each preoperative localization examination before surgery
检查项目 检出 未检出 合计 检出率(%) 颈部超声 85 23 108 78.70 MIBI 68 4 72 94.44 颈部CT 59 30 89 66.29 超声+MIBI 70 2 72 97.22 表 4 症状组与无症状组病灶定位检查比较(n)
Table 4. Comparison of sPHPT and aPHPT lesion localization examinations (n)
检查项目 症状组 无症状组 χ2 P 检出 未检出 检出 未检出 颈部超声 51 7 34 16 6.364 0.012* MIBI 45 1 23 3 1.278 0.258 颈部CT 32 9 27 21 4.702 0.030* *P < 0.05。 表 5 症状组与无症状组病理类型分布情况(n)
Table 5. Distribution of sPHPT and aPHPT pathology types (n)
病理类型 有症状组 无症状组 合计 χ2 P 腺瘤 52 45 97 增生 4 5 9 腺癌 2 0 2 合计 58 50 108 0.118 0.906 表 6 病灶最大径与PTPH患者各生化指标间的相关性
Table 6. Correlation between the maximum diameter of the lesions and each biochemical index
变量 相关系数 P 血钙 0.320 0.001* 血磷 −0.234 0.015* 血镁 −0.233 0.015* PTH 0.400 < 0.001* ALP 0.350 < 0.001* 骨钙素 0.419 < 0.001* *P < 0.05。 -
[1] Campbell M J. The definitive management of primary hyperparathyroidism: Who needs an operation?[J]. JAMA,2017,317(11):1167-1168. doi: 10.1001/jama.2017.1620 [2] Bilezikian J P,Bandeira L,Khan A,et al. Hyperparathyroidism[J]. Lancet,2018,391(10116):168-178. doi: 10.1016/S0140-6736(17)31430-7 [3] Hassan-Smith Z K,Criseno S,Gittoes N. Mild primary hyperparathyroidism-to treat or not to treat?[J]. Br Med Bull,2019,129(1):53-67. doi: 10.1093/bmb/ldy042 [4] 中华医学会骨质疏松和骨矿盐疾病分会, 中华医学会内分泌分会代谢性骨病学组. 原发性甲状旁腺功能亢进症诊疗指南[J]. 中华骨质疏松和骨矿盐疾病杂志, 2014, 7(3): 187-198. [5] 宋一丁,康维权,张建伟,等. 无症状型原发性甲状旁腺功能亢进患者的筛查与诊治[J]. 甘肃医药,2022,41(7):615-617. [6] Anagnostis P,Vaitsi K,Veneti S,et al. Efficacy of parathyroidectomy compared with active surveillance in patients with mild asymptomatic primary hyperparathyroidism: A systematic review and meta-analysis of randomized-controlled studies[J]. J Endocrinol Invest,2021,44(6):1127-1137. doi: 10.1007/s40618-020-01447-7 [7] 邢小平,王鸥,孟迅吾,等. 北京与纽约原发性甲状旁腺功能亢进症临床表现的比较[J]. 诊断学理论与实践,2006(6):483-486. [8] 姚晓爱,姜涛,魏伯俊,等. 无症状原发性甲状旁腺功能亢进症患者的临床特点[J]. 中南大学学报(医学版),2021,46(4):368-372. [9] 王鸥,邢小平,孟迅吾,等. 无症状型原发性甲状旁腺功能亢进症临床特点分析[J]. 中华骨质疏松和骨矿盐疾病杂志,2010,3(1):18-22. [10] Misgar R A,Dar P M,Masoodi S R,et al. Clinical and laboratory profile of primary hyperparathyroidism in Kashmir Valley: A single-center experience.[J]. Indian J Endocrinol Metab,2016,20(5):696-701. doi: 10.4103/2230-8210.190560 [11] Zhao L,Liu J M,He X Y,et al. The changing clinical patterns of primary hyperparathyroidism in Chinese patients: Data from 2000 to 2010 in a single clinical center[J]. J Clin Endocrinol Metab,2013,98(2):721-728. doi: 10.1210/jc.2012-2914 [12] Bilezikian J P,Cusano N E,Khan A A,et al. Primary hyperparathyroidism[J]. Nat Rev Dis Primers,2016,2:16033. doi: 10.1038/nrdp.2016.33 [13] 张浩. 无症状型原发性甲状旁腺功能亢进临床诊治[J]. 中国实用外科杂志,2014,34(4):311-314. [14] Macfarlane D P,Yu N,Leese G P. Asymptomatic and mild primary hyperparathyroidism[J]. Ann Endocrinol (Paris),2015,76(2):120-127. doi: 10.1016/j.ando.2015.03.001 [15] Abusahmin H,Geen J,Das G. Subclinical urolithiasis in patients with asymptomatic primary hyperparathyroidism[J]. Ther Adv Endocrinol Metab,2018,9(11):325-327. doi: 10.1177/2042018818788201 [16] 黄泽宇,苏磊,桑剑锋,等. 正常血钙型原发性甲状旁腺功能亢进症的临床特征及影响因素研究[J]. 中国全科医学,2023,26(11):1369-1374. [17] 陈孝平, 汪建平, 赵继宗. 外科学[M]. 第9版. 北京: 人民卫生出版社, 2018: 234-235. [18] Assadipour Y,Zhou H,Kuo E J,et al. End-organ effects of primary hyperparathyroidism: A population-based study[J]. Surgery,2019,165(1):99-104. doi: 10.1016/j.surg.2018.04.088 [19] Liu Y,Dang Y,Huo L,et al. Preoperative localization of adenomas in primary hyperparathyroidism: The value of (11)C-choline PET/CT in patients with negative or discordant findings on ultrasonography and (99m)Tc-sestamibi SPECT/CT[J]. J Nucl Med,2020,61(4):584-589. doi: 10.2967/jnumed.119.233213 [20] Lin X,Fan Y,Zhang Z,et al. Clinical characteristics of primary hyperparathyroidism: 15-year experience of 457 patients in a single center in China[J]. Front Endocrinol (Lausanne),2021,12:602221. doi: 10.3389/fendo.2021.602221 [21] Patel C N,Salahudeen H M,Lansdown M,et al. Clinical utility of ultrasound and 99mTc sestamibi SPECT/CT for preoperative localization of parathyroid adenoma in patients with primary hyperparathyroidism[J]. Clin Radiol,2010,65(4):278-287. doi: 10.1016/j.crad.2009.12.005 [22] 王曼,候亚琴,崔碧霄,等. (99m)Tc-MIBI SPECT/CT显像在原发性甲状旁腺功能亢进症术前诊断中的应用价值[J]. 首都医科大学学报,2022,43(6):861-866. [23] Lundstam K,Heck A,Mollerup C,et al. Effects of parathyroidectomy versus observation on the development of vertebral fractures in mild primary hyperparathyroidism[J]. J Clin Endocrinol Metab,2015,100(4):1359-1367. doi: 10.1210/jc.2014-3441 [24] Eller-Vainicher C,Filopanti M,Palmieri S,et al. Bone quality,as measured by trabecular bone score,in patients with primary hyperparathyroidism[J]. Eur J Endocrinol,2013,169(2):155-162. doi: 10.1530/EJE-13-0305 [25] Rowlands C,Zyada A,Zouwail S,et al. Recurrent urolithiasis following parathyroidectomy for primary hyperparathyroidism[J]. Ann R Coll Surg Engl,2013,95(7):523-528. doi: 10.1308/003588413X13629960048712 [26] Hu Y,Zhang X,Wang O,et al. The genomic profile of parathyroid carcinoma based on whole-genome sequencing[J]. Int J Cancer,2020,147(9):2446-2457. doi: 10.1002/ijc.33166 [27] Salcuni A S,Cetani F,Guarnieri V,et al. Parathyroid carcinoma[J]. Best Pract Res Clin Endocrinol Metab,2018,32(6):877-889. doi: 10.1016/j.beem.2018.11.002 [28] Bollen H,Decallonne B,Nuyts S. Radiation treatment for inoperable local relapse of parathyroid carcinoma with symptomatic hypercalcemia: A case report[J]. Front Oncol,2021,11:733772. doi: 10.3389/fonc.2021.733772 -






 下载:
下载: