Analysis of Pelvic Organ Prolapse and Related Factors in Primipara in Early Postpartum Period
-
摘要:
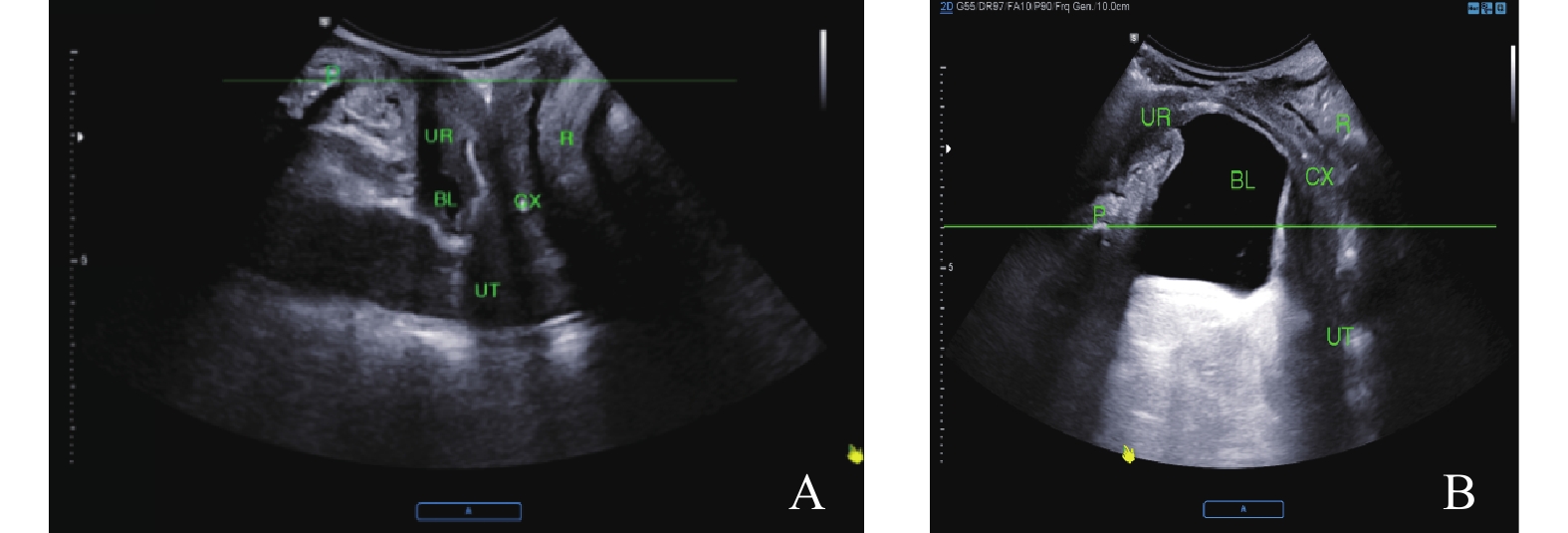
目的 探讨初产妇分娩各项因素与产后早期盆腔脏器脱垂(POP)的相关性。 方法 回顾性收集2021年1月至2022年6月于云南大学附属医院分娩后42~50 d进行常规超声检查的初产妇,病例组为超声诊断为POP的产妇141例,对照组为随机选取同时期未发生POP的产妇119例,结合产妇分娩方式、胎儿体重、顺产时产程及会阴侧切等指标分析初产妇分娩各项因素与产后POP的相关性。 结果 分娩各项因素中年龄、胎儿出生体重、顺产、顺产第2产程及会阴侧切与初产妇产后早期发生POP相关(P < 0.05)。 结论 年龄、胎儿出生体重、第2产程、顺产、会阴侧切是产后早期发生POP的危险因素,为临床预测产后发生POP提供参考,在妊娠及分娩过程中进行临床干预来降低产后POP的发生率。 Abstract:Objective To investigate the correlation between delivery factors and early postpartum pelvic organ prolapse (POP) in primipara. Methods From January 2021 to June 2022, primiparas who underwent routine ultrasound examination at the Affiliated Hospital of Yunnan University were retrospectively analysed. The case group included 141 primiparas diagnosed as POP by ultrasound, and the control group included 119 primiparas without POP randomly selected during the same period. The correlation between primiparas’ delivery factors and postpartum POP was analyzed by combining the indexes of fetal weight, labor process and lateral episiotomy. Results Age, birth weight, second stage of labor, vaginal delivery and episiotomy were significantly correlated with the occurrence of POP in primiparas (P < 0.05) . Conclusion Age, birth weight, second stage of labor, vaginal delivery, episiotomy are significantly correlated with early postpartum POP. These findings provide reference significance for clinical prediction of postpartum POP, and crucial for appropriate interventions during pregnancy and delivery, so as to reduce the incidence of postpartum POP. -
Key words:
- Pelvic organ prolapse /
- Factors of childbirth /
- Correlation
-
表 1 2组初产妇产后膀胱颈、宫颈外口、直肠壶腹移动度比较(
$\bar x \pm s $ )Table 1. Comparison of postpartum movement of bladder neck,outer cervix and rectal ampulla between the two groups of primipara (
$\bar x \pm s $ )组别 n 膀胱颈
(mm)宫颈外口
(mm)直肠壶腹
(mm)病例组 141 22.96 ± 8.86 20.72 ± 7.43 16.27 ± 9.27 对照组 119 11.41 ± 2.22 10.30 ± 2.43 5.94 ± 1.34 t 11.832 9.851 13.219 P < 0.001* < 0.001* < 0.001* *P < 0.05。 表 2 分娩各项因素比较[(
$\bar x \pm s $ )/n(%)]Table 2. Comparison of various factors in childbirth [(
$\bar x \pm s $ )/n(%)]项目 病例组 对照组 t/χ2 P 年龄(岁) 29.81 ± 3.92 28.20 ± 4.06 3.239 < 0.001* 身高(cm) 159.20 ± 4.83 159.48 ± 5.12 -0.454 0.650 体重(Kg) 69.23 ± 9.19 67.55 ± 8.62 1.518 0.130 BMI(kg/m2) 27.31 ± 3.33 26.56 ± 3.12 1.869 0.063 分娩孕周(周) 39.12 ± 1.33 38.81 ± 1.67 1.682 0.094 胎儿出生体重(g) 3184 ± 427 3038 ± 441 2.697 0.007* BPD(cm) 9.18 ± 0.41 9.14 ± 0.47 0.735 0.463 生产方式 7.189 0.007* 顺产 119(84.4) 84(70.6) 剖宫产 22(15.6) 35(29.4) 顺产会阴裂伤(有/无) 70/49(58.8/41.2) 43/41(51.2/48.8) 1.502 0.220 顺产会阴侧切(是/否) 23/96(19.3/80.7) 31/53(36.9/63.1) 7.145 0.008* 顺产总产程(min) 332 ± 133.63 362 ± 158.26 1.454 0.148 顺产第1产程(min) 286 ± 121.69 318 ± 148.54 1.675 0.096 顺产第2产程(min) 39.6 ± 38.99 28.08 ± 17.88 2.527 0.012* 顺产第3产程(min) 6.43 ± 3.57 6.87 ± 3.81 0.842 0.401 *P < 0.05。 表 3 初产妇分娩各项因素与产后发生POP的二元Logistic回归分析
Table 3. Binary Logistic regression analysis of the factors of primiparous childbirth and the occurrence of postpartum POP
因素 β S.E. Wald P OR 95%CI 年龄 0.103 0.033 9.728 0.002* 1.109 1.039~1.183 胎儿出生体重 0.001 0.000 6.853 0.009* 1.001 1.000~1.001 会阴侧切 −0.860 0.326 6.967 0.008* 0.423 0.224~0.801 第2产程 0.013 0.005 5.757 0.016* 1.013 1.002~1.024 分娩方式 −0.813 0.307 7.0 0.008* 0.444 0.243~0.810 *P < 0.05。 -
[1] Thibault-gagnon S,Yusuf S,Langer S,et al. Do women notice the impact of childbirth-related levator trauma on pelvic floor and sexual function? Results of an observational ultrasound study[J]. Int urogynecol J,2014,25(10):1389-1398. doi: 10.1007/s00192-014-2331-z [2] Verbeek M,Hayward L. Pelvic floor dysfunction and its effect on quality of sexual life[J]. Sexual Medicine Reviews,2019,7(4):559-564. doi: 10.1016/j.sxmr.2019.05.007 [3] 付楝,曾凡慧,李玲,等. 1 000例产妇产后早期盆底功能障碍性疾病的筛查及其影响因素分析[J]. 医学理论与实践,2019,32(21):3419-3421. [4] Mathew S,Guzman Rojasr A,Salvesenk A,et al. Levator ani muscle injury and risk for urinary and fecal incontinence in parous women from a normal population, a cross-sectional study[J]. Neurourology and Urodynamics,2019,38(8):2296-2302. [5] Blomquistj L, Carroll M, Munoz A, et al. Pelvic floor muscle strength and the incidence of pelvic floor disorders after vaginal and cesarean delivery[J]. American Journal of Obstetrics and Gynecology,2020,222(1):62.e1-62.e8. [6] Urbankova I,Grohregin K,Hanacek J,et al. The effect of the first vaginal birth on pelvic floor anatomy and dysfunction[J]. International Urogynecology Journal,2019,30(10):1689-1696. [7] 陈旭,崔广和,李华林,等. 初产妇经阴道分娩各项因素与产后肛提肌损伤之间的相关性研究[J]. 中国优生与遗传杂志.,2022,30(1):85-90. [8] Nam G,Lee S R,Kim S H,et al. Importance of translabial ultrasound for the diagnosis of pelvic organ orolapse and its correlation with the POP-Q examination: Analysis of 363 cases[J]. Journal of Clinical Medicine,2021,10(18):.4267. doi: 10.3390/jcm10184267 [9] 汪文磊. 经会阴超声观察不同类型前盆腔器官脱垂的盆底解剖与功能变化[D]. 广州: 广州医科大学硕士学位论文, 2017. [10] 蒋莹,刘静华,刘丽. 会阴超声观察不同分娩方式产后女性盆腔器官位置及移动度的变化[J]. 中国妇幼卫生杂志,2018,9(1):44-47. [11] Zhao Y, Zhang C, Cui C, et al. Longitudinal changes in pelvic organ support among primiparas with postpartum pelvic organ prolapse: A follow-up MRI study [J]. International Journal of Gynecology & Obstetrics, 2023, Epub ahead of print. [12] 毛永江,武佳薇,张辉,等. 首次分娩女性产后6~8周盆底超声检查分析[J]. 中国全科医学,2017,20(27):3443-3447. [13] 易颖义,洪莉. 女性盆底功能障碍性疾病的肛提肌损伤研究进展[J]. 中国计划生育和妇产科,2021,13(8):19-22. [14] 喻红霞,苏杭,王晨雨,等. 三维超声评估不同分娩方式对女性盆腔脏器脱垂的影响[J]. 深圳中西医结合杂志,2019,29(24):16-18. [15] Krause H,Ng S K,Singasi I,et al. Incidence of intimate partner violence among Ugandan women with pelvic floor dysfunction[J]. Int J Gynaecol Obstet,2019,144(3):309-313. doi: 10.1002/ijgo.12748 [16] Tinetti A,Weir N,Tangyotkajohn U,et al. Help-seeking behaviour for pelvic floor dysfunction in women over 55: drivers and barriers[J]. International Urogynecology Journal,2018,29(11):1645-1653. doi: 10.1007/s00192-018-3618-2 [17] Swift S E,Pound T,Dias J K. Case-control study of etiologic factors in the development of severe pelvic organ prolapse[J]. International Urogynecology Journal and Pelvic Floor Dysfunction,2001,12(3):187-192. doi: 10.1007/s001920170062 [18] 蒋云秀,潘永寿,潘焕贵,等. 阴道分娩对初产妇产后耻骨直肠肌弹性及收缩功能的影响[J]. 广西医学,2019,41(10):1231-1233. [19] Vandelft K,Sultan A H,Thakar R,et al. The relationship between postpartum levator ani muscle avulsion and signs and symptoms of pelvic floor dysfunction[J]. Bjog-an International Journal of Obstetrics and Gynaecology,2014,121(9):1164-1171. doi: 10.1111/1471-0528.12666 [20] Rostaminia G,Peck J D,Quiroz L H,et al. Characteristics associated with pelvic organ prolapse in women with significant levator ani muscle deficiency[J]. Int Urogynecol J,2016,27(2):261-267. doi: 10.1007/s00192-015-2827-1 [21] 陈玲,傅煜,魏薇,等. 新生儿体质量对初产妇早期盆底结构及弹性的影响[J]. 中国超声医学杂志,2020,36(10):942-945. [22] 刘俊,王晓东,唐瑶,等. 新产程标准管理下第二产程时长对产妇盆底功能近期影响研究[J]. 中国实用妇科与产科杂志,2017,33(12):1271-1275. [23] Karahan N,Arslan H,Çam Ç. The behaviour of pelvic floor muscles during uterine contractions in spontaneous and oxytocin-induced labour[J]. Journal of Obstetrics and Gynaecology,2018,38(5):629-634. doi: 10.1080/01443615.2017.1399111 [24] Speksnijder L,Oomd M J,Van Bavel J,et al. Association of levator injury and urogynecological complaints in women after their first vaginal birth with and without mediolateral episiotomy[J]. Am J Obstet Gynecol,2019,220(1):93.e1-93.e9. doi: 10.1016/j.ajog.2018.09.025 [25] 李茗薇, 陈星, 马宁, 等 . 产后早期肛提肌裂孔扩张程度及相关因素分析 [J] 安徽理工大学学报(自然科学版). 2021, 41(6): 74-80. -






 下载:
下载: