The Analysis between Uterocervical Angles and Cervical Length in Predicting Preterm Labor
-
摘要:
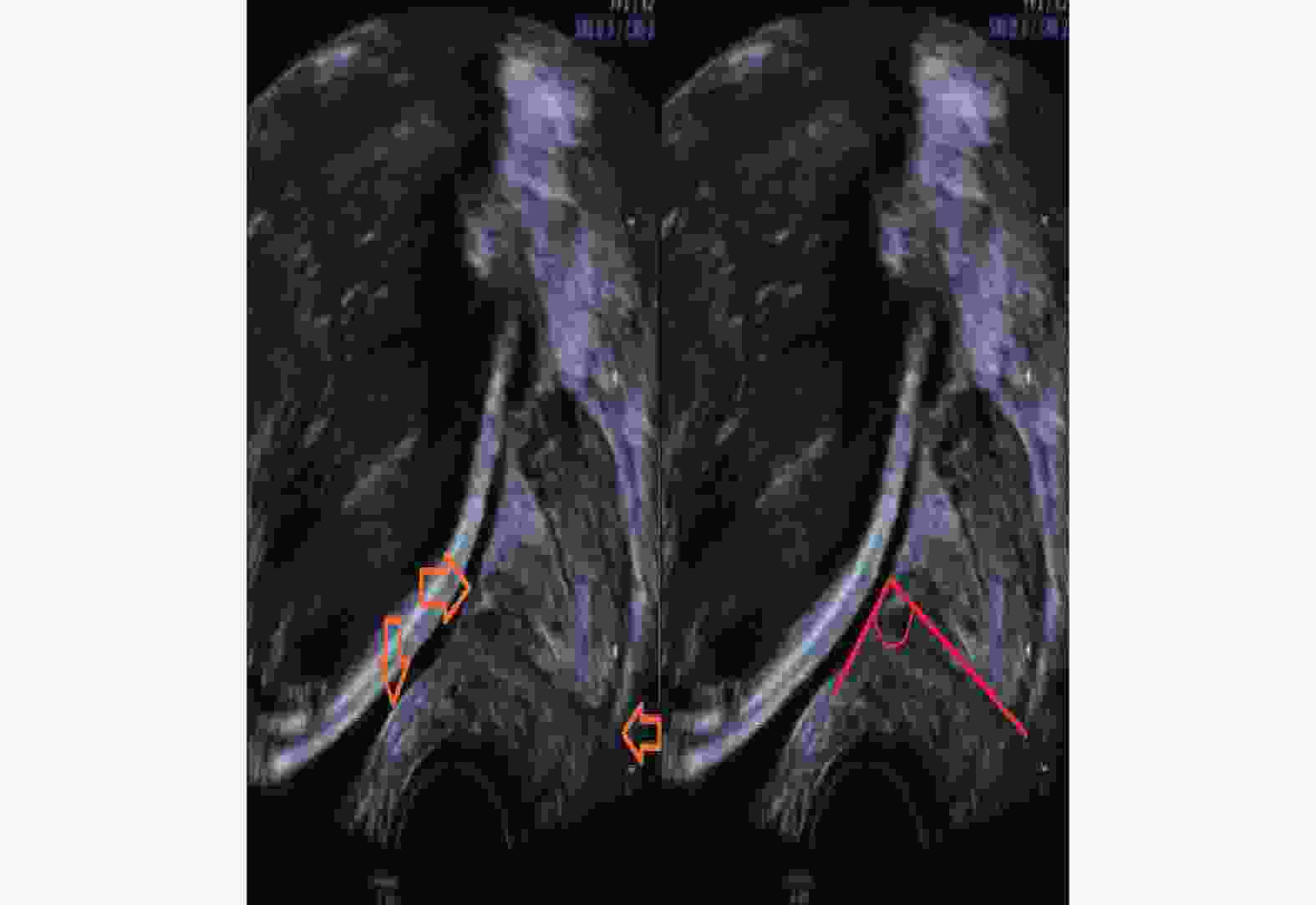
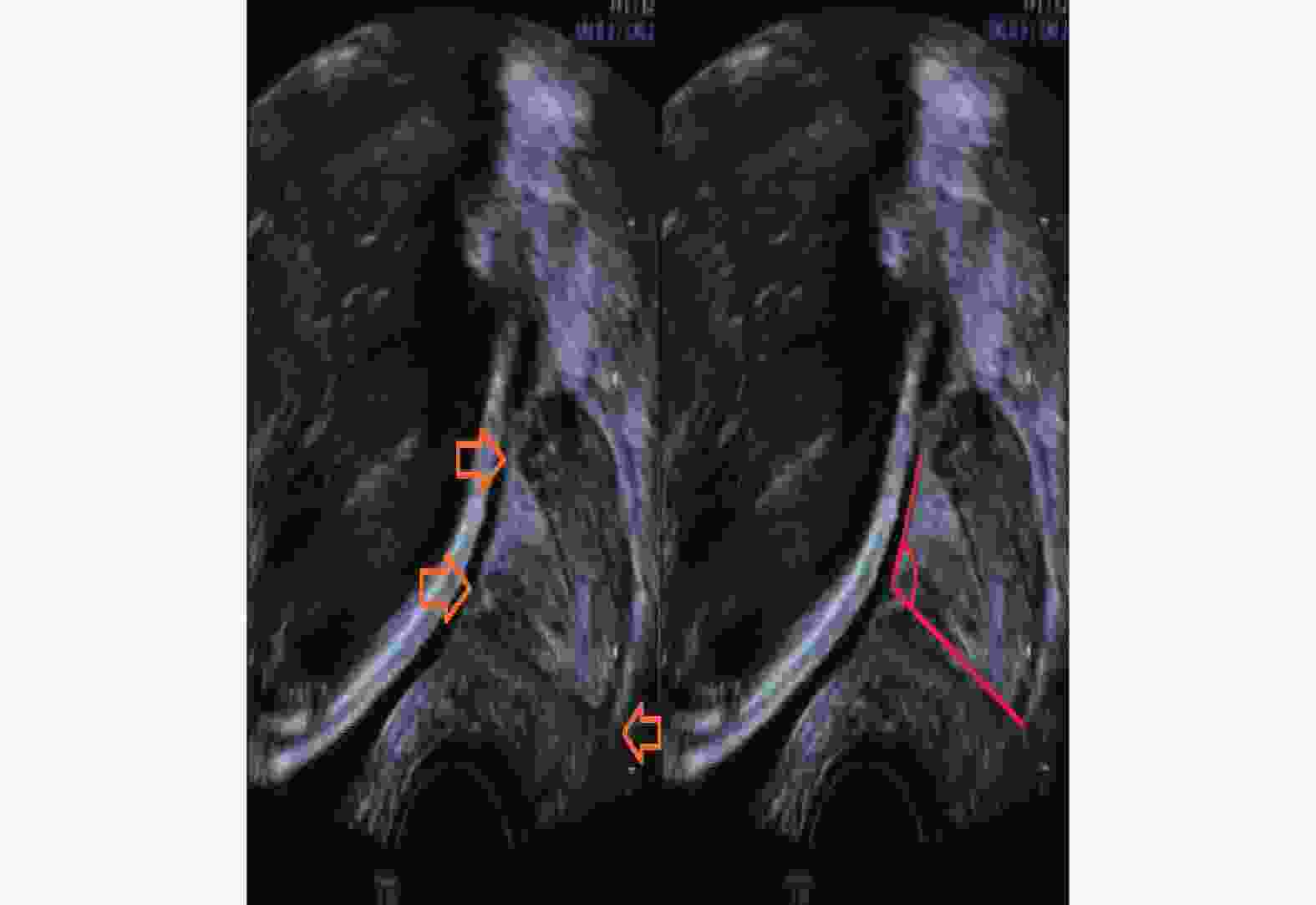
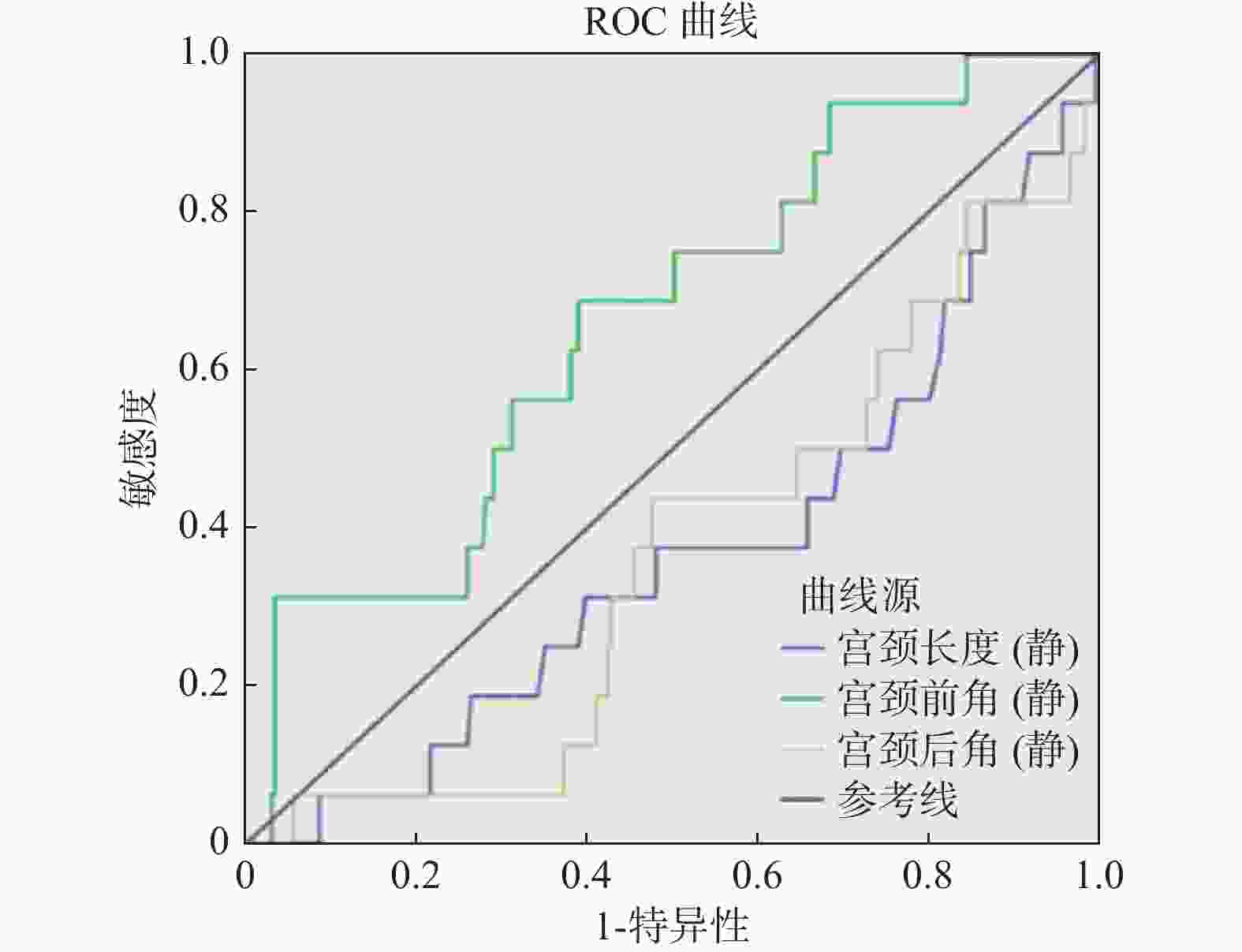
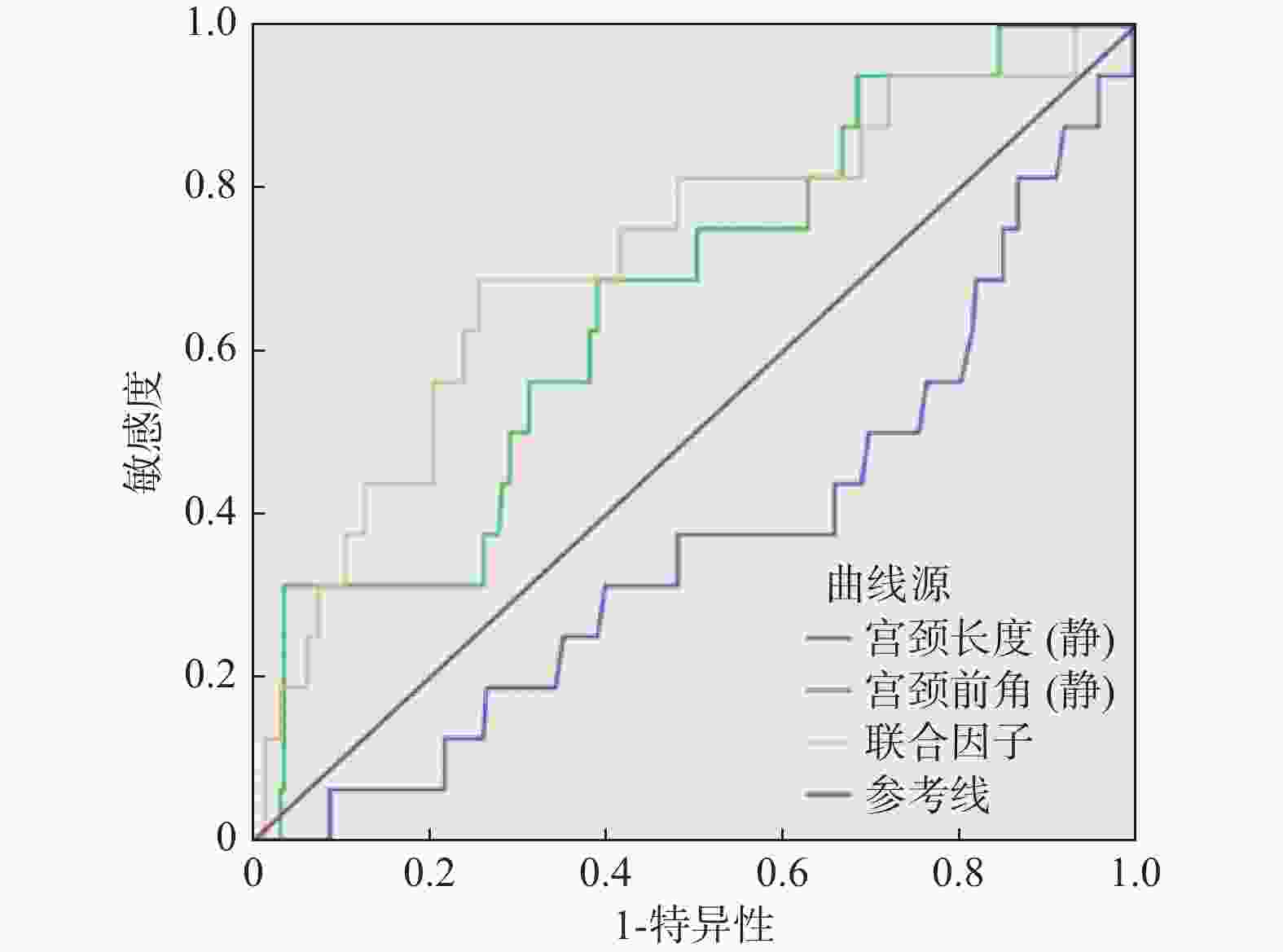
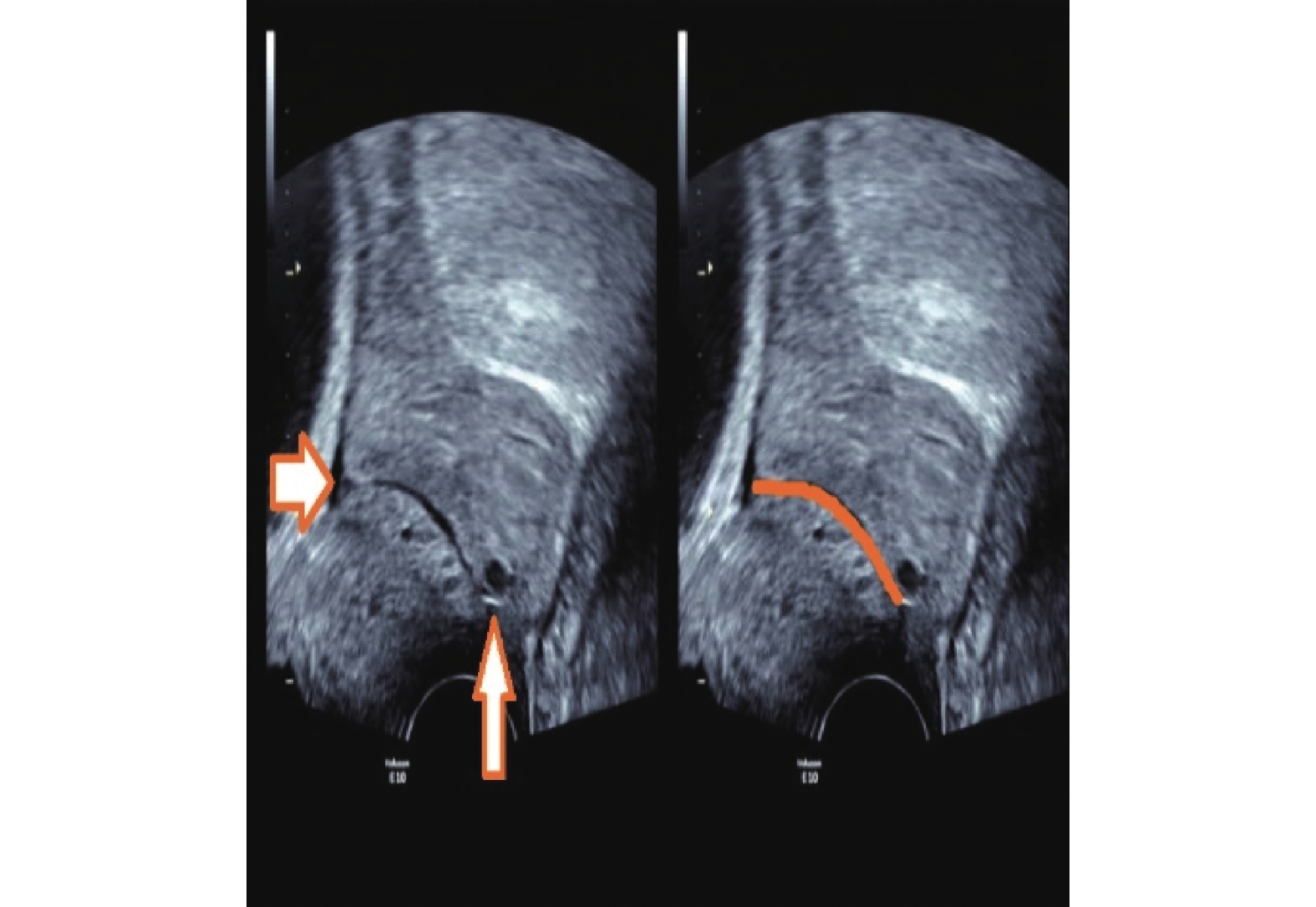
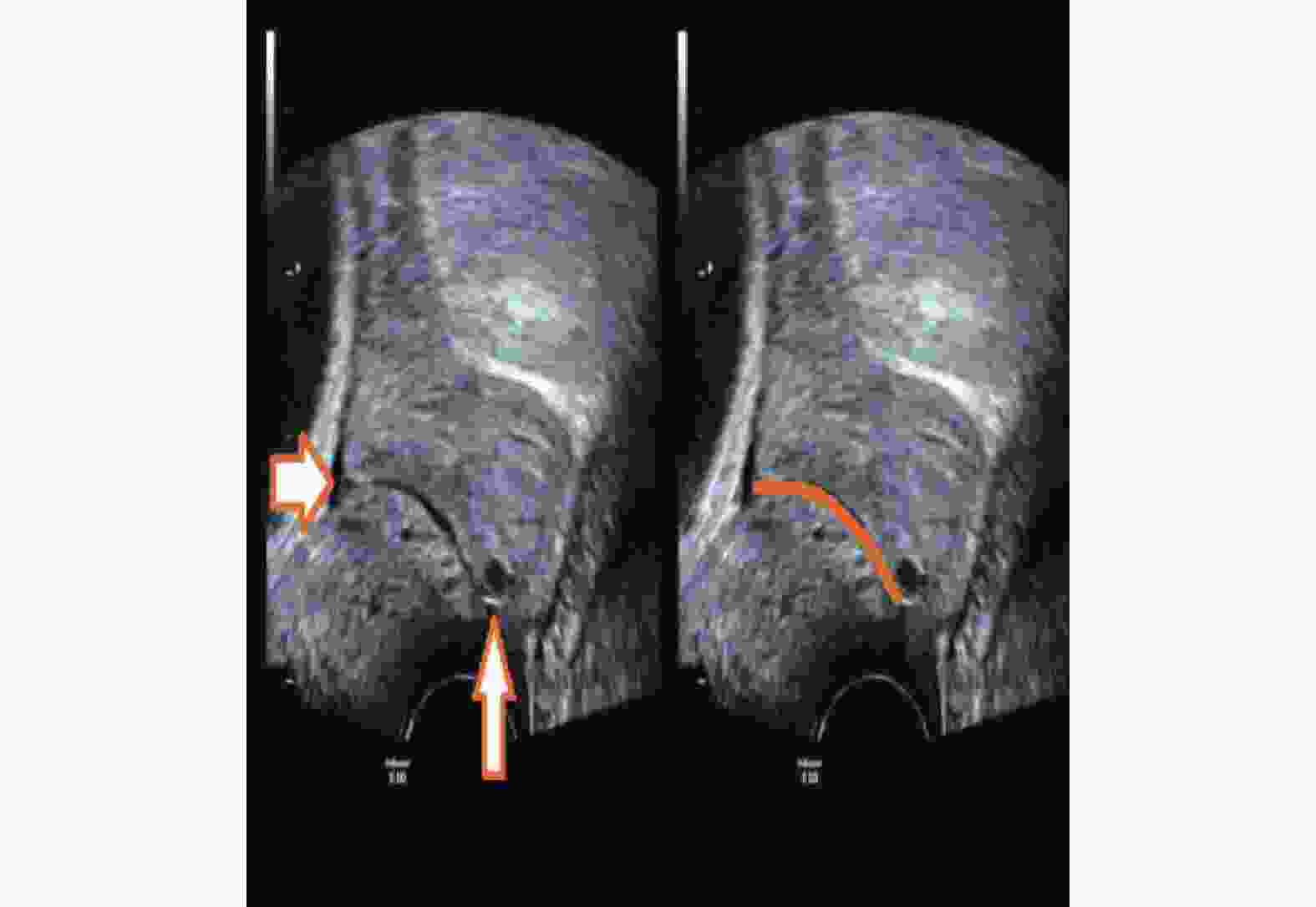
目的 研究子宫颈长度(CL)与子宫宫颈角(前角aUCA和后角pUCA)的早产预测价值,探索宫颈超声预测早产的新指标,以提供新的早产预测思路。 方法 对孕24~27+6周的252例妇女进行前瞻性队列研究,经阴道测量CL、aUCA和pUCA,根据分娩时间分为足月组和早产组,比较2组间各项指标的差异及彼此间的早产预测效能。 结果 236例足月产,16例早产,2组间aUCA和pUCA差异均存在统计学意义(P < 0.05),而CL无统计学意义( P > 0.05);计算出3项子宫颈超声指标的ROC曲线下面积(AUC),只有aUCA的AUC明显大于0.5,其阈值为102.22°;aUCA联合CL预测早产的ROC曲线下面积为0.715,联合因子的阈值为-2.385。 结论 孕24~27+6周单活胎孕妇CL的早产预测性欠佳,当aUCA≥102.22°需警觉自发性早产的发生,推荐联合aUCA和CL对无症状的孕妇进行早产预测;CL、pUCA的早产预测价值有待进一步研究。 Abstract:Objective To study the value of the cervical length (CL) and uterocervical angles (involving anterior uterocervical angles and posterior uterocervical angles) in predicting preterm labor to find new predicting markers via transvaginal ultrasound (TVU) and provide new predicting thoughts. Methods A total of 252 pregnant women selected from 24 to 27+6 weeks of gestation underwent TVU to measure their CL, aUCA and pUCA, and finally were divided into the normal group and the premature group according their delivery time. The difference and value of above markers between the two groups were compared in predicting preterm. Results Among them, 236 gave birth at term, and 16 went into labor prematurely.There was a statistically significant difference in aUCA and pUCA between the two groups (P < 0.05), while there was no statistically significant difference in CL ( P > 0.05). By calculating the area under the ROC curve (AUC) of three cervical ultrasound indicators, only the AUC of aUCA was significantly greater than 0.5, with a threshold of 102.22°; The area under the ROC curve for predicting preterm birth using aUCA combined with CL was 0.715, and the threshold for the combined factor was -2.385. Conclusion The predictive value of premature delivery for CL in single live pregnant women aged 24-27+6 weeks is not good. Compared with CL, the measurement of aUCA through TVU is more effective in predicting preterm birth and when measuring aUCA ≥102.22°, the occurrence of premature birth should be highly vigilant. The joint variable combined aUCA and CL is recommended as the predicting marker for pregnant women with single fetus but without any symptom. the predicting value of CL and pUCA need to be studied further. -
表 1 足月与早产组间CL、aUCA和pUCA的比较(
$\bar x \pm s $ )Table 1. Compare of CL,aUCA,pUCA between mature and premature groups (
$\bar x \pm s $ )指标 足月组 早产组 t P CL(cm) 3.68 ± 0.71 3.34 ± 0.71 −1.861 0.064 aUCA(°) 91.72 ± 29.57 109.55 ± 27.43 2.343 0.02* pUCA(°) 114.16 ± 29.45 98.69 ± 32.60 −2.02 0.045* *P < 0.05。 表 2 早产与子宫宫颈角的Logistic回归分析
Table 2. Logistic regression analysis between premature and UCAs
变量 B S.E. Wald P OR OR 95%CI 下限 上限 aUCA 0.052 0.018 8.406 0.004 1.053 1.017 1.091 pUCA −0.043 0.013 4.528 0.045 0.978 0.960 0.997 表 3 aUCA预测早产分布情况(n)
Table 3. Distribution of aUCA predicting premature (n)
分组 早产 足月产 总数 aUCA ≥ 102.22° 11 91 102 aUCA < 102.22° 5 141 146 总数 16 232 248 -
[1] Chawanpaiboon S,Vogel J P,Moller A B,et al. Global,regional,and national estimates of levels of preterm birth in 2014: A systematic review and modelling analysis[J]. Lancet Glob Health,2019,7(1):e37-e46. doi: 10.1016/S2214-109X(18)30451-0 [2] Gründler K,Gerber B,Stubert J. Uterocervical angle as a predictor of preterm birth on a high-risk collective between 20 and 31 weeks of gestation: A cohort analysis[J]. Acta Obstet Gynecol Scand,2020,99(11):1527-1533. doi: 10.1111/aogs.13955 [3] Sochacki W N,Wojcicki J,Bomba O D,et al. Anterior cervical angle as a new biophysical ultrasound marker for prediction of spontaneous preterm birth[J]. Ultrasound Obstet Gynecol,2015,46(3):377-8. doi: 10.1002/uog.14801 [4] Gokturk U,Cavkaytar S,Danısman N. Can measurement of cervical length,fetal head position and posterior cervical angle be an alternative method to Bishop score in the prediction of successful labor induction?[J]. J Matern Fetal Neonatal Med,2015,28(11):1360-1365. doi: 10.3109/14767058.2014.954538 [5] 郑倩文. 妊娠中晚期超声检测子宫颈形态与早产预测相关性的研究[D]. 昆明: 昆明医科大学硕士学位论文, 2021. [6] 陆燕飞,宋海国,苏嘉文,等. 不同超声方法在妊娠中期测量不同形态宫颈长度应用[J]. 中国计划生育学杂志,2019,27(11):1445-1447,1451. [7] 谢幸, 孔北华, 段涛. 妇产科学[M]. 第9版. 北京: 人民卫生出版社, 2018: 31, 95. [8] 田欣. 94例早产儿呼吸暂停相关因素分析与探讨[D]. 重庆: 重庆医科大学硕士学位论文, 2010. [9] 李茂军,吴青,石伟,等. 不同胎龄新生儿呼吸窘迫综合征临床特征分析[J]. 中国当代儿科杂志,2016,18(10):960-964. [10] 黄颖敏,陈智毅. 超声技术评估妊娠宫颈在预测早产中的应用进展[J]. 临床超声医学杂志,2021,23(1):61-64. [11] 中华医学会妇产科学分会产科学组. 早产临床诊断与治疗指南[J]. 中华妇产科杂志,2014,49(7):481-485. doi: 10.3760/cma.j.issn.0529-567x.2014.07.001 [12] Son M,Grobman W A,Ayala N K,et al. A universal mid-trimester transvaginal cervical length screening program and its associated reduced preterm birth rate[J]. Am J Obstet Gynecol,2016,214(3):365.e1-5. doi: 10.1016/j.ajog.2015.12.020 [13] Owen J,Yost N,Berghella V,et al. Mid-trimester endovaginal sonography in women at high risk for spontaneous preterm birth[J]. JAMA,2001,286(11):1340-1348. doi: 10.1001/jama.286.11.1340 [14] 陶玉程,丁文波,武心萍,等. 孕晚期超声测量宫颈前角及宫颈长度预测自发性早产价值[J]. 中国计划生育学杂志,2021,29(12):2679-2682. [15] 郑倩文,郭珊珊,刘继红. 宫颈重塑与早产相关性的研究进展[J]. 现代妇产科进展,2019,28(6):475-476. [16] Yenigul N N,Ercan F. The efficacy and efficiency of uterocervical angle measurements to predict preterm labor in idiopathic polyhydramnios patients: A prospective cohort study[J]. Z Geburtshilfe Neonatol,2021,225(2):129-133. doi: 10.1055/a-1176-2390 [17] Pruksanusak N,Sawaddisan R,Kor A O,et al. Comparison of reliability between uterocervical angle and cervical length measurements by various experienced operators using transvaginal ultrasound[J]. J Matern Fetal Neonatal Med,2020,33(8):1419-1426. [18] 金珈汐,仲莞,孙静莉,等. 超声测量宫颈角对早产的预测价值[J]. 中国医学影像学杂志,2020,28(9):692-695. -





 下载:
下载: