Development and Validation of Risk Predicting Model for Severe Diabetic Peripheral Neuropathy Based on Glucose Variability Parameters
-
摘要:
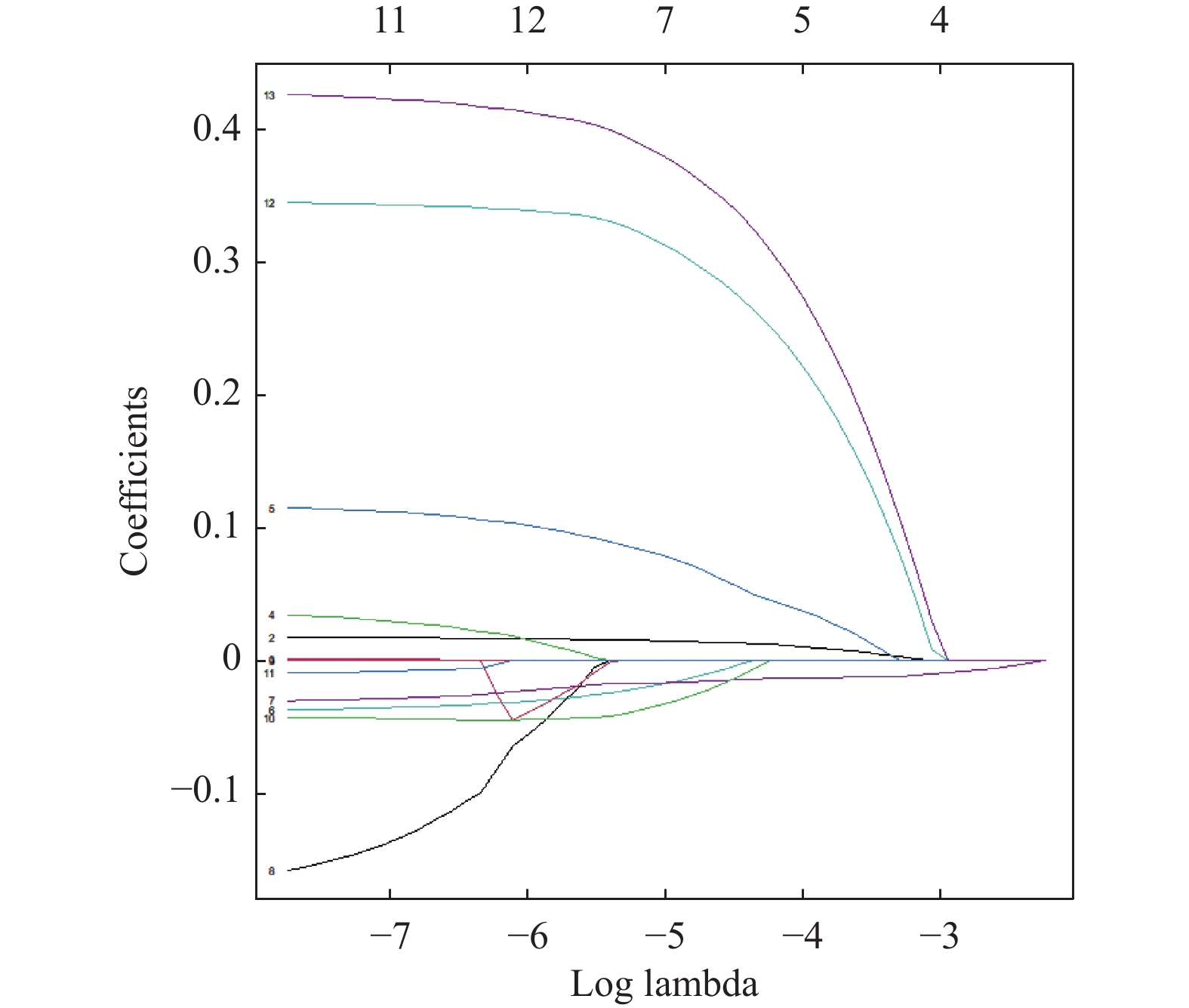
目的 使用葡萄糖变异参数建立2型糖尿病患者重度DPN发生的临床风险预测模型并进行验证,为糖尿病慢性并发症的防治提供参考依据。 方法 收集2019年4月至2020年5月昆明医科大学第一附属医院内分泌二科住院治疗且符合纳入标准的2型糖尿病周围神经病变患者323例的临床资料。据感觉阈值测定结果将患者分为重度糖尿病周围神经病变(DPN)组及非重度组。使用Lasso回归模型筛选重度DPN发生的预测因子,制作列线图使模型可视化,做ROC曲线、校准度曲线、决策曲线评估模型区分度、校准度及辅助模型临床决策。 结果 2型糖尿病患者重度DPN发生的显著预测因素为年龄、吸烟、血脂异常、HbA1c、TIR,同时TIR是重度DPN发生的独立危险因素;使用筛选变量建立重度DPN的预测模型。ROC曲线评估模型区分度AUC = 0.647(95%CI = 0.585 ~ 0.708,P < 0.05);HL拟合优度检验评估模型拟合度P = 0.074。 结论 葡萄糖变异参数中的TIR能够作为2型糖尿病患者重度DPN发生的显著预测因子,以TIR为基础建立的临床预测模型准确性尚可;建议患者经模型评估重度DPN发生风险大于20%(评分 > 250)即进行积极干预。 Abstract:Objective To develop and validate a risk prediction model for severe DPN in patients with type 2 diabetes using glucose variability parameters, and to provide the evidence for the prevention and treatment of diabetic chronic complications. Methods The medical records from 323 inpatients with T2DM who met the inclusion criteria were collected in the First Affiliated Hospital of Kunming Medical University from April 2019 to May 2020. Based on the professional sensory threshold measured, patients were divided into none-sever DPN group and severe DPN group. Lasso regression model was used to select risk factors. A risk prediction models for severe DPN was established and shown as a nomogram. ROC curve, calibration curve and decision curve analysis was used to validate the model. Results Age, smoking, dyslipidemia, HbA1c and TIR were significant predictors of severe DPN in type 2 diabetes patients, and TIR was an independent risk factor for severe DPN. An assessing model discrimination was established by using ROC curves with AUC = 0.653 (95%CI = 0.592 - 0.715, P < 0.05). The Hosmer-Lemeshow test was used to determine the model fit with P value 0.074. Conclusion TIR can be a significant predictor of the severe DPN in patients with T2DM, and the clinical prediction model established on the basis of TIR has the fair accuracy. It is recommended to actively intervene in the patients with a risk of severe DPN greater than 20% (score > 250) evaluated by the model. -
表 1 正中神经感觉阈值测定规范值 (μA)
Table 1. Normative values to determine the sensory thresholds of the median nerve sensory (μA)
刺激频率 无感觉减退 轻度感觉减退 中度感觉减退 重度感觉减退 2000 Hz < 401 401~466 466~546 > 546 250 Hz < 183 183~207 207~249 > 249 5 Hz < 104 104~127 127~154 > 154 表 2 腓浅及腓深神经神经感觉阈值测定规范值(μA)
Table 2. Normative values to determine the sensory thresholds of the deep peroneal nerve and the superficial peroneal nerve (μA)
刺激频率 无感觉减退 轻度感觉减退 中度感觉减退 重度感觉减退 2000 Hz < 525 525~582 582~686 > 686 250 Hz < 211 211~266 266~324 > 324 5 Hz < 173 173~197 197~241 > 241 表 3 组间一般资料、葡萄糖变异参数的比较
Table 3. Comparison of general information and glucose variability parameters between groups
临床指标 非重度DPN(n=194) 重度DPN(n=129) 检验统计量 P 男性[n(%)] 127(65.4) 73(56.6) 2.2254 0.108 年龄(岁) 55.36 ± 11.25 57.69 ± 11.36 −1.764 0.078 病程(a) 6(2,12) 7(3,12) 11744 0.347 BMI(kg/m2) 22.44(22.51,26.44) 23.88(21.78,26.45) 13768 0.127 吸烟[n(%)] 90(46.4) 47(36.4) 2.7509 0.076 高血压[n(%)] 85(43.8) 61(47.2) 0.25 0.539 血脂异常[n(%)] 142(73.1) 82(63.6) 2.9425 0.066 TC(mmol/L) 4.24(3.64,4.91) 4.44(3.59,5.15) 13869 0.452 TG(mmol/L) 1.98(1.22,2.79) 1.64(1.11,2.60) 11912 0.110 HDL-C(mmol/L) 0.93(0.78,1.08) 0.99(0.80,1.22) 10820 0.047* LDL-C(mmol/L) 2.63(1.97,3.11) 2.65(2.01,3.35) 11841 0.380 血肌酐(umol/L) 66.5(53.7,76.9) 65.0(53.7,76.9) 11583 0.268 空腹血糖(mmol/L) 7.1(5.38,9.98) 7.5(5.67,11.20) 11597 0.280 HbA1c(%) 8.3(7.1,10.7) 9.70(7.30,11.60) 10776 0.031* 葡萄糖平均值(mmol/L) 8.2(7.2,9.4) 9.0(7.6,10.2) 10265 0.006* 葡萄糖标准差(mmol/L) 1.9(1.4,2.5) 2.2(1.7,2.7) 10641 0.025* 葡萄糖变异系数(%) 23.49 ± 8.11 24.1 ± 7.56 −0.535 0.598 MAGE(mmol/L) 4.4(2.8,6.1) 4.7(3.0,6.4) 11564 0.248 TIR(%) 79(61,94) 70(48,87) 15166 0.001* 正态分布资料以($ \bar x \pm s$)表示,采用t检验,检验统计量为t;非正态分布资料以中位数及四分位数间距[M(QL,QU)]表示,使用Wilcoxon检验,检验统计量为W;二分类资料以χ(%)表示,使用卡方检验,检验统计量为χ2;*P < 0.05。 表 4 葡萄糖变异参数多重共线性检验
Table 4. Multicollinearity test of glucose variability parameters
葡萄糖变异参数 平均值 标准差 变异系数 MAGE TIR $\sqrt {{\rm{VIF}}} $ 4.91 6.22 5.21 1.68 3.12 表 5 Lasso回归筛选重度DPN预测模型变量的回归系数
Table 5. Lasso regression coefficients for filtering severe DPN prediction model variables
入选变量 年龄 HbA1c 血脂异常 吸烟 TIR Lasso
回归系数0.009706 0.032768 0.252567 0.203794 −0.012917 表 6 重度DPN多因素回归模型相关参数
Table 6. Multivariate regression equation parameter of severe DPN prediction model
参数 B SE Wald OR 95%CI P 年龄 0.0186 0.0111 1.68 1.018 0.954~1.830 0.093 吸烟 0.3725 0.2420 1.54 1.451 0.428~1.107 0.123 血脂异常 0.4497 0.2562 1.76 1.567 0.948~2.590 0.079 HBA1C 0.0774 0.0575 1.35 1.080 0.871~2.098 0.178 TIR −0.0148 0.0055 −2.67 0.985 0.367~0.857 0.007 -
[1] Caroline A Abbott,Rayaz A Malik,Ernest R E van Ross,et al. Prevalence and characteristics of painful diabetic neuropathy in a large community-based diabetic population in the UK[J]. Diabetes Care,2011,34(10):2220-2224. doi: 10.2337/dc11-1108 [2] Nanna B Finnerup,Simon Haroutounian,Peter Kamerman,et al. Neuropathic pain:An updated grading system for research and clinical practice[J]. Pain,2016,157(8):1599-1606. doi: 10.1097/j.pain.0000000000000492 [3] Xu Feng,Zhao Li-Hua,Su Jian-Bin,et al. The relationship between glycemic variability and diabetic peripheral neuropathy in type 2 diabetes with well-controlled HbA1c[J]. Diabetology & Metabolic Syndrome,2014,6(1):139. [4] 中华医学会糖尿病学分会. 中国2型糖尿病防治指南(2020年版)[J]. 中华糖尿病杂志,2021,13(4):315-409. [5] Rodica,Pop-Busui,Andrew J M,et al. Diabetic neuropathy: A position statement by the American Diabetes Association[J]. Diabetes Care,2017,40(1):136-154. doi: 10.2337/dc16-2042 [6] 中国成人血脂异常防治指南修订联合委员会. 中国成人血脂异常防治指南(2016年修订版)[J]. 中华心血管病杂志,2016,44(10):833-853. doi: 10.3760/cma.j.issn.0253-3758.2016.10.005 [7] Vinod P Balachandran,Mithat Gonen,Joshua Smith,et al. Nomograms in oncology:More than meets the eye[J]. The Lancet Oncology,2015,16(4):173-180. doi: 10.1016/S1470-2045(14)71116-7 [8] Liu S,Zheng H,Zhu X,et al. Neutrophil-to-lymphocyte ratio is associated with diabetic peripheral neuropathy in type 2 diabetes patients[J]. Diabetes Res Clin Pract,2017,130(1):90-97. [9] Callaghan B C,Gallagher G,Fridman V,et al. Diabetic neuropathy: What does the future hold?[J]. Diabetologia,2020,63(5):891-897. doi: 10.1007/s00125-020-05085-9 [10] Feldman E L,Callaghan B C,Pop Busui R,et al. Diabetic neuropathy[J]. Nat Rev Dis Primers,2019,5(1):42. doi: 10.1038/s41572-019-0097-9 [11] Clair,Carole,Cohen,Marya J,et al. The effect of cigarette smoking on diabetic peripheral neuropathy: A systematic review and meta-analysis[J]. Journal of General Internal Medicine,2015,30(8):1193-1203. doi: 10.1007/s11606-015-3354-y [12] Hu Yu-Ming,Zhao Li-Hua,Zhang Xiu-Lin,et al. Association of glycaemic variability evaluated by continuous glucose monitoring with diabetic peripheral neuropathy in type 2 diabetic patients[J]. Endocrine,2018,60(2):292-300. doi: 10.1007/s12020-018-1546-z [13] Paul. Mitochondrial dysfunction in diabetic neuropathy: A series of unfortunate metabolic events[J]. Current Diabetes Reports,2015,15(11):89. doi: 10.1007/s11892-015-0671-9 [14] Kristin Ørstavik,Barbara Namer,Roland Schmidt,et al. Abnormal function of C-fibers in patients with diabetic neuropathy[J]. The Journal of Neuroscience:The Official Journal of the Society for Neuroscience,2006,26(44):11287-94. doi: 10.1523/JNEUROSCI.2659-06.2006 [15] Yoshiaki Suzuki,Jun Sato,Minoru Kawanishi,et al. Tissue glucose level modulates the mechanical responses of cutaneous nociceptors in streptozotocin-diabetic rats but not normal rats in vitro[J]. Pain,2002,99(3):475-484. doi: 10.1016/S0304-3959(02)00244-0 [16] Fitzgerald M,Saville B R,Lewis R J. Decision curve analysis[J]. JAMA,2015,313(4):409-410. doi: 10.1001/jama.2015.37 -






 下载:
下载: