Clinical Study of Cervical Spondylotic Myelopathy Treated by Single Door Laminoplasty
-
摘要:
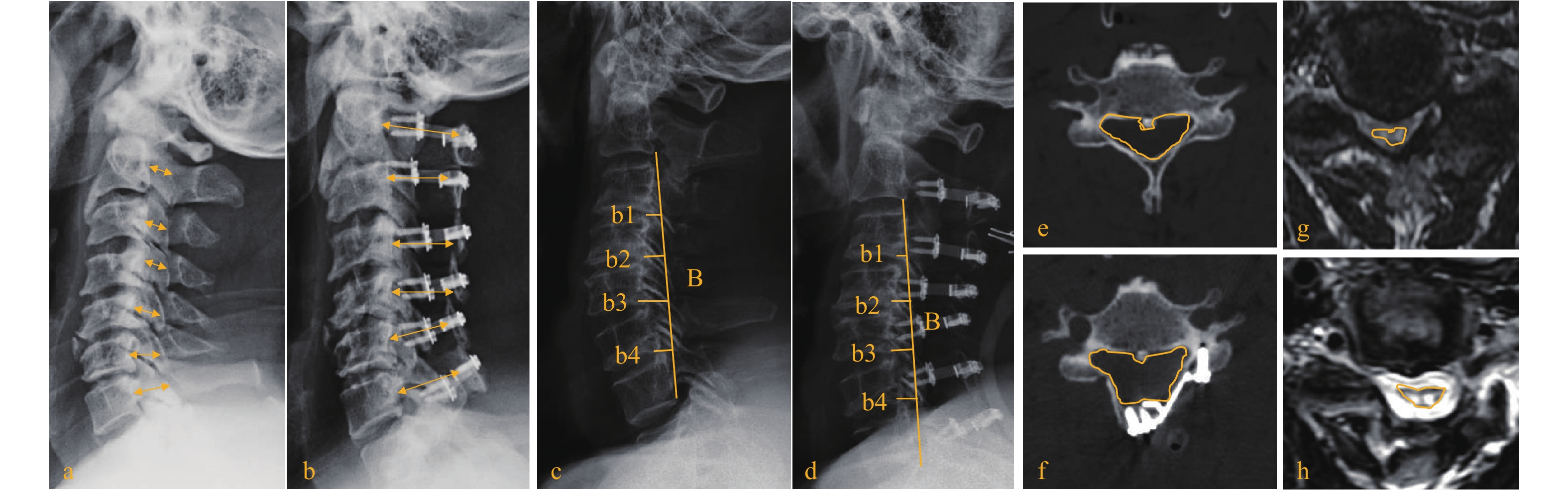
目的 通过分析颈椎单开门成形术术后患者远期临床疗效,探讨颈脊髓面积改变量与患者术后远期临床疗效的相关性。 方法 回顾性分析自2015年11月至2021 年6月期间在海南医学院第一附属医院行颈椎单开门成形术的60例脊髓型颈椎病患者。术后末次随访时采用日本骨科协会(JOA)改善率评估患者远期临床疗效。将末次随访JOA改善率 > 60%的32例患者分为预后良好组,而末次随访JOA改善率≤60%的28例患者分为预后不良组。记录2组患者性别、年龄、症状持续时间、失血量、手术时间、术前及术后JOA评分。并通过术前、术后颈椎MRI、CT及X射线测量椎管矢状面直径、颈椎曲率指数、颈椎活动度、椎管面积及颈脊髓面积。 结果 预后良好组术后颈脊髓面积改变量为(55±41) mm2显著大于预后不良组的(35±37) mm2,2组间差异具有统计学意义(P < 0.05)。此外,预后良好组术前、术后椎管面积及门轴位置均明显大于预后不良组(P < 0.05)。但2组间术前、术后椎管尺状面直径及颈椎活动度的差异无统计学意义(P > 0.05)。而多因素回归分析显示,术前(OR = 6.924,P < 0.05)及术后JOA评分(OR = 22.000,P < 0.05)、术前椎管面积(OR = 2.518,P < 0.05)和颈脊髓面积改变量(OR = 5.513,P < 0.05)与患者末次随访JOA改善率有关。 结论 SDCL术后颈脊髓面积改变量、术前颈椎管面积、及术前术后JOA评分与术后末次随访时JOA改善率密切相关。术者可依据SDCL术后颈脊髓面积改变量预判患者的远期疗效。 Abstract:Objective By analyzing the long term clinical effect of patients after single open-door cervical laminoplasty, the correlation between the change of cervical spinal cord area and the long term clinical effect of patients was discussed. Methods A retrospective analysis was performed on 60 patients with cervical spondylotic myelopathy who underwent cervical single open-door laminoplasty in the First Affiliated Hospital of Hainan Medical College from November 2015 to June 2021. The long-term clinical efficacy was evaluated by Japanese Orthopaedic Association (JOA ) improvement rate at the last follow-up. 32 patients with JOA improvement rate of > 60% at the last follow-up were divided into good prognosis group, while 28 patients with JOA improvement rate of ≤60% at the last follow-up were divided into poor prognosis group. Gender, age, duration of symptoms, blood loss, operation time, preoperative and postoperative JOA score were observed. Spinal canal sagittal diameter, cervical curvature index, cervical range of motion, spinal canal area and cervical spinal cord area were measured by preoperative and postoperative cervical MRI, CT and X-ray. Results The change of cervical spinal cord area in the good prognosis group was (55 ± 41 ) mm2, which was significantly larger than that in the poor prognosis group (35 ± 37 ) mm2, and the difference between the two groups was statistically significant (P < 0.05 ). The preoperative and postoperative spinal canal area and the axial position in the good prognosis group were significantly larger than those in the poor prognosis group (P < 0.05 ). But there was no significant difference in the preoperative and postoperative spinal canal ulnar diameter and cervical activity between the two groups (P > 0.05 ). Multivariate regression analysis showed that preoperative (OR = 6.924, P < 0.05) and postoperative JOA score (OR = 22.000, P < 0.05 ), preoperative spinal canal area (OR = 2.518, P < 0.05 ) and cervical spinal cord area change (OR = 5.513, P < 0.05 ) were related to the improvement rate of JOA at the last follow-up. Conclusion The change of cervical spinal cord area after SDCL, preoperative cervical spinal canal area, and preoperative and postoperative JOA score are closely related to the improvement rate of JOA at the last follow-up. Surgeons can predict the long-term efficacy of the patients according to the change of cervical spinal cord area after SDCL. -
表 1 2组患者基本资料(
$\bar x \pm s $ )Table 1. Basic data of two groups (
$\bar x \pm s $ )项目 预后良好组(n = 32) 预后不良组(n = 28) t/z P 性别(男∶女) 18∶14 15∶13 0.483 0.674 年龄(岁) 63.5 ± 10.2 61.3 ± 8.5 0.329 0.442 术中失血量(mL) 238 ± 155 246 ± 180 −0.378 0.538 手术时间(min) 136 ± 38 141 ± 36 −0.814 0.315 住院时间(d) 9.8 ± 2.6 10.2 ± 3.4 −0.728 0.414 症状持续时间(月) 51.4 ± 74.6 63.8 ± 78.5 2.672 0.061 随访时间(月) 18.8 ± 13.1 17.9 ± 15.4 0.621 0.328 表 2 2 组患者解剖参数变化(
$\bar x \pm s $ )Table 2. Changes in anatomical parameters of the two groups of patients (
$\bar x \pm s $ )项目 预后良好
组(n = 32)预后不良
组(n = 28)t P 门轴位置(宽:窄) 23:9 12:16 0.463 0.001* 椎管直径(cm) 术前 1.67 ± 0.15 1.65 ± 0.16 0.354 0.872 术后 2.54 ± 0.12 2.49 ± 0.18 0.696 0.786 改变量 0.87 ± 0.15 0.84 ± 0.18 0.424 0.374 C2~C7 Cobb(°) 术前 12.3 ± 6.8 13.5 ± 8.4 −0.852 0.682 术后 10.6 ± 7.3 11.8 ± 9.1 −0.744 0.583 改变量 −1.7 ± 7.1 −1.7 ± 8.8 −0.624 0.517 颈椎曲率指数 术前 0.12 ± 0.15 0.11 ± 0.10 0.711 0.632 术后 −0.04 ± 0.07 −0.02 ± 0.06 0.520 0.423 改变量 0.11 ± 0.08 0.09 ± 0.08 0.784 0.566 椎管面积(mm2) 术前 198 ± 33 177 ± 32 0.382 0.030* 术后 348 ± 49 325 ± 47 0.249 0.024* 改变量 150 ± 28 148 ± 27 0.399 0.090 颈椎活动度(°) 术前 43.6 ± 12.7 44.8 ± 13.2 −0.884 0.637 术后 28.1 ± 11.8 31.4 ± 11.9 −0.729 0.516 改变量 −15.5 ± 11.8 −13.4 ± 12.5 0.478 0.361 颈脊髓面积(mm2) 术前 105 ± 49 98 ± 44 0.539 0.422 术后 160 ± 78 133 ± 72 0.473 0.316 改变量 55 ± 41 35 ± 37 0.126 0.001* *P < 0.05。 表 3 2 组间术前术后 JOA 评分变化[(
$\bar x \pm s $ )/%]Table 3. Changes of JOA score between the two groups before and after operation [(
$\bar x \pm s $ )/%]项目 预后良好组
(> 60%,n = 32)预后不良组
(≤60%,n = 28)术前JOA评分 10.3 ± 2.3 8.8 ± 1.5 术后JOA评分 14.5 ± 1.1 12.2 ± 0.8 末次随访JOA评分 16.9 ± 1.4 12.5 ± 1.2 末次随访JOA改善率 64.1 42.0 注:2组内术前、术后JOA评分统计学意义分别为:t1 = 12.252,P1 = 0.007;t2 = 10.537,P2 = 0.011。 表 4 影响患者 JOA 改善率的相关因素
Table 4. Related factors affecting JOA improvement rate of patients
项目 b OR 95%CI P 术前椎管面积 1.035 2.518 1.863~2.020 0.022* 颈脊髓面积改变量 1.868 5.513 1.729~2.105 0.001* 术前JOA评分 2.153 6.924 8.769~9.690 0.001* 术后JOA评分 1.899 22 13.000~13.681 0.001* *P < 0.05。 -
[1] Chen G,Huang W,Jia M,et al. A modified cutting line in the single-door cervical laminoplasty via a computed tomography-based morphological study of the subaxial cervical spine[J]. Clinical Neurology and Neurosurgery,2021,200(1):106384. doi: 10.1016/j.clineuro.2020.106384 [2] Nakashima H,Kato F,Yukawa Y,et al. Comparative effectiveness of open-door laminoplasty versus French-door laminoplasty in cervical compressive myelopathy[J]. Spine,2014,39(8):642-647. doi: 10.1097/BRS.0000000000000252 [3] Hirabayashi K,Watanabe K,Wakano K,et al. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy[J]. Spine,1983,8(7):693-699. doi: 10.1097/00007632-198310000-00003 [4] Hoti Y U D,Aziz A,Ishaque K,et al. Clinical outcome of laminoplasty in cervical myelopathy[J]. Journal of the College of Physicians and Surgeons-pakistan,2018,28(6):466-469. [5] Zhao D W,Fang Z G,Jing D M,et al. Bridging the cervicothoracic junction during posterior cervical laminectomy and fusion for the treatment of multilevel cervical ossification of the posterior longitudinal ligament: a retrospective case series[J]. BMC Musculoskeletal Disorders,2022,23(1):446-446. doi: 10.1186/s12891-022-05417-3 [6] Cheng L,Yunli M,Lei L,et al. Posterior decompression and fusion with vertical pressure procedure in the treatment of multilevel cervical OPLL with kyphotic deformity[J]. Orthopaedic Surgery,2022,14(9):2361-2368. doi: 10.1111/os.13433 [7] 王亚楠,谢梦琦,轩安武,等. 结合K线分析颈椎后纵韧带骨化患者的颈椎活动度与手术预后的关系[J]. 中国骨伤,2018,31(8):6. [8] Nagoshi N,Tsuji O,Okada E,et al. Clinical indicators of surgical outcomes after cervical single open-door laminoplasty assessed by the Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire[J]. Spinal Cord,2019,57(8):644-651. doi: 10.1038/s41393-019-0258-4 [9] Liu G,Fung G,Tan J,et al. A feasibility study of a new muscle sparing “C3 dome-hybrid open-door laminoplasty”: A surgical technique,clinical outcome,and learning curve description[J]. Spine,2020,45(19):E1256-E1263. doi: 10.1097/BRS.0000000000003546 [10] 何伟,钱宇,张军,等. 颈椎退变对外伤性颈髓损伤的影响[J]. 中国骨伤,2012,28(9):737-742. [11] 蒋伟宇,马维虎,顾勇杰,等. 双开门揭盖式椎板分块切除治疗严重颈椎后纵韧带骨化伴颈脊髓损伤[J]. 中国骨伤,2017,30(9):5. [12] Miyazaki M,Ishihara T,Notani N,et al. Relationship of preoperative intramedullary MRI signal intensity and dynamic factors with surgical outcomes of laminoplasty for cervical ossification of the posterior longitudinal ligament[J]. Clinical Neurology and Neurosurgery,2018,174(9):117-122. doi: 10.1016/j.clineuro.2018.09.018 [13] Takeuchi K,Yokoyama T,Wada K,et al. Relationship between enlargement of the cross-sectional area of the dural sac and neurological improvements after cervical laminoplasty: differences between cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament[J]. Spine Surgery and Related Research,2019,3(1):27-36. doi: 10.22603/ssrr.2018-0008 [14] Hirabayashi K J M. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament.[J]. Spine,1981,6(4):354-364. doi: 10.1097/00007632-198107000-00005 [15] Nishida N,Kanchiku T,Imajo Y,et al. Stress analysis of the cervical spinal cord: Impact of the morphology of spinal cord segments on stress[J]. The Journal of Spinal Cord Medicine,2016,39(3):327-334. doi: 10.1179/2045772315Y.0000000012 [16] Mizutani M,Fujishiro T,Obo T,et al. Impact of morphological restoration of the spinal cord from the preoperative to early postoperative periods on C5 palsy development[J]. Journal of Neurosurgery:Spine,2021,35(5):624-632. doi: 10.3171/2021.2.SPINE201955 [17] Wu W,Yang Z,Zhang T,et al. Microstructural changes in compressed cervical spinal cord are consistent with clinical symptoms and symptom duration[J]. Spine,2020,45(16):E999-E1005. doi: 10.1097/BRS.0000000000003480 [18] Houten J K,Cooper P R. Laminectomy and posterior cervical plating for multilevel cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament: effects on cervical alignment,spinal cord compression,and neurological outcome[J]. Neurosurgery,2003,52(5):1081-1088. [19] 方明,陆建猛,王兴武,等. C3扩大半椎板切除单开门椎板成形术治疗多节段颈脊髓压迫症[J]. 中国骨伤,2020,33(8):6. [20] Yuan W,Zhu Y,Liu X,et al. Postoperative three-dimensional cervical range of motion and neurological outcomes in patients with cervical ossification of the posterior longitudinal ligament: cervical laminoplasty versus laminectomy with fusion[J]. Clinical Neurology and Neurosurgery,2015,134:17-23. doi: 10.1016/j.clineuro.2015.04.004 [21] Zhang K,Yang Y,Liu H,et al. Is there any correlation between the recovery rate of JOA and the increasing of cervical spinal cord area after single-door cervical laminoplasty?[J]. Clinical Neurology and Neurosurgery,2022,213:107103. doi: 10.1016/j.clineuro.2021.107103 [22] Hou Y,Liang L,Shi G D,et al. Comparing effects of cervical anterior approach and laminoplasty in surgical management of cervical ossification of posterior longitudinal ligament by a prospective nonrandomized controlled study[J]. Orthopaedics & Traumatology:Surgery & Research,2017,103(5):733-740. [23] Zhang K,Yang Y,Liu H,et al. Multivariate analysis of factors associated with spinal cord area in single-door cervical laminoplasty with miniplate fixation[J]. BMC Musculoskeletal Disorders,2021,22(1):1-9. doi: 10.1186/s12891-020-03840-y [24] Takahashi Y,Narusawa K,Shimizu K,et al. Enlargement of cervical spinal cord correlates with improvement of motor function in upper extremities after laminoplasty for cervical myelopathy[J]. Clinical Spine Surgery,2006,19(3):194-198. [25] Zhao Y,Cheng C,Chen H,et al. Limited laminectomy and foraminal decompression combined with internal fixation for treating multi-segment cervical spondylotic myelopathy: Does it effectively improve neurological function and prevent C5 palsy?[J]. Medicine,2018,97(47):e13327. doi: 10.1097/MD.0000000000013327 [26] Yang L,Gu Y,Shi J,et al. Modified plate-only open-door laminoplasty versus laminectomy and fusion for the treatment of cervical stenotic myelopathy[J]. Orthopedics,2013,36(1):e79-e87. [27] Subramaniam V,Chamberlain R H,Theodore N,et al. Biomechanical effects of laminoplasty versus laminectomy: stenosis and stability[J]. Spine,2009,34(16):E573-E578. [28] Li Z,Xue Y,He D,et al. Extensive laminectomy for multilevel cervical stenosis with ligamentum flavum hypertrophy: more than 10 years follow-up[J]. European Spine Journal,2015,24:1605-1612. [29] Hamburger C,Büttner A,Uhl E. The cross-sectional area of the cervical spinal canal in patients with cervical spondylotic myelopathy: correlation of preoperative and postoperative area with clinical symptoms[J]. Spine,1997,22(17):1990-1994. doi: 10.1097/00007632-199709010-00009 -






 下载:
下载: