Value of Transesophageal Three-dimensional Echocardiography in Diagnosis of Perivalvular Leakage after Aortic Valve Replacement
-
摘要:
目的 探讨经食管三维超声(RT-3D-TEE)对主动脉瓣置换术后瓣周漏评估的临床意义。 方法 选取北华大学附属医院2015年1月至2018年12月收治的主动脉瓣置换术后疑似瓣周漏患者70例,均接受二维经胸超声心动图(2D-TTE)检查和RT-3D-TEE检查,比较2D-TTE与RT-3D-TEE检查对主动脉瓣置换术后瓣周漏的诊断、破口位置和范围及瓣周其他情况评估的差异。90例患者均再次接受手术治疗。 结果 70例患者中,经术中观察确诊瓣周漏45例,非瓣周漏25例。2D-TTE诊断正确52例(诊断为瓣周漏36例,含6例疑似诊断),误诊9例,漏诊9例,RT-3D-TEE诊断正确70例(诊断为瓣周漏45例,含3例疑似诊断),RT-3D-TEE的诊断准确率(100.0%)高于2D-TTE(74.29%),差异有统计学意义(P < 0.05)。2D-TTE诊断的36例瓣周漏中,破口位于左冠瓣区5例,右冠瓣区8例,多个破口或破口面积超过单个瓣叶区域11例,其余12例分区不明确,在RT-3D-TEE诊断的45例瓣周漏中,破口位于左冠瓣区9例,右冠瓣区15例,多个破口或破口面积超过单个瓣叶区域18例,其余3例分区不明确,经手术证实,RT-3D-TEE诊断的漏口位置与范围与术中观察基本一致。术中发现,9例患者合并瓣环部分脱位,6例合并瓣周脓肿,3例合并二尖瓣机械瓣卡瓣,RT-3D-TEE全部诊断正确,2D-TTE正确诊断合并瓣环部分脱位6例,合并瓣周脓肿3例,漏诊合并二尖瓣机械瓣卡瓣3例。2种检查方法在测量瓣周漏破口的长度和宽度方面,差异无统计学意义(P > 0.05)。RT-3D-TEE对合并有瓣环脱位、瓣周脓肿、二尖瓣卡瓣的诊断准确度高于2D-TTE。 结论 RT-3D-TEE因其观察位置的特殊性表现出对人工瓣膜整体观图像上的优势,是对2D-TTE诊断主动脉瓣置换术后瓣周漏的良好补充。 -
关键词:
- 人工主动脉瓣置换术 /
- 瓣周漏 /
- 经食管三维超声心动图
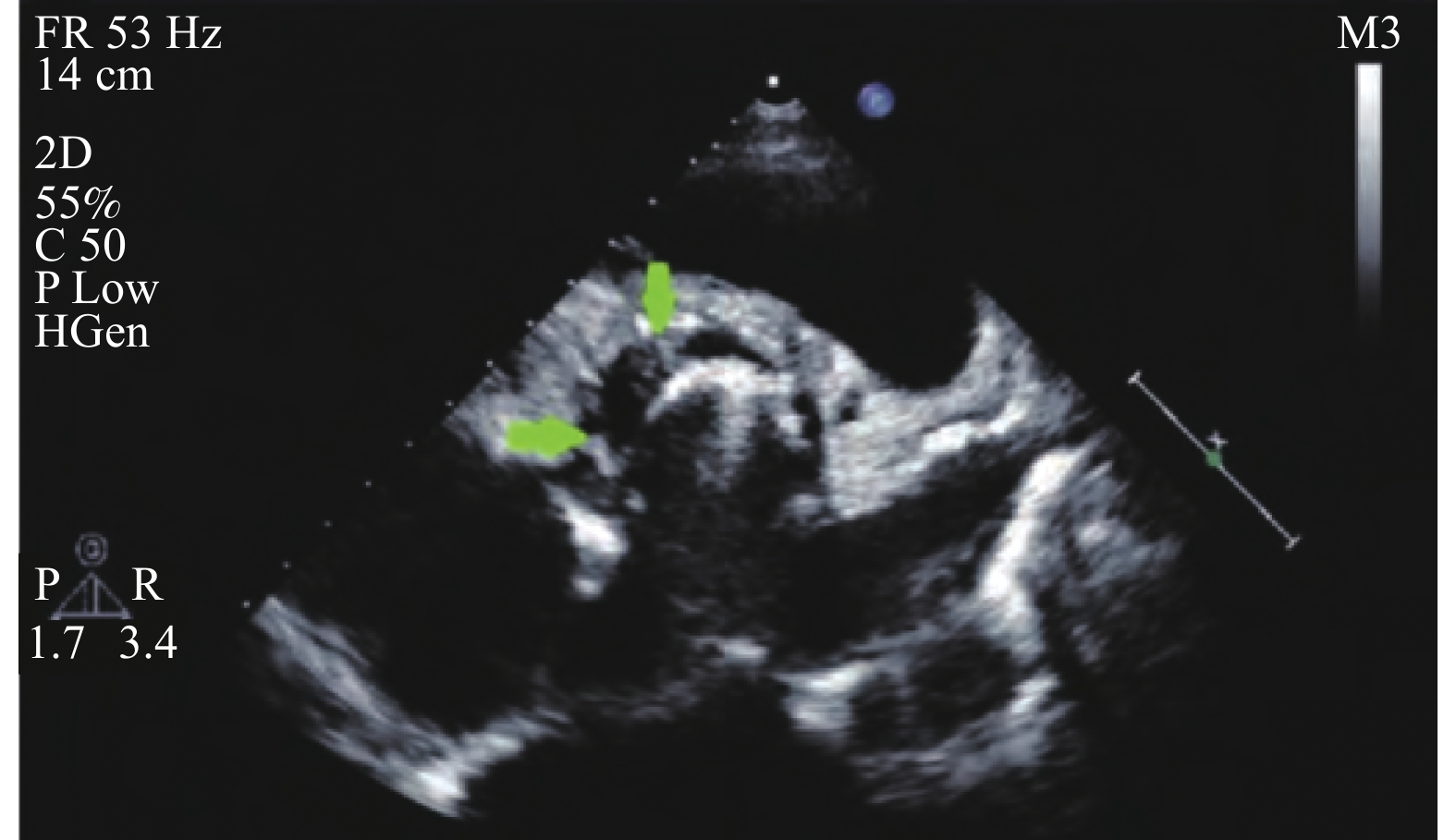
Abstract:Objective To explore the clinical value of transesophageal three-dimensional echocardiography (RT-3D-TEE) in the diagnosis of perivalvular leakage after aortic valve replacement. Methods 70 patients with suspectde perivalvular leak after aortic valve replacement in our hospital from January 2015 to December 2018 were selected.All patients underwent 2-D transthoracic echocardiography (2D-TTE) and RT-3D-TEE was compared. The accuracy of the two methods in the diagnosis of perivalvular leakage after aortic valve replacement, and the location, range and other conditions of perivalvular leakage were compared. All 70 patients underwent surgery again. Results After surgical treatment, 45 cases of perivalvular leakage and 25 cases of non-perivalvular leakage were confirmed.2D-TTE was diagnosed correctly in 52 cases, misdiagnosed in 9 case and missed in 9 cases. RT-3D-TEE was diagnosed correctly in 70 cases. The diagnostic accuracy of RT-3D-TEE (100.0%) was higher than that of 2D-TTE (80.0%), and the difference was statistically significant (P < 0.05). Among the 36 cases of perivalvular leakage diagnosed by 2D-TTE, 5 were located in the left coronary valve region, 8 were located in the right coronary valve region, 11 had multiple or larger than a single lobe region, and the remaining 12 cases could not be clearly identified. Among the 45 cases of perivalvular leakage diagnosed by RT-3D-TEE, 9 cases were located in the left coronary valve region, 15 cases were located in the right coronary valve region, 18 cases had multiple or larger than a single lobe region, and the remaining 3 cases could not be clearly identified. The location and scope of leakage in the diagnosis of RT-3D-TEE were basically consistent with the intraoperative observation.RT-3D-TEE diagnosed 9 patients with partial flap ring dislocation, 6 patients with perivalvular abscess, and 3 patients with mechanical mitral valve sticking, which was consistent with the intraoperative observation. 2D-TTE diagnosed 6 patients with partial flap ring dislocation, 3 patients with perivalvular abscess and 3 patients with mechanical mitral valve sticking were misdiagnosed.There was no significant difference in the length and width of perivalvular leakage between the two methods (P > 0.05). The diagnostic accuracy of RT-3D-TEE was higher than that of 2D-TTE in the diagnosis of ring dislocation, perivalvular abscess and mechanical mitral valve valves. Conclusion RT-3D-TEE is a good complement to 2D-TTE in the diagnosis of perivalvular leakage after aortic valve replacement because of its superiority in the overall image of prosthetic valve because of its special observation position. -
表 1 患者一般资料
Table 1. General information of patients
项目 临床特征 n 构成比(%) 原发疾病 风湿性心脏病 45 64.29 先天性心脏病 8 11.43 瓣膜退行性变 7 10 感染性心内膜炎 10 14.28 人工主动脉瓣类型 机械瓣 52 74.29 生物瓣 18 25.71 首次换瓣至本次
入院时间间隔<1 a 21 30 1~5 a 15 21.43 >5 a 34 48.57 本次就诊症状 呼吸困难 44 62.86 活动后心悸 65 92.86 心绞痛 38 54.29 发热 15 21.43 贫血 10 14.29 手术方式 瓣周漏修补术 57 81.43 二次换瓣术 13 18.57 表 2 2D-TTE与RT-3D-TEE测量瓣周漏破口大小比较[(
$\bar x \pm s $ ),mm]Table 2. Comparison of perivalvular leak size measured by 2D-TTE and RT-3D-TEE [(
$\bar x \pm s $ ),mm]检查方法 例数(破口数) 破口长度 破口宽度 2D-TTE 24(37) 5.8 ± 0.9 4.7 ± 0.6 RT-3D-TEE 24(37) 5.6 ± 0.7 4.5 ± 0.7 t 1.067 0.152 P 0.290 0.191 -
[1] 晋军. 经导管主动脉瓣置换术的临床研究和应用进展[J]. 第三军医大学学报,2019,41(19):1873-1880. [2] 左鹏飞,李亚峰,顿国亮. RT-3D-TEE诊断二尖瓣瓣膜置换术后PVL的价值分析[J]. 西南国防医药,2018,28(12):1207-1209. [3] Volkmar F,Helmut B,Jeroen J B,et al. ESC/EACTS Guidelines for the management of valvular heart disease: The task force for the management of valvular heart disease of the european society of cardiology (ESC) and the european association for cardio-thoracic surgery (EACTS)[J]. European Journal of Cardio-thoracic Surgery,2017,52(4):832. doi: 10.1093/ejcts/ezx363 [4] 高润霖. 中国心瓣膜病现状[J]. 华西医学,2018,33(2):127-131. [5] Gursoy O M,Astarcioglu M A,Gokdeniz T,et al. Severe mitral paravalvular leakage: echo-morphologic description of 47 patients from real-time three-dimensional transesophageal echocardiography perspective[J]. The Anatolian Journal of Cardiology,2013,13(7):633-640. [6] 周文君,柳梅,尚小珂,等. 介入封堵和外科手术治疗二尖瓣置换术后瓣周漏的临床对比研究[J]. 中国介入心脏病学杂志,2018,26(9):504-509. [7] 科雨彤,安博静,蒲俊舟,等. 经食道三维超声心动图对指导心外科术后吻合口漏介入封堵的价值[J]. 中国超声医学杂志,2019,35(9):788-792. [8] Suh Y J,Hong G R,Han K,et al. Assessment of mitral paravalvular leakage after mitral valve replacement using cardiac computed tomography: comparison with surgical findings[J]. Circulation Cardiovascular Imaging,2016,9(6):e004153. doi: 10.1161/CIRCIMAGING.115.004153 [9] Ruiz C E,Hahn R T,Berrebi A,et al. Clinical trial principles and endpoint definitions for paravalvular leaks in surgical prosthesis: An expert statement[J]. European Heart Journal,2017,65(16):2067-2087. [10] 李兴文,吴丽萍. 经食管三维超声对二尖瓣瓣膜置换术后瓣周漏的临床诊断意义[J]. 牡丹江医学院学报,2018,39(1):21-23. [11] 万俊义,张浩,张戈军,等. 介入治疗二尖瓣置换术后瓣周漏的疗效分析[J]. 中国循环杂志,2019,34(11):1074-1078. [12] 赵星,王浩,高一鸣,等. 主动脉瓣置换术后瓣周漏的临床及超声心动图分析[J]. 中国循环杂志,2018,33(5):485-489. [13] Kliger C,Eiros R,Isasti G,et al. Review of surgical prosthetic paravalvular leaks: diagnosis and catheter-based closure[J]. European Heart Journal,2013,34(9):638-649. doi: 10.1093/eurheartj/ehs347 [14] 蒲俊舟,吴文辉,黄连军. 应用Ⅲ型血管塞封堵二尖瓣瓣周漏1例[J]. 中国介入心脏病学杂志,2018,26(6):355-356. [15] Krishnaswamy A,Kapadia S R,Tuzcu E M. Percutaneous paravalvular leak closure-imaging,techniques and outcomes[J]. Circulation Journal,2013,77(1):19-27. doi: 10.1253/circj.CJ-12-1433 [16] 王瑶,张永庆,路蓉. 经食管三维超声心动图对二尖瓣反流与二尖瓣复合体构型及左房功能变化间的关系研究[J]. 中国超声医学杂志,2018,34(8):696-700. doi: 10.3969/j.issn.1002-0101.2018.08.008 [17] Gafoor S,Steinberg D H,Franke J,et al. Tools and techniques-clinical:paravalvular leak closure[J]. Euro Intervention,2014,9(11):1359-1363. doi: 10.4244/EIJV9I11A227 -






 下载:
下载: