Correlation between DDAH1 Gene 836A/T Polymorphism and Type 2 Diabetic Kidney Disease in Yunnan Han Population
-
摘要:
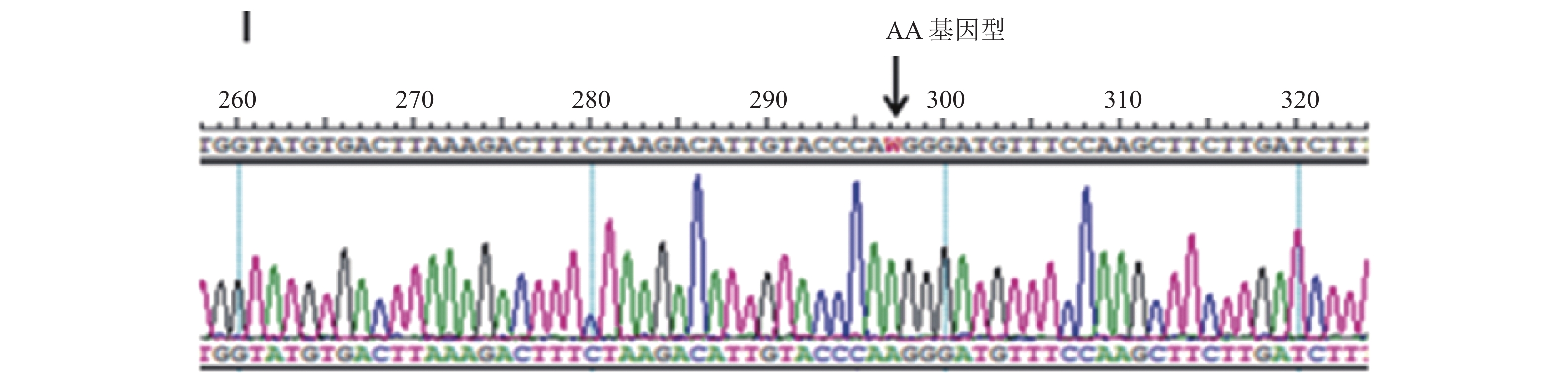
目的 探讨DDAH1基因836A/T多态性与云南地区汉族人群2型糖尿病肾脏疾病发生的相关性。 方法 选取T2DM患者共660例,根据UACR检测结果,将患者分为3组:单纯2型糖尿病组(DN0组),合并早期肾病组(DN1组),合并临床期肾病组(DN2组)。 健康人群(NC组)304例。采用PCR-DNA测序技术对DDAH1基因836A/T多态性进行基因分型,ELISA 法检测血浆非对称性二甲基精氨酸(ADMA)浓度。 结果 DDAH1基因836位点AA基因型在DN1 + DN2组的分布频率高于DN0组 (P < 0.05)。A等位基因在DN1 + DN2组的分布频率高于DN0组 (P < 0.05)。T2DM患者中AA基因型携带者较AT+TT基因型个体具有更高的ADMA水平。ADMA水平在DN1 + DN2组高于DN0组(P < 0.05)。通过相关危险因素分析发现, 在T2DM患者中ADMA水平、DDAH1基因836位点AA基因型是发生DKD的危险因素。 结论 DDAH1基因836位点AA基因型可能是云南地区汉族T2DM 患者发生DKD的危险因素,AA基因型携带者ADMA水平升高。 Abstract:objective To investigate the association between DDAH1 gene 836A/T polymorphism and type 2 diabetic kidney disease (DKD) in Yunnan Han population. Methods A total of 660 patients with T2DM were included. Patients were divided into three groups based on UACR results: simple type 2 diabetes mellitus group (DN0 group), complicated with early nephropathy group (DN1 group), and complicated with clinical nephropathy group (DN2 group). A total of 304 healthy people were included as normal control group (NC group). The genotype of DDAH1 gene 836A/T polymorphism was determined by PCR-DNA sequencing. The plasma asymmetric dimethylarginine (ADMA)concentration was measured by ELISA. Results The distribution frequency of AA genotype and allele A at the 836 locus of DDAH1 gene in the DN1+DN2 group was significantly higher than those in the DN0 group (P < 0.05). AA genotype carriers have higher ADMA levels than AT+TT genotype individuals in T2DM patients. The level of ADMA in DN1+DN2 group was higher than that in DN0 group (P < 0.05). Logistic regression analysis showed that ADMA level and DDAH1 gene 836 AA genotype were risk factors for DKD in T2DM patients. Conclusions The DDAH1 gene 836 AA genotype may be a risk factor for diabetic kidney disease in T2DM patients of Han nationality in Yunnan Province, and patients with this genotype have higher ADMA levels. -
Key words:
- Type 2 diabetes mellitus /
- diabetic kidney disease /
- DDAH1 /
- ADMA /
- Genetic polymorphism
-
表 1 PCR引物序列
Table 1. PCR primer sequences
基因多态性位点 上游引物序列 下游引物序列 DDAH1基因836A/T 5′- TGGTCTCCTCTGCCTCTGAC -3′ 5′-GGTGATCGCTTCCTGAACAT-3′ 表 2 各组间临床资料比较(
$\bar x \pm s $ )Table 2. Comparison of clinical data of each group (
$\bar x \pm s $ )指标 NC DN0 DN1 DN2 DN1+DN2 F P 年龄(岁) 54.62 ± 10.58 54.64 ± 10.73 55.75 ± 10.42 57.28 ± 11.67 56.36 ± 11.36 2.758 0.13 病程(月) − 72.13 ± 25.09 92.23 ± 43.62△ 109.18 ± 45.69△▲ 100.24 ± 51.46△▲ 9.364 < 0.001 收缩压(mmHg) 117.59 ± 13.26 122.64 ± 16.72 133.52 ± 18.54*△ 142.65 ± 21.17*△#▲ 138.83 ± 19.82*△ 11.5 < 0.001 舒张压(mmHg) 77.15 ± 7.63 78.25 ± 10.02 82.42 ± 11.54 81.76 ± 12.22 82.05 ± 12.09 0.831 0.598 血肌酐(mmol/L) 63.2 ± 18.55 65.7 ± 18.25 69.43 ± 19.43* 79.17 ± 24.64*△# 73.76 ± 26.78* 15.684 < 0.001 尿酸(mmol/L) 337.36 ± 87.62 337.89 ± 86.72 335.58 ± 104.05 354.32 ± 102.91*△# 346.62 ± 103.42 7.275 < 0.001 TC(mmol/L) 4.39 ± 1.07 4.38 ± 1.25 4.51 ± 1.34 4.43 ± 1.27 4.49 ± 1.33 1.26 0.289 TG (mmol/L) 1.25 ± 0.98 2.63 ± 1.42* 2.67 ± 1.78* 2.31 ± 1.45* 2.52 ± 1.79* 10.24 < 0.001 HLD(mmol/L) 1.29 ± 0.34 1.03 ± 0.35 1.01 ± 0.29 0.98 ± 0.75 1.00 ± 0.31 0.75 0.52 LDL (mmol/L) 2.52 ± 1.22 2.58 ± 1.52 2.83 ± 2.14*△ 2.79 ± 1.86*△ 2.82 ± 1.75*△ 5.19 0.002 HbA1C (%) 6.17 ± 2.25 8.50 ± 2.12* 8.57 ± 2.06* 8.66 ± 2.63* 8.61 ± 2.05* 11.04 < 0.001 ADMA (μmol/L) 0.62 ± 0.23 1.06 ± 0.27* 1.23 ± 0.42*△ 1.29 ± 0.53*△ 1.27 ± 0.41*△▲ 12.424 < 0.001 与NC组比较,* P < 0.05;与DN0组比较,△P < 0.05;与DN1组比较,#P < 0.05;协方差分析,▲P < 0.05。 表 3 各组间基因型频率和等位基因频率[n(%)](1)
Table 3. The genotype and allele frequencies in each group [n(%)](1)
组别 n 基因型 χ2 P AA AT+TT NC组 304 128(42.1) 176(57.9) 11.863 0.013 DN0组 296 146(49.6)* 150(50.4) DN1组 190 112(58.9)* 78(41.1) DN2组 174 98(56.3)*# 76(43.7) DN1+DN2组 364 210(57.7)*# 154(42.3) 与NC组比较,*P < 0.05;与DN0组比较,#P < 0.05。 表 3 各组间基因型频率和等位基因频率[n(%)](2)
Table 3. The genotype and allele frequencies in each group [n(%)](2)
组别 n 等位基因 χ2 P A T NC组 304 398 (65.5) 210(34.5) 19.318 0.001 DN0组 296 416(70.3)* 176(29.7) DN1组 190 290(76.3)* 90(23.7) DN2组 174 262(75.3)*# 86(24.7) DN1+DN2组 364 552(75.8)*# 176(24.2) 与NC组比较,*P < 0.05;与DN0组比较,#P < 0.05。 表 4 T2DM患者中不同基因型间临床资料比较(
$\bar x \pm s $ )(1)Table 4. Comparison of clinical data of DDAH1 genotype of T2DM patients (
$\bar x \pm s $ )(1)基因型 收缩压(mmHg) 舒张压(mmHg) 血肌酐(mmol/L) 尿酸(mmol/L) TC(mmol/L) AA 130.26 ± 17.43 79.53 ± 9.76 74.62 ± 23.64 344.41 ± 103.42 4.48 ± 1.04 AT+TT 129.82 ± 17.84 78.05 ± 10.62 72.58 ± 21.93 338.51 ± 91.45 4.38 ± 126 表 4 T2DM患者中不同基因型间临床资料比较(
$\bar x \pm s $ )(2)Table 4. Comparison of clinical data of DDAH1 genotype of T2DM patients (
$\bar x \pm s $ )(2)基因型 收缩压(mmHg) 舒张压(mmHg) 血肌酐(mmol/L) 尿酸(mmol/L) TC(mmol/L) AA 2.50 ± 1.42 1.06 ± 0.27 2.92 ± 1.68 9.12 ± 2.21 1.39 ± 0.34 AT+TT 2.57 ± 1.82 1.01 ± 0.33 2.85 ± 1.74 8.71 ± 2.08 1.09 ± 0.27 * 2组间比较,*P < 0.05。 表 5 T2DM-DKD发生的危险因素的Logistic分析
Table 5. Logistic regression analysis of T2DM-DKD occurence
进入回归方程的变量 B S.E. Wald P OR OR值的95%CI 下限 上限 病程(月)) 0.821 0.476 5.365 0.021 1.103 1.152 3.275 ADMA(μmol/L) 1.374 0.602 5.473 0.029 3.973 1.228 10.876 AA基因型 1.538 0.452 10.384 0.001 4.421 1.734 9.326 表 6 T2DM-DKD发展的危险因素的Logistic分析
Table 6. Logistic regression analysis of T2DM-DKD development
进入回归方程的变量 B S.E. Wald P OR OR值的95%CI 下限 上限 病程(月) 0.862 0.368 11.178 0.001 2.410 1.476 4.632 SBP(mmHg) 1.423 0.574 6.692 0.023 4.335 1.431 12.795 -
[1] American Diabetes Association Professional Practice Committee. Classification and diagnosis of diabetes: Standards of medical care in diabetes-2022. Amer diabet assoc professional pra jan 2022[J]. Diabetes Care,2022,45(9):S17-S38. [2] Alhaider A A,Korashy H M,Sayed-Ahmed M M,et al. Metformin attenuates streptozotocin-induced diabetic nephropathy in rats through modulation of oxidative stress genes expression[J]. Chem Biol Interact,2011,192(3):233-242. doi: 10.1016/j.cbi.2011.03.014 [3] Michael D W,Ting G,Kristen S,et al. Enhancing kidney DDAH-1 expression by adenovirus delivery reduces ADMA and ameliorates diabetic nephropathy[J]. America Journal Of Physiology-Renal Physiology,2020,318(2):509-517. doi: 10.1152/ajprenal.00518.2019 [4] Mannino G C,Pezzilli S,Averta C,et al. A functional variant of the dimethylarginine dimethylaminohydrolase-2 gene is associated with myocardial infarction in type 2 diabetic patients[J]. Cardiovasc Diabetol.,2019,18(1):102. doi: 10.1186/s12933-019-0906-1 [5] Rhys D. Fogarty,Sotoodeh Abhary,Shahrbanou Javadiyan,et al. Rlationship between DDAH gene variants and serum a ADMA level in individuals with type 1 diabetes[J]. Diabetes Complications,2012,26(3):195-198. doi: 10.1016/j.jdiacomp.2012.03.022 [6] 中华医学会糖尿病学分会. 中国2型糖尿病防治指南(2017年版)[J]. 中华糖尿病杂志,2018,10(1):4-67. doi: 10.3760/cma.j.issn.1674-5809.2018.01.003 [7] 石柔,张娴,谭洪,等. 云南地区汉族2型糖尿病患者二甲基精氨酸二甲胺水解酶1、二甲基精氨酸二甲胺水解酶2基因单核苷酸多态性与动脉粥样硬化关系的研究[J]. 中国糖尿病杂志,2021,29(5):321-327. doi: 10.3969/j.issn.1006-6187.2021.05.001 [8] Dagar N,Das P,Bisht P,et al. Diabetic nephropathy: A twisted thread to unravel[J]. Life Sciences,2021,278(8):119635. [9] Creager M A,Luscher T F,Cosentino F,et al. Diabetes and vascular disease: pathophysiology,clinical consequences,and medical therapy: Part I[J]. Circulation,2003,108(12):1527-1532. doi: 10.1161/01.CIR.0000091257.27563.32 [10] Wieczor R,Wieczor A M,Rosc D J,et al. ADMA (asymmetric dimethylarginine) and angiogenic potential in patients with type 2 diabetes and prediabetes[J]. Experimental Biology and Medicine,2020,246(2):153-162. [11] Mihout F,Shweke N,N Big´e,et al. Asymmetric dimethylarginine(ADMA) induces chronic kidney disease through a mechanism involving collagen and TGF-β1 synthesis[J]. The Journal of Pathology,2011,223(1):37-45. doi: 10.1002/path.2769 [12] Mei Rong D,Gui Xia J,Nian Sheng L,et al. Role of Asymmetrical Dimethyl- arginine in Diabetic Microvascular Complications[J]. Journal of Cardiovascular Pharmacology,2016,68(4):322-326. doi: 10.1097/FJC.0000000000000414 [13] Jing L,Caiying L,Wen C,et al. Relationship between serum asymmetric dimethylarginine level and microvascular complications in diabetes mellitus:A meta-analysis[J]. BioMed Research International,2019,2019:2941861. [14] Isaivani J,Saravanakumar S,Prabu P,et al. Association of circulatory asymmetric dimethylarginine (ADMA) with diabetic nephropathy in Asian Indians and its causative role in renal cell injury[J]. Clinical Biochemistry,2017,50(15):835-842. doi: 10.1016/j.clinbiochem.2017.05.007 [15] Hu X,Atzler D,Xu X,et al. Dimethylarginine dimethylaminoh ydrolase-1 is the critical enzyme for degrading the cardiovascular risk factor asymmetrical dimethylarginine[J]. Arterioscler Thromb Vasc Biol,2011,31(1):1540-1546. [16] Roman N R,Natalia J,Alfred S,et al. ADMA elevation does not exacerbate development of diabetic nephropathy in mice with streptozotocin-induced diabetes mellitus[J]. Atherosclerosis Supplements,2019,30:319-325. [17] Shi L L,Zhao C Y,Wang H Y,et al. Dimethylarginine dimethylamin ohydrolase 1 deficiency induces the epithelial to mesenchymal transition in renal proximal tubular epithelial cells and exacerbates kidney damage in aged and diabetic mice[J]. Antioxidants & Redox Signaling,2017,27(16):1347-1360. [18] Abhary S,Burdon K P,Kuot A,et al. Sequence variation in DDAH1 and DDAH2 genes is strongly and additively associated with serum ADMA concentrations in individuals with Type 2 diabetes[J]. Plos One,2010,5(3):e9462. doi: 10.1371/journal.pone.0009462 [19] Lind L,Ingelsson E,Kumar J,et al. Genetic variation in the dimethylarginine dimethylaminohydrolase 1 gene (DDAH1) is related to asymmetric dimethylarginine (ADMA) levels,but not to endothelium-dependent vasodilation[J]. Vascular Medicine,2013,18(4):192-199. doi: 10.1177/1358863X13496488 [20] JHannemann J,Zummack J,Hillig J,et al. Association of variability in the DDAH1,DDAH2,AGXT2 and PRMT1 genes with circulating ADMA concentration in human whole blood[J]. Journal of Clinical Medicine,2022,11(4):941. doi: 10.3390/jcm11040941 [21] Zhu F S,Zhou C,Wen Z,et al. DDAH1 promoter -396 4N insertion variant is associated with increased risk of type 2 diabetes in a gender‐dependent manner[J]. Molecular Genetics & Genomic Medicine,2020,8(1):e1011. [22] Wang S Y,Deng Z X,Zhang H,et al. The effect of haptoglobin genotype on the association of asymmetric dimethylarginine and DDAH 1 polymorphism with diabetic macroangiopathy[J]. Cardiovascular Diabetology,2022,21:265. doi: 10.1186/s12933-022-01702-6 -






 下载:
下载: