Analysis of Prognostic Risk Factors in Patients with Septic Shock Based on Circulatory and Cellular Immune Response Indicators
-
摘要:
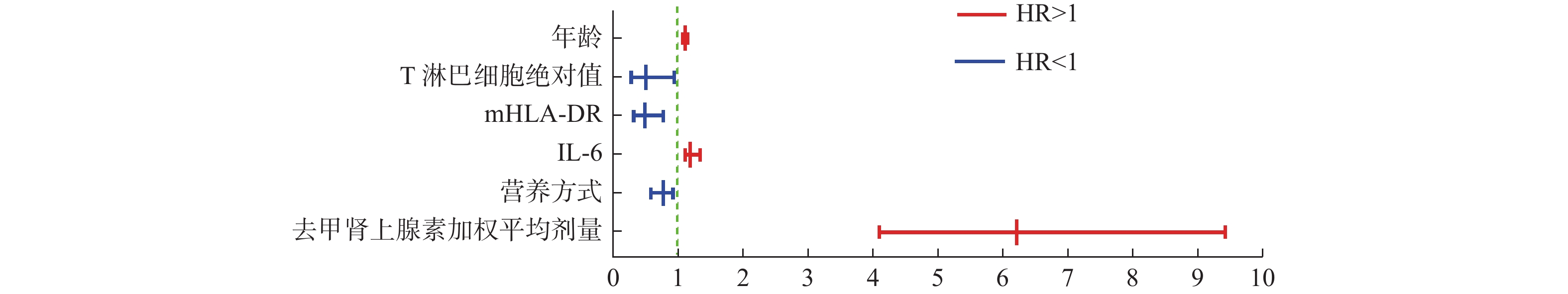
目的 探讨脓毒性休克患者预后风险因素,以循环和细胞免疫效应指标为基础,精准调控去甲肾上腺素剂量,减轻免疫功能抑制,提高脓毒性休克救治成功率。 方法 研究为回顾性队列研究。依据纳入和排除标准收集昆明医科大学第一附属医院ICU 2021年5月至2022年12月期间救治的脓毒性休克患者病例资料160例,均给予标准集束化治疗。同时根据脓毒性休克患者28 d生存结局情况分为死亡组(n = 89)和生存组(n = 71),统计2组患者入院24 h内基线资料、检验指标、去甲肾上腺素加权平均剂量、血气分析、微循环指标、细胞免疫以及早期72 h内的临床综合治疗数据,通过单因素分析判断出有意义的指标,并应用多因素COX比例风险回归模型分析,筛选出影响脓毒性休克患者预后的独立风险因素。 结果 多因素COX模型回归分析结果显示:年龄(HR = 1.05,95%CI:1.09~1.12,P = 0.036)、营养方式(HR = 0.74,95%CI:0.56~0.90,P = 0.037)、去甲肾上腺素加权平均剂量(HR = 6.21,95%CI:4.09~9.43,P < 0.001)、IL-6(HR = 1.16,95%CI:1.09~1.31,P = 0.012)、T淋巴细胞绝对值(HR = 0.47,95%CI:0.24~0.91,P = 0.025)、mHLA-DR(HR = 0.46,95%CI:0.28~0.75,P = 0.002)6个因素为影响脓毒性休克患者预后的独立风险因素,以可视化森林图呈现。 结论 年龄、去甲肾上腺素加权平均剂量、IL-6是影响脓毒性休克患者预后的危险因素,风险比均大于1。营养方式、T淋巴细胞绝对值、mHLA-DR是影响脓毒性休克患者预后的保护因素,风险比均小于1。 Abstract:Objective To investigate the prognostic risk factors of patients with septic shock based on circulatory and cellular immune effects, to accurately regulate the noradrenaline dose, alleviate immune function suppression, and improve the success rate of septic shock treatment. Methods This is an observational, retrospective, cohort study. According to the inclusion and exculusion criteria, 160 patients with septic shock treated in ICU of the first affiliated hospital of Kunming medical university from May 2021 to December 2022 were collected, and all of them were given standard cluster treatment. At the same time, according to 28d survival outcome in patients with septic shock was divided into death group (n = 89) and survival group (n = 71), statistics of two groups of patients admitted to the hospital within 24h baseline data, test indicators, the weighted average dose of noradrenaline, blood gas index, microcirculation index, cellular immunity and early treatment of clinical data in 72h. Meaningful indicators were identified by single-factor analysis, and a multivariate COX proportional risk regression model was applied to screen out independent risk factors affecting the prognosis of patients with septic shock. Results Multivariate COX regression model analysis results showed that: age (HR = 1.05, 95%CI: 1.09~1.12, P = 0.036), nutritional mode (HR = 0.74, 95%CI: 0.56~0.90, P = 0.037), the weighted average dose of norepinephrine (HR = 6.21, 95%CI: 4.09~9.43, P < 0.001), IL-6 (HR = 1.16, 95%CI: 1.09~1.31, P = 0.012), absolute value of T lymphocytes (HR = 0.47, 95%CI: 0.24~0.91, P = 0.025), mHLA-DR (HR = 0.46, 95%CI: 0.28~0.75, P = 0.002).Six factors were independent risk factors affecting the outcome of patients with septic shock to visualize the forest plots presented. Conclusions The age, the weighted average dose of norepinephrine and IL-6 are the dangerous factors affecting the prognosis of patients with septic shock. The hazard ratio is greater than 1. Nutrition, T-lymphocyte absolute value and mHLA-DR are the protection factors affecting the prognosis of patients with septic shock. The hazard ratio is less than 1. -
Key words:
- Septic shock /
- Norepinephrine /
- Cellular immunity /
- Prognostic analysis
-
表 1 2组患者基线资料比较[n(%)/
$\bar x \pm s $ ]Table 1. Comparison of general condition data between the two groups [n(%)/
$\bar x \pm s $ ]指标 生存组
(n = 71)死亡组
(n = 89)t/χ2 P 性别 0.086 0.769 女 19(26.76) 22(24.72) 男 52(73.24) 67(75.28) 年龄(岁) 60.97 ± 21.13 69.44 ± 18.43 −2.690 0.008* 体重指数(kg/m2) 22.12 ± 3.44 21.49 ± 4.34 1.016 0.311 既往病史 0.990 0.804 无 8(11.27) 14(15.73) 1种 43(60.56) 42(47.19) 2种 13(14.61) 24(26.97) 3种及以上 7(9.86) 9(10.11) 感染部位 14.397 0.026* 肺部 43(60.56) 45(50.56) 腹腔 11(15.49) 22(24.73) 血流 1(1.40) 9(10.11) 泌尿系 3(4.23) 0(0.00) 中枢神经系统 8(11.27) 9(10.11) 胆道 3(4.23) 1(1.12) 皮肤软组织 2(2.82) 3(3.37) 病原学 2.118 0.548 细菌 62(87.32) 69(77.53) 病毒 2(2.82) 5(5.62) 真菌 5(7.04) 13(14.60) 非典型病原体 2(2.82) 2(2.25) 病原来源 15.093 0.020* 痰液 21(29.58) 26(29.21) 肺泡灌洗液 18(25.35) 23(25.84) 血液 5(7.04) 12(13.48) 尿液 3(4.23) 0(0.00) 分泌物 17(23.94) 20(22.48) 引流液 4(5.63) 6(6.74) 脑脊液 3(4.23) 2(2.25) 营养方式 12.122 0.002* EN 40(56.34) 32(35.96) PN 18(25.35) 23(25.84) PN+EN 13(18.31) 34(38.20) APACHE-II评分 22.96 ± 5.53 27.33 ± 6.67 −4.431 < 0.001* SOFA评分 10.06 ± 2.96 12.13 ± 3.21 −4.208 < 0.001* *P < 0.05。 表 2 2组患者去甲肾上腺素加权平均剂量、血气、微循环指标情况比较[n(%)/
$\bar x \pm s $ ]Table 2. Comparison of the weighted average dose of noradrenaline,blood gas and microcirculation index between the two groups [n(%)/
$\bar x \pm s $ ]指标 生存组(n = 71) 死亡组(n = 89) t/χ2 P 去甲肾上腺素加权平均剂量[μg/(kg·min)] 0.26 ± 0.19 0.70 ± 0.48 −8.075 < 0.001* 血乳酸(Lac)(mmol/L) 3.11 ± 2.32 3.72 ± 2.51 −1.574 0.118 pH值 7.39 ± 0.10 7.36 ± 0.14 1.403 0.163 氧合指数(OI) 197.25 ± 104.50 174.93 ± 100.74 1.356 0.177 毛细血管再充盈时间(CRT) 5.413 0.020* < 3 s 28(39.44) 20(22.47) > 3 s 43(60.56) 69(77.53) *P < 0.05。 表 3 2组患者实验室检查资料比较[(
$\bar x \pm s $ )/M(P25,P75)]Table 3. Comparison of laboratory examination data between the two groups [(
$\bar x \pm s $ )/M(P25,P75)]指标 生存组(n = 71) 死亡组(n = 89) t/z P WBC(109/L) 13.55 ± 6.58 12.79 ± 6.92 0.708 0.480 NEUT% 86.01 ± 8.93 86.93 ± 9.02 −0.646 0.519 NEUT#(109/L) 11.90 ± 6.28 11.21 ± 6.38 0.684 0.695 LYMPH#(109/L) 0.78(0.45,1.31) 0.60(0.36,0.92) −2.203 0.028* NLR 14.09(7.78,28.13) 18.04(8.92,28.12) −0.970 0.332 PLR 222.58(105.71,411.43) 265.38(136.41,472.53) −0.804 0.422 MONO#(109/L) 0.53(0.35,0.92) 0.44(0.24,0.78) 1.455 0.146 PLT(109/L) 172.00(106.00,254.00) 162.00(77.00,227.00) 1.661 0.097 Hb(g/L) 111.34 ± 27.57 112.13 ± 31.05 −0.169 0.866 HCT 33.84 ± 8.14 34.60 ± 9.10 −0.555 0.580 PCT(ng/mL) 1.58(0.53,8.30) 1.82(0.65,8.09) −0.78 0.436 HS-CRP(mg/L) 86.50(24.80,144.10) 88.10(35.90,166.70) −1.123 0.261 PT(s) 16.10 ± 4.07 19.03 ± 8.77 −2.598 0.010* APTT(s) 45.48 ± 21.10 48.68 ± 20.21 −0.977 0.330 D-二聚体(mg/L) 3.02(2.00,6.37) 4.38(2.69,7.73) −0.204 0.041* TBIL(μmol/L) 16.30(8.80,30.60) 17.40(11.15,31.60) −1.267 0.205 ALT(IUl/L) 37.00(20.80,69.00) 31.00(20.60,68.00) 0.421 0.674 AST(IUl/L) 43.00(24.00,73.00) 50.80(29.00,83.94) −1.211 0.205 BUN(mmol/L) 9.60(7.00,14.60) 10.59(7.00,17.92) −0.524 0.600 肌酐(μmol/L) 105.3(69.60,170.40) 120.50(75.86,176.85) −0.687 0.492 ALB(g/L) 31.05 ± 18.69 26.75 ± 5.78 2.050 0.042* 血糖(mmol/L) 10.13 ± 4.91 10.22 ± 5.65 −0.109 0.914 K+(mmol/L) 4.01 ± 0.78 4.13 ± 0.91 −0.943 0.347 Na+(mmol/L) 140.01 ± 8.46 140.29 ± 8.52 −0.201 0.841 cTnI(ng/mL) 0.08(0.01,0.28) 0.10(0.03,0.49) −1.271 0.204 BNP(pg/mL) 137.32(47.06,428.53) 227.97(116.17,652.92) −1.824 0.068 *P < 0.05。 表 4 2组患者临床其它综合情况比较[n(%)/
$\bar x \pm s $ ]Table 4. Comparison of other comprehensive clinical conditions between the two groups [n(%)/
$\bar x \pm s $ ]指标 生存组(n = 71) 死亡组(n = 89) t/χ2 P 继发感染情况 24.050 < 0.002* 无 40(56.34) 23(25.84) 真菌 6(8.45) 26(29.21) 病毒 1(1.41) 2(2.25) 多重耐药菌 24(33.80) 38(42.70) 使用免疫球蛋白 0.598 0.439 否 63(88.73) 74(83.15) 是 8(11.27) 15(16.85) 使用血管加压素 0.299 0.584 否 62(87.32) 75(84.27) 是 9(12.68) 14(15.73) 应用血液净化 0.709 0.399 否 61(85.92) 72(80.90) 是 10(14.08) 17(19.10) 短效激素应用 2.942 0.086 否 40(56.34) 38(42.70) 是 31(43.66) 51(57.30) β-受体阻滞剂 0.222 0.638 否 23(32.39) 32(35.96) 是 48(67.61) 57(64.04) ≧2种血管活性药物 12.196 < 0.001* 否 55(77.46) 45(50.56) 是 16(22.54) 44(49.44) 应用人血白蛋白 11.753 < 0.001* 否 16(22.54) 4(4.49) 是 55(77.46) 85(95.51) 机械通气时间(h) 313.11 ± 239.64 250.97 ± 161.39 1.826 0.071 ICU住院时间(d) 15.69 ± 6.78 10.66 ± 6.62 3.957 < 0.001* *P < 0.05。 表 5 2组患者细胞免疫效应指标情况比较[M(P25,P75)]
Table 5. Comparison of the cellular immune effect indicators between the two groups [M(P25,P75)]
指标 生存组(n = 71) 死亡组(n = 89) z P IL-1β(pg/mL) 1.23(0.65,3.92) 1.71(0.79,5.06) −1.084 0.278 IL-2(pg/mL) 1.15(0.68,1.72) 1.35(1.01,2.13) −1.536 0.125 IL-4(pg/mL) 1.00(0.61,.39) 1.09(0.64,1.37) −0.11 0.911 IL-5(pg/mL) 1.93(1.18,3.36) 2.30(1.37,3.34) −1.034 0.301 IL-6(pg/mL) 46.75(19.09,103.51) 78.12(37.79,262.09) −3.526 0.004* IL-8(pg/mL) 3.60(0.68,17.87) 5.13(1.93,44.67) −1.782 0.025* IL-10(pg/mL) 1.94(1.33,3.98) 4.79(2.80,9.38) −2.792 0.009* TNF-α 0.84(0.49,1.68) 0.95(0.53,1.30) −0.231 0.817 CD3+/CD45+
#(个/μL)642.00(329.50,1020.50) 444.00(228.00,617.00) −2.321 0.010* CD3+CD8+/CD45+#(个/μL) 195.00(107.50,324.00) 192.00(83.00,284.00) −1.119 0.263 CD3+CD4+/CD45+#(个/μL) 297.00(222.00,461.00) 254.00(126.00,405.00) −2.101 0.036* CD4/CD8比值 1.48(1.07,2.25) 1.45(1.19,1.82) −0.389 0.697 CD64感染指数 2.50(1.22,4.56) 3.02(2.18,8.51) −2.668 0.008* mHLA-DR% 63.05(53.15,77.05) 29.05(15.60,72.70) −3.986 0.002* Tregs% 8.05(7.15,11.00) 7.05(5.60,9.30) −2.158 0.031* *P < 0.05。 表 6 预后模型中各个变量赋值表
Table 6. Table of various variables in the prognostic model
变量 各个变量赋值 年龄 连续变量 营养方式 设置哑变量EN + PN = 0,
EN或PN = 1去甲肾上腺素加权平均剂量 连续变量 IL-6 连续变量 T淋巴细胞绝对值 连续变量 mHLA-DR% 连续变量 表 7 影响28 d生存的COX回归模型分析
Table 7. The COX regression model analysis affecting survival at 28 days
变量 B S.E Wald P HR 95%CI 年龄 0.01 0.01 4.40 0.036* 1.05 1.09-1.12 营养方式 −0.30 0.145 4.34 0.037* 0.74 0.56-0.90 去甲肾上腺素加权平均剂量 1.83 0.21 73.34 < 0.001* 6.21 4.09-9.43 IL-6 0.15 0.06 6.26 0.012* 1.16 1.09-1.31 T淋巴细胞绝对值 −0.75 0.34 5.00 0.025* 0.47 0.24-0.91 mHLA-DR% −0.78 0.25 9.83 0.002* 0.46 0.28-0.75 B值为回归系数,S.E为标准误,Wald为瓦尔德卡方值,HR为风险比,*P < 0.05。 -
[1] Napolitano L M. Sepsis 2018:Definitions and guideline changes[J]. Surg Infect (Larchmt),2018,19(2):117-125. doi: 10.1089/sur.2017.278 [2] Uhel F,van der Poll T. Norepinephrine in septic shock: A mixed blessing[J]. American Journal of Respiratory and Critical Care Medicine,2020,202(6):788-789. doi: 10.1164/rccm.202006-2301ED [3] 中国医师协会急诊医师分会,中国研究型医院学会休克与脓毒症专业委员会. 中国脓毒症/脓毒性休克急诊治疗指南(2018)[J]. 中国急救医学,2018,38(9):741-756. doi: 10.3969/j.issn.1002-1949.2018.09.001 [4] Riley R D,Ensor J,Snell K I E,et al. Calculating the sample size required for developing a clinical prediction model[J]. BMJ,2020,368(18):m441. [5] Rhodes A,Evans L E,Alhazzani W,et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock: 2016[J]. Intensive Care Med,2017,43(3):304-377. doi: 10.1007/s00134-017-4683-6 [6] Evans L,Rhodes A,Alhazzani W,et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021[J]. Intensive Care Med,2021,47(11):1181-1247. doi: 10.1007/s00134-021-06506-y [7] Stolk R,Kox M,Pickkers P. Noradrenaline drives immunosuppression in sepsis: Clinical consequences[J]. Intensive Care Medicine,2020,46(6):1246-1248. [8] 纪美玲,彭易根,杨宝成,等. 年龄对乳酸清除率预测脓毒性休克患者预后价值的影响[J]. 国际麻醉学与复苏杂志,2020,41(4):335-339. [9] Michels E H A,Butler J M,Reijnders T D Y,et al. Association between age and the host response in critically ill patients with sepsis[J]. Crit Care,2022,26(1):385. doi: 10.1186/s13054-022-04266-9 [10] Basodan N,Al Mehmadi A E,Aldawood S M,et al. Septic shock: Management and outcomes[J]. Cureus,2022,14(12):e32158. doi: 10.7759/cureus.32158 [11] Van Niekerk G,Meaker C,Engelbrecht A M. Nutritional support in sepsis: when less may be more[J]. Crit Care,2020,24(1):53. doi: 10.1186/s13054-020-2771-4 [12] Kott M,Hartl W H,Elke G. Enteral vs. parenteral nutrition in septic shock: are they equivalent?[J]. Curr Opin Crit Care,2019,25(4):340-348. doi: 10.1097/MCC.0000000000000618 [13] Ridley E J,Lambell K. Nutrition before,during and after critical illness[J]. Curr Opin Crit Care,2022,28(4):395-400. doi: 10.1097/MCC.0000000000000961 [14] Lambell K J,Tatucu-Babet O A,Chapple L A,et al. Nutrition therapy in critical illness:A review of the literature for clinicians[J]. Crit Care,2020,24(1):35. doi: 10.1186/s13054-020-2739-4 [15] Hamzaoui O,Scheeren T W L,Teboul J L. Norepinephrine in septic shock: when and how much?[J]. Curr Opin Crit Care,2017,23(4):342-347. [16] Auchet T,Regnier M A,Girerd N,etal. Outcome of patients with septic shock and high-dose vasopressor therapy[J]. Ann Intensive Care,2017,7(1):43. doi: 10.1186/s13613-017-0261-x [17] 范文婧,陈贵梅,苑俊,等. 去甲肾上腺素对于脓毒症/脓毒性休克患者预后的评估价值[J]. 安徽医科大学学报,2020,55(12):1950-1954. [18] Yamamura H,Kawazoe Y,Miyamoto K,et al. Effect of norepinephrine dosage on mortality in patients with septic shock[J]. Journal of Intensive Care,2018,6:12. doi: 10.1186/s40560-018-0280-1 [19] Domizi R,Calcinaro S,Harris S,et al. Relationship between norepinephrine dose,tachycardia and outcome in septic shock: A multicentre evaluation[J]. J Crit Care,2020,57(1):185-190. [20] 中国医药教育协会感染疾病专业委员会. 感染相关生物标志物临床意义解读专家共识[J]. 中华结核和呼吸杂志,2017,40(4):243-257. [21] 穆艳平,杨长君,李霞. 外周血白细胞介素-6降钙素原水平对脓毒症及脓毒性休克患者预后的评估价值[J]. 实用医技杂志,2022,29(5):536-538. [22] 赵琨,杨德兴,蒋国云,等. 细胞因子在诊断感染性疾病及其严重程度中的价值[J]. 昆明医科大学学报,2020,41(10):101-107. [23] Thao P T N,Tra T T,Son N T,et al. Reduction in the IL-6 level at 24 h after admission to the intensive care unit is a survival predictor for Vietnamese patients with sepsis and septic shock: a prospective study[J]. BMC Emerg Med,2018,18(1):39. doi: 10.1186/s12873-018-0191-4 [24] Song J,Park D W,Moon S,et al. Diagnostic and prognostic value of interleukin-6,pentraxin 3,and procalcitonin levels among sepsis and septic shock patients: a prospective controlled study according to the Sepsis-3 definitions[J]. BMC Infect Dis,2019,19(1):968. doi: 10.1186/s12879-019-4618-7 [25] 陈涛,臧彬. 脓毒症及脓毒性休克患者T淋巴细胞亚群变化研究[J]. 临床军医杂志,2017,45(1):46-48. [26] 张思也,侯粲,钟燕军,等. 脓毒症T淋巴细胞亚群免疫监测的研究进展[J]. 中华重症医学电子杂志,2021,07(1):48-54. [27] Liu J,Li S,Liu J,et al. Longitudinal characteristics of lymphocyteresponses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients[J]. EBio Medicine,2020,55(5):102763. [28] Li Q,Yan W,Liu S,et al. Study on the correlation and clinical significance of T-lymphocyte Subsets,IL-6 and PCT in the severity of patients with sepsis[J]. Pak J Med Sci,2023,39(1):227-231. [29] Bourgoin P,Taspinar R,Gossez M,et al. Toward monocyte HLA-DR bedside monitoring: A proof-of-concept study[J]. Shock,2021,55(6):782-789. doi: 10.1097/SHK.0000000000001673 [30] Bodinier M,Peronnet E,Brengel-Pesce K,et al. Monocyte trajectories endotypes are associated with worsening in septic patients[J]. Front Immunol,2021,12:795052. doi: 10.3389/fimmu.2021.795052 [31] Quadrini K J,Patti-Diaz L,Maghsoudlou J,et al. A flow cytometric assay for HLA-DR expression on monocytes validated as a biomarker for enrollment in sepsis clinical trials[J]. Cytometry B Clin Cytom,2021,100(1):103-114. doi: 10.1002/cyto.b.21987 [32] Sanju S,Jain P,Priya V V,et al. Quantitation of mHLA-DR and nCD64 by flow cytometry to study dysregulated host Response: The use of quantiBRITE™ PE beads and Its stability[J]. Appl Biochem Biotechnol,2022,11(1):1-6. [33] Leijte G P,Rimmelé T,Kox M,et al. Monocytic HLA-DR expression kinetics in septic shock patients with different pathogens,sites of infection and adverse outcomes[J]. Crit Care,2020,24(1):110. [34] 陈建平,李小悦,傅明. 脓毒症免疫抑制机制及免疫调理治疗新进展[J]. 医学综述,2021,27(13):2600-2605. [35] Pei F,Yao R Q,Ren C,etal. Expert consensus on the monitoring and treatment of sepsis-induced immunosuppression[J]. Mil Med Res,2022,9(1):74. -






 下载:
下载: