The Intervention of Digital Technology in the Correction of Maxillary Labial High Canine Teeth
-
摘要:
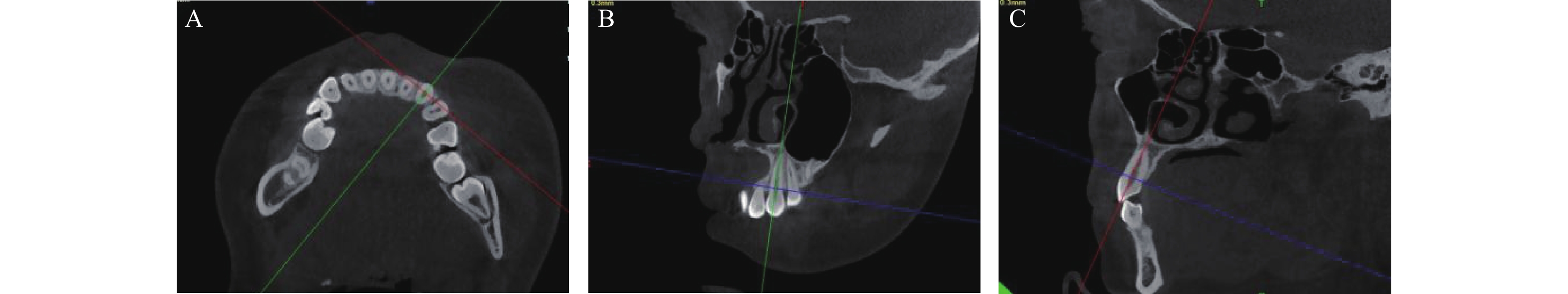
目的 为预防上颌唇向低位尖牙矫治后的牙槽骨水平吸收,探索用数字化技术对上颌唇向低位尖牙矫治前进行精准施力的干预以期改善牙槽嵴顶吸收的临床疗效。 方法 纳入43名成年矫治患者的54颗上颌唇向低位尖牙,将其分为干预组和未干预组,对治疗前后釉牙骨质界到牙槽嵴顶距离(CEJ-AC)等相关指标进行统计分析。 结果 (1)矫治后干预组CEJ-AC小于治疗前(P < 0.05),未干预组CEJ-AC不变;(2)矫治前后,薄龈型患者的CEJ-AC变化,差异无统计学意义(P > 0.05),干预组厚龈型患者的CEJ-AC降低(P < 0.05);(3)固定矫治干预组矫治后CEJ-AC值降低(P < 0.05),治疗前后的CEJ-AC差值大于常规矫治组(P < 0.05);隐形矫治干预组矫治后的CEJ-AC降低值大于常规矫治组(P < 0.05)。 结论 干预措施对厚龈型患者矫治后的CEJ-AC有改善作用,但对薄龈型无明显作用;在固定矫治或隐形矫治前进行干预,均有效果。 Abstract:Objective To explore the use of digital technology to intervene in the precise force stimuli for labial high positioned maxillary canines before the orthodontic treatment so as to improve alveolar crest absorption. Methods 54 maxillary labial low canine teeth from 43 adult orthodontic patients were included and divided into an intervention group and a non-intervention group. The distance between cemento-enamel bone junction and alveolar crest (CEJ-AC) before and after the treatment and other relevant data were statistically analyzed. Results 1. There was no statistical difference of CEJ-AC between the intervention group and the non-intervention group before the treatment; After the treatment, the CEJ-AC in the intervention group was lower than that before the treatment (P < 0.05), and there was no statistical difference of the CEJ-AC in the non-intervention group . 2. Before and after the treatment, there was no statistical difference in the changes of CEJ-AC in patients with thin gingival biotype, but decreased in patients with thick gingival biotype in the intervention group (P < 0.05). 3. The CEJ-AC decreased after the fixed orthodontic therapy intervention group (P < 0.05), and the difference between CEJ-AC before and after the treatment was greater than that in the conventional correction group (P < 0.05), while the reduction value of CEJ-AC of the invisible intervention group after the orthodontic therapy was greater than that in the conventional correction group (P < 0.05). Conclusion Pre-treatment intervention appliance with digitally designed for labial high maxillary canines can improve alveolar crest absorption after the orthodontic treatment in patients with thick gingival biotype. However, there are no significant effects on thin gingival biotype. Interventions prior to fixed or invisible correction are both effective. -
Key words:
- Labial high maxillary canine /
- Occlusal hypofunction /
- Orthodontics /
- Digital technology
-
表 1 常规矫治矫治组和干预矫治组矫治前后CEJ-AC情况[(
$ \bar{x} \pm s $ ),mm]Table 1. CEJ-AC before and after treatment in the non-intervention group and the intervention group[(
$ \bar{x} \pm s $ ),mm]组别 n(颗) 治疗前 治疗后 治疗前后差值 t P 常规矫治组 32 3.30 ± 1.91 3.43 ± 1.63 −0.13 ± 0.11 −1.25 0.220 干预矫治组 22 3.63 ± 1.58 3.15 ± 1.32 0.48 ± 0.12 4.01 0.001* t −0.66 0.68 3.79 P 0.515 0.499 < 0.001* *P < 0.05。 表 2 干预措施对不同牙龈型矫治前后CEJ-AC的影响[(
$ \bar{x} \pm s $ ),mm]Table 2. Effect of interventions on CEJ-AC before and after treatment with different gingival type [(
$ \bar{x} \pm s $ ),mm]组别 n(颗) 治疗前 治疗后 治疗前后差值 t P 薄龈型 常规矫治组 19 3.32 ± 2.05 3.57 ± 1.71 −0.25 ± 0.16 −1.59 0.129 干预矫治组 12 3.39 ± 1.47 3.22 ± 1.31 0.18 ± 0.11 1.64 0.129 t −0.10 0.61 1.98 P 0.918 0.547 0.058 厚龈型 常规矫治组 13 3.28 ± 1.76 3.24 ± 1.55 0.04 ± 0.11 0.34 0.743 干预矫治组 10 3.91 ± 1.73 3.07 ± 1.39 0.84 ± 0.17 4.92 0.001* t −0.86 0.27 4.04 P 0.400 0.790 0.001* *P < 0.05。 表 3 干预措施对不同矫治方式矫治前后CEJ-AC的影响[(
$\bar{x} \pm s $ ),mm]Table 3. Effect of interventions on CEJ-AC before and after treatment with different treatment methods [(
$\bar{x} \pm s $ ),mm]组别 n(颗) 治疗前 治疗后 治疗前后差值 t P 固定矫治 常规矫治组 26 3.38±1.88 3.47±1.61 0.10±0.11 0.81 0.428 干预矫治组 14 3.12±1.35 2.73±1.17 −0.39±0.10 −3.65 0.003* t 0.45 1.52 2.69 P 0.657 0.137 0.010* 隐形矫治 常规矫治组 6 2.98±2.17 3.27±1.84 0.28±0.22 1.27 0.259 干预矫治组 8 4.51±1.62 3.89±1.28 −0.63±0.27 −2.29 0.055 t −1.51 −0.75 2.45 P 0.156 0.470 0.030* *P < 0.05。 -
[1] Kenessey D E,Vlemincq-mendieta T,Scott G R,et al. An anthropological investigation of the sociocultural and economic forces shaping dental crowding prevalence[J]. Archives of Oral Biology,2023,147(3):105614. [2] Shigenobu N,Hisano M,Shima S,et al. Patterns of dental crowding in the lower arch and contributing factors. A statistical study[J]. The Angle Orthodontist,2007,77(2):303-310. doi: 10.2319/0003-3219(2007)077[0303:PODCIT]2.0.CO;2 [3] Massaro C,Miranda F,Janson G,et al. Maturational changes of the normal occlusion: A 40-year follow-up[J]. Am J Orthod Dentofacial Orthop,2018,154(2):188-200. doi: 10.1016/j.ajodo.2017.10.028 [4] Mochizuki M,Hasegawa K,Machida Y. A longitudinal study of the development of crowded dental arch[J]. The Bulletin of Tokyo Dental College,1998,39(1):41-46. [5] Mucedero M,Ricchiuti M R,Cozza P,et al. Prevalence rate and dentoskeletal features associated with buccally displaced maxillary canines[J]. European Journal of Orthodontics,2013,35(3):305-309. doi: 10.1093/ejo/cjr133 [6] Mucedero M,Rozzi M,Di Fusco G,et al. Morphometric analysis of the palatal shape and arch dimension in subjects with buccally displaced canine[J]. European Journal of Orthodontics,2020,42(5):544-550. doi: 10.1093/ejo/cjz091 [7] Alhaija E S A,Alwahadni A M,Al-tawachi A,et al. Evaluation of maxillary sinus dimensions and volume using cone beam computed tomography in patients with unilaterally displaced palatal and buccal maxillary canines[J]. Oral Radiology,2023,39(3):504-516. doi: 10.1007/s11282-022-00663-6 [8] 季娟娟,范群,周治,等. 咬合功能低下对正畸中牙龈组织CTGF表达的影响[J]. 昆明医科大学学报,2018,39(8):18-22. doi: 10.3969/j.issn.1003-4706.2018.08.005 [9] Ji J J,Li X D,Fan Q,et al. Prevalence of gingival recession after orthodontic treatment of infraversion and open bite[J]. J Orofac Orthop,2019,80(1):1-8. doi: 10.1007/s00056-018-0159-8 [10] Kan J Y,Rungcharassaeng K,Umezu K,et al. Dimensions of peri-implant mucosa: an evaluation of maxillary anterior single implants in humans[J]. Journal of Periodontology,2003,74(4):557-562. doi: 10.1902/jop.2003.74.4.557 [11] Denes B J,Mavropoulos A,Bresin A,et al. Influence of masticatory hypofunction on the alveolar bone and the molar periodontal ligament space in the rat maxilla[J]. European Journal of Oral Sciences,2013,121(6):532-537. doi: 10.1111/eos.12092 [12] 毛铭馨,徐莉,靖无迪,等. 骨性安氏Ⅲ类错(牙合)畸形患者前牙唇侧牙槽嵴顶位置及相关因素分析[J]. 北京大学学报(医学版),2020,52(1):77-82. [13] Kook Y A,Kim G,Kim Y. Comparison of alveolar bone loss around incisors in normal occlusion samples and surgical skeletal class III patients[J]. The Angle Orthodontist,2012,82(4):645-652. doi: 10.2319/070111-424.1 [14] Alsino H I,Hajeer M Y,Alkhouri I,et al. The diagnostic accuracy of cone-beam computed tomography (CBCT) imaging in detecting and measuring dehiscence and fenestration in patients with class I malocclusion: A surgical-exposure-based validation study[J]. Cureus,2022,14(3):e22789. [15] Usumi-fujita R,Hosomichi J,Ono N,et al. Occlusal hypofunction causes periodontal atrophy and VEGF/VEGFR inhibition in tooth movement[J]. The Angle Orthodontist,2013,83(1):48-56. doi: 10.2319/011712-45.1 [16] Termsuknirandorn S,Hosomichi J,Soma K. Occlusal stimuli influence on the expression of IGF-1 and the IGF-1 receptor in the rat periodontal ligament[J]. Angle Orthod,2008,78(4):610-616. [17] Shafizadeh M,Amid R,Tehranchi A,et al. Evaluation of the association between gingival phenotype and alveolar bone thickness: A systematic review and meta-analysis[J]. Archives of Oral Biology,2022,133(1):105287. [18] Ashfaq M,Sadiq A,Sukhia R H,et al. Association of hard and soft tissue factors with gingival recession in orthodontically treated patients: A retrospective study[J]. International Orthodontics,2021,19(1):60-66. doi: 10.1016/j.ortho.2020.12.001 [19] 卢海丽,康娜. 无托槽隐形矫治器与固定矫治器对正畸患者牙周健康影响的研究现状和进展[J]. 口腔医学研究,2019,35(7):625-628. doi: 10.13701/j.cnki.kqyxyj.2019.07.002 [20] Wang Y,Chen J,Qin S,et al. An in vivo evaluation of clear aligners for optimal orthodontic force and movement to determine high-efficacy and periodontal-friendly aligner staging[J]. Heliyon,2023,9(4):e15317. doi: 10.1016/j.heliyon.2023.e15317 -






 下载:
下载: