|
[1]
|
Tatemoto K,Rökaeus A,Jörnvall H,et al. Galanin-a novel biologically active peptide from porcine intestine[J]. FEBS Lett,1983,164(1):124-128. doi: 10.1016/0014-5793(83)80033-7
|
|
[2]
|
Taylor T S,Konda P,John S S,et al. Galanin suppresses visceral afferent responses to noxious mechanical and inflammatory stimuli[J]. Physiological Reports,2020,8(2):e14326.
|
|
[3]
|
Yu M,Fang P H,Wang H,et al. Beneficial effects of galanin system on diabetic peripheral neuropathic pain and its complications[J]. Peptides,2020,134(12):170404.
|
|
[4]
|
Liu F, Yajima T, Wang M, et al. Effects of trigeminal nerve injury on the expression of galanin and its receptors in the rat trigeminal ganglion [J]. Neuropeptides, 2020, 84(期号!): 102098.Liu F,Yajima T,Wang M,et al. Effects of trigeminal nerve injury on the expression of galanin and its receptors in the rat trigeminal ganglion[J]. Neuropeptides,2020,84:102098.
|
|
[5]
|
Amorim D,David-Pereira A,Marques P,et al. A role of supraspinal galanin in behavioural hyperalgesia in the rat[J]. Plos one,2014,9(11):e113077. doi: 10.1371/journal.pone.0113077
|
|
[6]
|
Dias E V,Sartori C R,Mariao P R,et al. Nucleus accumbens dopaminergic neurotransmission switches its modulatory action in chronification of inflammatory hyperalgesia[J]. Eur J Neurosci,2015,42(7):2380-2389. doi: 10.1111/ejn.13015
|
|
[7]
|
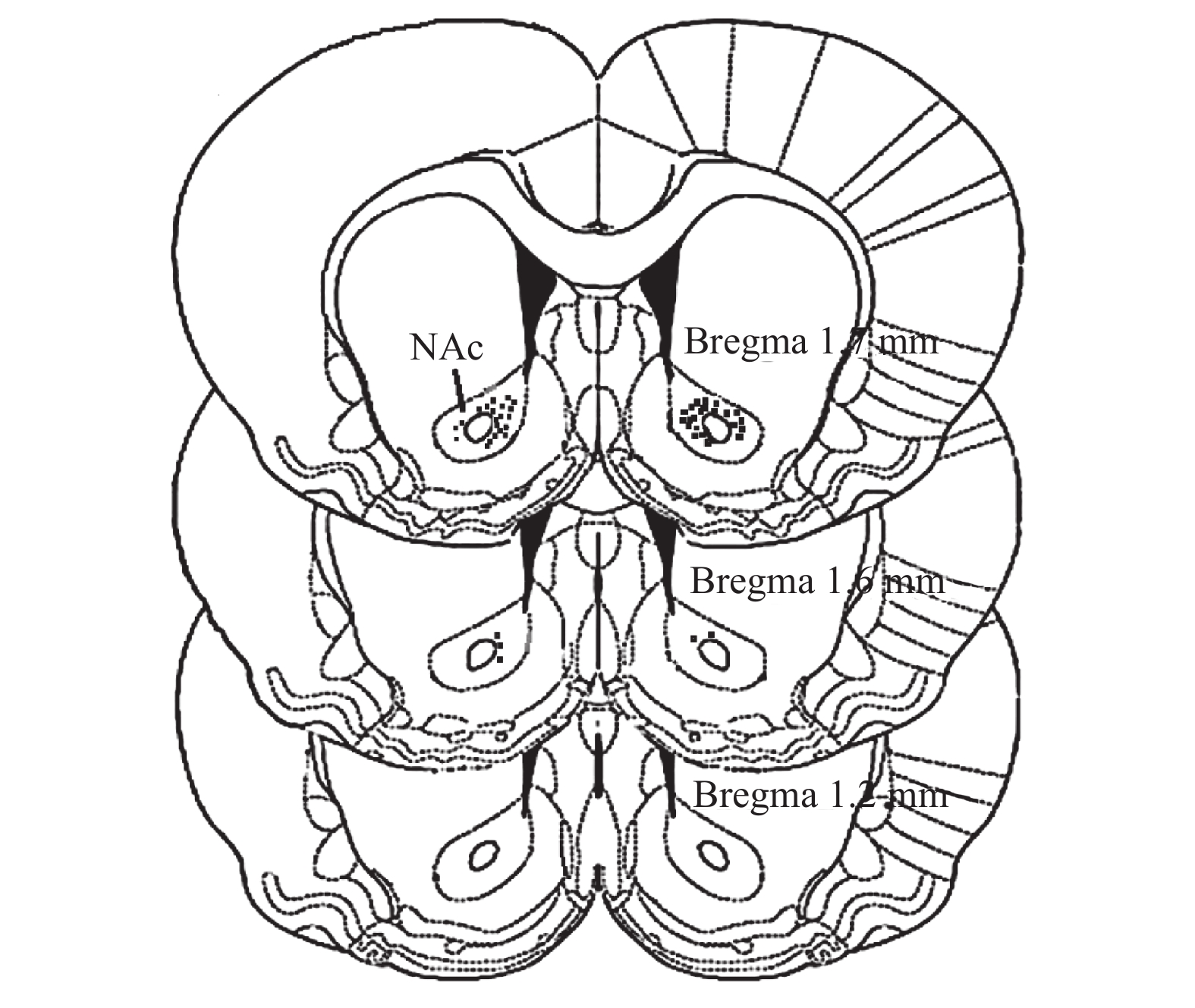
Duan H,Zhang Y,Zhang X M,et al. Antinociceptive roles of galanin receptor 1 in nucleus accumbens of rats in a model of neuropathic pain[J]. J Neurosci Res,2015,93(10):1542-1551. doi: 10.1002/jnr.23611
|
|
[8]
|
Mitsukawa K,Lu X,Bartfai T. Galanin,galanin receptors and drug targets[J]. Cell Mol Life Sci,2008,65(12):1796-1805. doi: 10.1007/s00018-008-8153-8
|
|
[9]
|
Gear R W,Aley K O,Levine J D. Pain—induced analgesia mediated by mesolimbic reward circuits[J]. J Neurosci,1999,19(16):7175-7181. doi: 10.1523/JNEUROSCI.19-16-07175.1999
|
|
[10]
|
Watanabe M,Sugiura Y,Sugiyama E,et al. Extracellular N- acetylaspartylglutamate released in the nucleus accumbens modulates the pain sensation: Analysis using a microdialysis/mass spectrometry integrated system[J]. Mol Pain,2018,14:1744806918754934.
|
|
[11]
|
Zhang Y, Gao Y, Li CY, et al. Galanin plays a role in antinociception via binding to galanin receptors in the nucleus accumbens of rats with neuropathic pain [J]. Neurosci Lett, 2019, 706(期号?): 93-98.Zhang Y,Gao Y,Li C Y,et al. Galanin plays a role in antinociception via binding to galanin receptors in the nucleus accumbens of rats with neuropathic pain[J]. Neurosci Lett,2019,706:93-98.
|
|
[12]
|
Zhang, ML, Fu, FH, Yu, LC. Antinociception induced by galanin in anterior cingulate cortex in rats with acute inflammation [J]. Neurosci. Lett. 2017, 638(期号?): 156-161.Zhang M L,Fu F H,Yu L C. Antinociception induced by galanin in anterior cingulate cortex in rats with acute inflammation[J]. Neurosci Lett,2017,638:156-161.
|
|
[13]
|
Zhang M L,Wang H B,Fu F H,et al. Involvement of galanin and galanin receptor 2 in nociceptive modulation in anterior cingulate cortex of normal rats and rats with mononeuropathy[J]. Sci Rep,2017,7(1):45930. doi: 10.1038/srep45930
|
|
[14]
|
Li S Y,Huo M L,Wu X Y,et al. Involvement of galanin and galanin receptor 1 in nociceptive modulation in the central nucleus of amygdala in normal and neuropathic rats[J]. Sci Rep,2017,7(1):15317. doi: 10.1038/s41598-017-13944-6
|
|
[15]
|
Li L X, Wang X B, Yu L C. Involvement of opioid receptors in the CGRP-induced antinociception in the nucleus accumbens of rats[J]. Brain Res,2010,1353:53-59.
|
|
[16]
|
Hobson S A,Bacon A,Elliot-Hunt C R,et al. Galanin acts as a trophic factor to the central and peripheral nervous systems[J]. Cell Mol Life Sci,2008,65(12):1806-1812.
|
|
[17]
|
Barreda-Gómez G,Giralt M T,Rodríguez-Puertas R. G protein-coupled galanin receptor distribution in the rat central nervous system[J]. Neuropeptides,2005,39(3):153-156.
|
|
[18]
|
Lang R,Gundlach A L,Holmes F E,et al. Physiology,signaling,and pharmacology of galanin peptides and receptors: Three decades of emerging diversity[J]. Pharmacol Rev,2015,67(1):118-175. doi: 10.1124/pr.112.006536
|
|
[19]
|
Chen S H,Lue J H,Hsiao Y J,et al. Elevated galanin receptor type 2 primarily contributes to mechanical hypersensitivity after median nerve injury[J]. PLoS ONE,2018,13(6):e0199512.
|
|
[20]
|
Xu X F,Yang X D,Zhang P,et al. Effects of exogenous galanin on neuropathic pain state and change of galanin and its receptors in DRG and SDH after sciatic nerve-pinch injury in rat[J]. Plos One,2012,7(5):e37621. doi: 10.1371/journal.pone.0037621
|
|
[21]
|
Dong Yan,Li Chongyang,Zhang Xiaomin,et al. The activation of galanin receptor 2 plays an antinociceptive effect in nucleus accumbens of rats with neuropathic pain[J]. J Physiol Sci,2021,71(1):6. doi: 10.1186/s12576-021-00790-5
|
|
[22]
|
Mengnan Li, Xiaomin Zhang, Chongyang Li, et al. Galanin receptor 2 is involved in galanin-induced analgesic effect by activating PKC and CaMKII in the nucleus accumbens of inflammatory pain rats [J]. Front Neurosci, 2021, 14(期号?): 593331.Li Mengnan,Zhang Xiaomin,Li Chongyang,et al. Galanin receptor 2 is involved in galanin-induced analgesic effect by activating PKC and CaMKII in the nucleus accumbens of inflammatory pain rats[J]. Front Neurosci,2021,14:593331.
|






 下载:
下载: