Metformin Inhibits high Glucose-induced Vascular Smooth Muscle Cells Proliferation by Promoting Autophagy via AMPK/PPAR-γ
-
摘要:
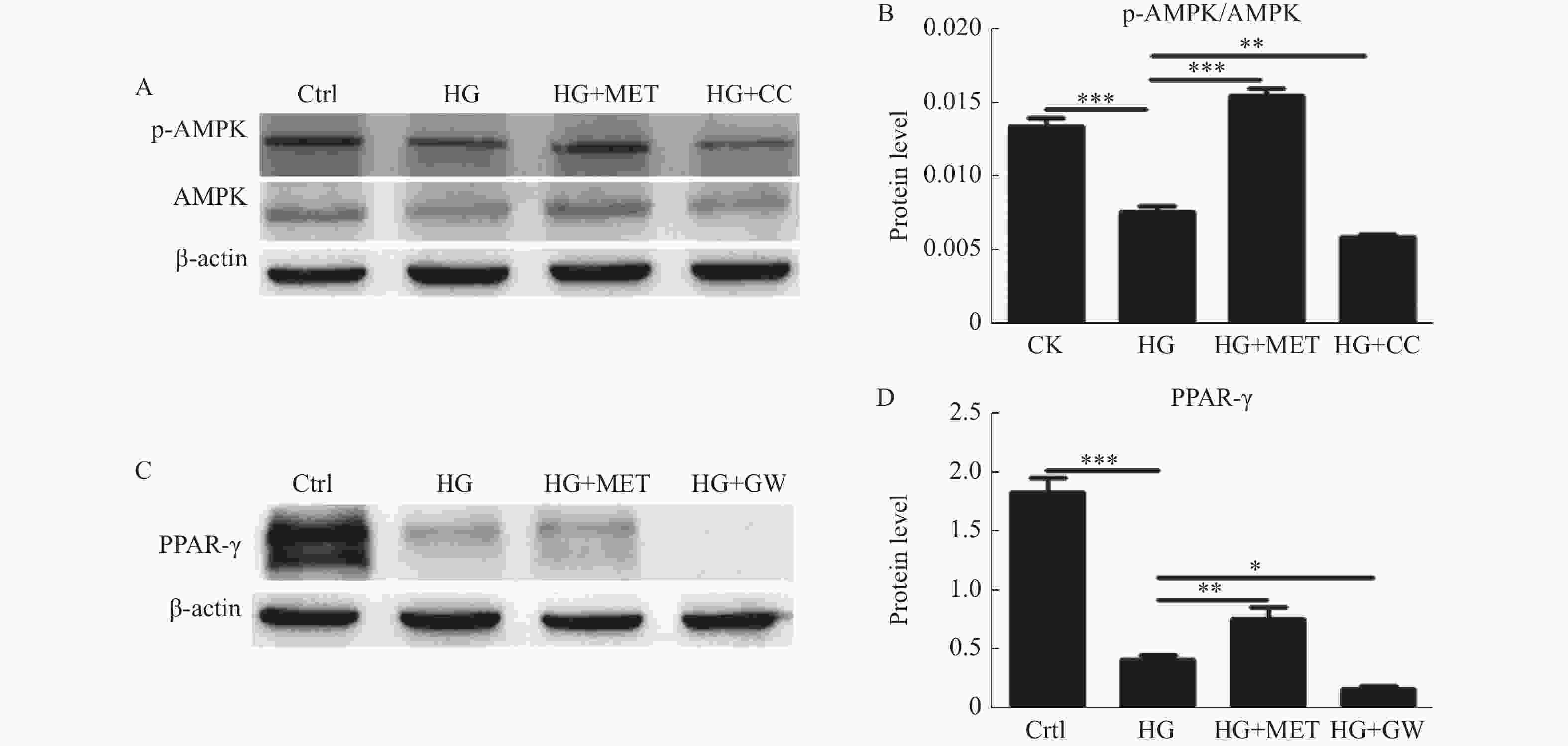
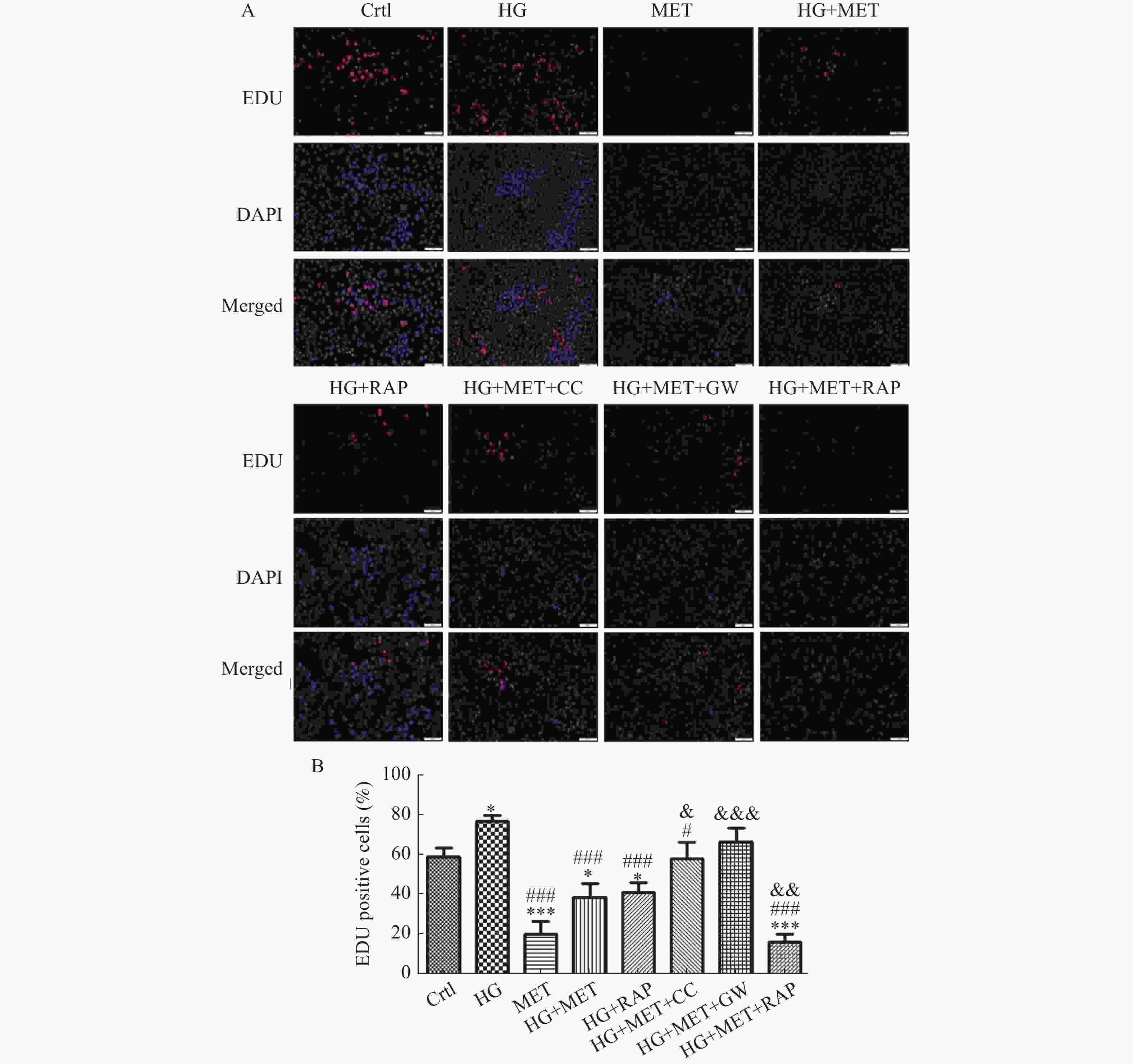
目的 探讨二甲双胍(Metformin)对高糖培养的小鼠主动脉血管平滑肌细胞(vascular smooth muscle cell,VSMCs)自噬、细胞增殖的影响及其调控机制。 方法 用Western blot检测不同处理组微管相关蛋白轻链-3-Ⅱ(LC3-Ⅱ),Becline-1蛋白水平变化,透射电镜观察各处理组VSMCs自噬小体水平;用Western blot检测不同处理组p-AMPK/AMPK、PPAR-γ蛋白表达水平;用EDU法检测不同处理组VSMCs增殖情况。 结果 二甲双胍、雷帕霉素逆转高糖抑制VSMCs自噬的作用(P < 0.001);Compound C、GW9662增加高糖抑制VSMCs自噬的作用(P < 0.05);二甲双胍逆转高糖对AMPK/PPAR-γ通路的负调控(P < 0.01);二甲双胍、雷帕霉素抑制高糖促进的VSMCs增殖(P < 0.001),Compound C、GW9662逆转二甲双胍抑制高糖促VSMCs增殖的作用(P < 0.05)。 结论 高糖促进VSMCs增殖可能是自噬调节相关的,二甲双胍可通过激活AMPK/PPAR-γ通路上调VSMCs自噬水平,抑制高糖促进的VSMCs异常增殖。 Abstract:Objective To investigate the effect and regulatory mechanism of metformin on autophagy and cell proliferation of vascular smooth muscle cells (VSMCs) cultured in high glucose in mice aortic. Methods Western blot was used to detect the changes in microtubule-associated protein light chain 3-II (LC3-II) and Beclin-1 protein levels in different treatment groups. Transmission electron microscope was used to observe the the level of autophagosomes in VSMCs of each treatment group. Western blot was used to detect the expression levels of p-AMPK/AMPK and PPAR-γ proteins in different treatment groups. The EDU method was used to detect the proliferation of VSMCs in different treatment groups. Results Metformin and rapamycin reversed the inhibitory effect of high glucose on VSMC autophagy (P < 0.001). Compound C and GW9662 enhanced the inhibitory effect of high glucose on VSMC autophagy (P < 0.05). Metformin reversed the negative regulation of high glucose on the AMPK/PPAR-γ pathway (P < 0.01). Metformin and rapamycin inhibited high glucose-induced VSMC proliferation (P < 0.001), and Compound C and GW9662 reversed the inhibitory effect of metformin on high glucose-induced VSMC proliferation (P < 0.05). Conclusion High glucose promotes the proliferation of VSMCs, which may be regulated by autophagy. Metformin can upregulate autophagy levels in VSMCs by activating the AMPK/PPAR-γ pathway, thereby inhibiting the abnormal proliferation of VSMCs induced by high sugar. -
Key words:
- Metformin /
- High glucose /
- Autophagy /
- Vascular smooth muscle cell /
- Proliferation
-
图 3 二甲双胍对高糖培养下VSMCs p-AMPK/AMPK、PPAR-γ表达的影响
A:Western blot检测对照组、HG组、HG+MET组及HG+CC组p-AMPK/AMPK的表达;B:定量分析不同处理组p-AMPK/AMPK的表达水平;C:Western blot检测对照组、HG组、HG+MET组及HG+GW组PPAR-γ的表达;D:定量分析不同处理组PPAR-γ的表达水平。*P < 0.05,**P < 0.01,***P < 0.001。
Figure 3. Effect of metformin and high glucose on p-AMPK/AMPK、PPAR-γexpression of VSMCs
-
[1] Chiong M,Morales P,Torres G,et al. Influence of glucose metabolism on vascular smooth muscle cell proliferation[J]. Vasa,2013,42(1):8-16. doi: 10.1024/0301-1526/a000243 [2] Yang M,Fang J,Liu Q,et al. Role of ROS-TRPM7-ERK1/2 axis in high concentration glucose-mediated proliferation and phenotype switching of rat aortic vascular smooth muscle cells[J]. Biochemical and Biophysical Research Communications,2017,494(3-4):526-533. doi: 10.1016/j.bbrc.2017.10.122 [3] Marino G,Niso-Santano M,Baehrecke E H,et al. Self-consumption: The interplay of autophagy and apoptosis[J]. Nat Rev Mol Cell Biol,2014,15(2):81-94. doi: 10.1038/nrm3735 [4] Wu H,Song A,Hu W,et al. The anti-atherosclerotic effect of paeonol against vascular smooth muscle cell proliferation by up-regulation of autophagy via the AMPK/mTOR signaling pathway[J]. Frontiers in Pharmacology,2018,8:948. doi: 10.3389/fphar.2017.00948 [5] 张紫微,杨丽霞,吕晋琳,等. 血管紧张素Ⅱ诱发自噬对血管平滑肌细胞表型转换的调控作用[J]. 中国动脉硬化杂志,2017,25(5):452-456. [6] Phadwal K,Feng D,Zhu D,et al. Autophagy as a novel therapeutic target in vascular calcification[J]. Pharmacology & Therapeutics,2020,206:107430. [7] Peng S,Xu L,Che X,et al. Atorvastatin inhibits inflammatory response,attenuates lipid deposition,and improves the stability of vulnerable atherosclerotic plaques by modulating autophagy[J]. Frontiers in Ppharmacology,2018,9:438. doi: 10.3389/fphar.2018.00438 [8] Poznyak A V,Litvinova L,Poggio P,et al. From diabetes to atherosclerosis: Potential of metformin for management of cardiovascular disease[J]. International Journal of Molecular Sciences,2022,23(17):9738. doi: 10.3390/ijms23179738 [9] Yang Q,Yuan H,Chen M,et al. Metformin ameliorates the progression of atherosclerosis via suppressing macrophage infiltration and inflammatory responses in rabbits[J]. Life Sciences,2018,198:56-64. doi: 10.1016/j.lfs.2018.02.017 [10] Wu H,Feng K,Zhang C,et al. Metformin attenuates atherosclerosis and plaque vulnerability by upregulating KLF2-mediated autophagy in apoE−/-mice[J]. Biochemical and Biophysical Research Communications,2021,557:334-341. doi: 10.1016/j.bbrc.2021.04.029 [11] Phadwal K,Koo E,Jones R A,et al. Metformin protects against vascular calcification through the selective degradation of Runx2 by the p62 autophagy receptor[J]. Journal of Cellular Physiology,2022,237(11):4303-4316. doi: 10.1002/jcp.30887 [12] Yang B,Gao X,Sun Y,et al. Dihydroartemisinin alleviates high glucose-induced vascular smooth muscle cells proliferation and inflammation by depressing the miR-376b-3p/KLF15 pathway[J]. Biochemical and Biophysical Research Communications,2020,530(3):574-580. doi: 10.1016/j.bbrc.2020.07.095 [13] Yuan T,Yang T,Chen H,et al. New insights into oxidative stress and inflammation during diabetes mellitus-accelerated atherosclerosis[J]. Redox Biology,2019,20:247-260. doi: 10.1016/j.redox.2018.09.025 [14] Tiong Y L,Ng K Y,Koh R Y,et al. Melatonin inhibits high glucose-induced ox-LDL/LDL expression and apoptosis in human umbilical endothelial cells[J]. Hormone Molecular Biology and Clinical Investigation,2020,41(4):20200009. doi: 10.1515/hmbci-2020-0009 [15] Zhao Y,Lu N,Zhang Y,et al. High glucose induced rat aorta vascular smooth muscle cell oxidative injury: Involvement of protein tyrosine nitration[J]. Journal of Physiology and Biochemistry,2011,67(4):539-549. doi: 10.1007/s13105-011-0099-x [16] Liu J,Wu J,Sun A,et al. Hydrogen sulfide decreases high glucose/palmitate-induced autophagy in endothelial cells by the Nrf2-ROS-AMPK signaling pathway[J]. Cell & Bioscience,2016,6(1):1-17. [17] Xu K,Liu X,Ke Z,et al. Resveratrol modulates apoptosis and autophagy induced by high glucose and palmitate in cardiac cells[J]. Cellular Physiology and Biochemistry,2018,46(5):2031-2040. doi: 10.1159/000489442 [18] De Jager J,Kooy A,Schalkwijk C,et al. Long‐term effects of metformin on endothelial function in type 2 diabetes: A randomized controlled trial[J]. Journal of Internal Medicine,2014,275(1):59-70. doi: 10.1111/joim.12128 [19] Van der Aa M P,Elst M,Van De Garde E,et al. Long-term treatment with metformin in obese,insulin-resistant adolescents: Results of a randomized double-blinded placebo-controlled trial[J]. Nutrition & Diabetes,2016,6(8):e228. [20] He X,Chen X,Wang L,et al. Metformin ameliorates Ox-LDL-induced foam cell formation in raw264.7 cells by promoting ABCG-1 mediated cholesterol efflux[J]. Life Sciences,2019,216:67-74. doi: 10.1016/j.lfs.2018.09.024 [21] Gopoju R,Panangipalli S,Kotamraju S. Metformin treatment prevents SREBP2-mediated cholesterol uptake and improves lipid homeostasis during oxidative stress-induced atherosclerosis[J]. Free Radical Biology and Medicine,2018,118:85-97. doi: 10.1016/j.freeradbiomed.2018.02.031 [22] You G,Long X,Song F,et al. Metformin activates the AMPK-mTOR pathway by modulating lncRNA TUG1 to induce autophagy and inhibit atherosclerosis[J]. Drug Design,Development and Therapy,2020,14:457. doi: 10.2147/DDDT.S233932 [23] Faghfouri A H,Khajebishak Y,Payahoo L,et al. PPAR-gamma agonists: Potential modulators of autophagy in obesity[J]. European Journal of Pharmacology,2021,912:174562. doi: 10.1016/j.ejphar.2021.174562 [24] Wang H,Wang A,Wang X,et al. AMPK/PPAR-γ/NF-κB axis participates in ROS-mediated apoptosis and autophagy caused by cadmium in pig liver[J]. Environmental Pollution,2022,294:118659. doi: 10.1016/j.envpol.2021.118659 -






 下载:
下载: