Application of Gastric Antrum Ultrasound in Assessing the Aspiration Risk during Pediatric Emergency Surgery
-
摘要:
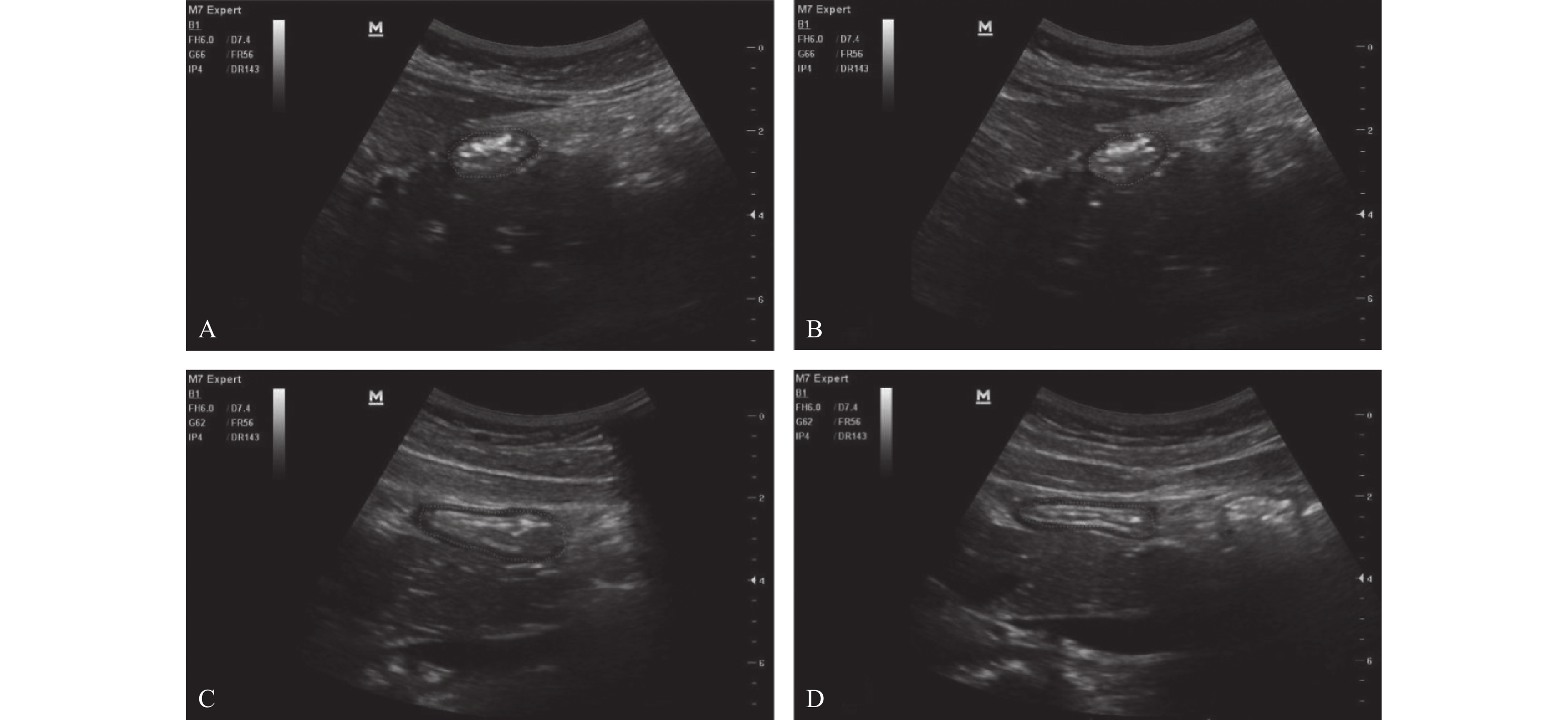
目的 探讨即时胃窦部超声检查在小儿急诊手术误吸风险评估中的应用。 方法 选择湖北省荆州市中心医院2020年12月至2021年12月的急诊小儿手术120例,年龄1~12岁,ASA分级I~III级,拟行外科手术治疗,首先根据是否符合美国麻醉医师协会2017年发布的禁饮禁食指南,对患儿进行临床胃排空评估,将患儿分为临床空腹(CE组)和临床饱胃(CF组),然后利用迈瑞M7超声,对小儿胃窦部进行胃内容物的定性和定量评估,将患儿分为超声空腹(UE组)和超声饱胃(UF组),记录临床和超声2种评估方法的一致性。检测右侧卧位下小儿胃管吸引前和吸引后胃窦部横截面积(cross-sectional area,CSA),记录胃管吸引前后CSA的变化,术前小儿的进食种类和进食量,进食与超声检查之间的时间间隔。 结果 最终纳入108例小儿进行了统计分析,临床和超声判断胃排空结果一致性较差,超声和临床均判断为空腹92例(85.2%),超声判断空腹,临床判断饱胃4例(3.7%),超声判断饱胃,临床判断空腹9例(8.3%),超声和临床均判断为饱胃3例(2.8%),(kappa=0.255,P=0.006)。患儿胃管吸引前的进食量与胃窦部CSA存在较好相关性(r =0.840,P<0.05)。吸引前UF组患儿胃窦部CSA明显大于UE组(P<0.05),吸引后UF组患儿胃窦部CSA与UE组无明显差异(P=0.324)。UF组患儿进食以配方奶和高脂肪食物居多,且胃管吸引量,进食量多于UE组(P<0.05),UF组患儿超声检查间隔时间短于UE组(P<0.05)。2组患儿术后呕吐的发生率分别为8.3%和5.2%,差异无统计学意义(P=0.674)。 结论 急诊手术患儿术前行即时胃窦部超声检查结合患儿的进食种类和进食量,可以有效帮助麻醉医师在紧急情况下做出是否饱胃的判断,以便及时调整麻醉策略,选择合适的气道管理方式。 Abstract:Objective To investigate the application of point-of-care gastric antrum ultrasonography in the risk assessment of aspiration in children undergoing emergency surgery. Methods A total of 120 cases of pediatric emergency surgery in Jingzhou Central Hospital of Hubei Province from December 2020 to December 2021, aged 1-12 years, American Society of Anesthesiologists physical status I-III, scheduled for surgical treatment, were selected. First, according to whether it met the fasting guidelines issued by the American Society of Anesthesiologists in 2017, the clinical gastric emptying of the children were evaluated. The children were divided into clinical fasting group(CE group) and clinical full group(CF group), and then Mindray M7 ultrasound was used to qualitatively and quantitatively evaluate the gastric contents in the gastric antrum. The children were divided into ultrasound empty group(UE group) and ultrasound full group(UF group), and the consistency of clinical and ultrasound evaluation methods was recorded. The cross-sectional area(CSA) of the gastric antrum was measured before and after gastric tube suction in children in the right lateral position. The changes of CSA before and after gastric tube suction, the type and amount of food eaten before surgery, and the time interval between eating and ultrasound examination were recorded. Results A total of 108 children were finally included for statistical analysis. The consistency between clinical and ultrasound examination was poor, 92 cases(85.2%) were judged as fasting by both ultrasound and clinical. 4 cases(3.7%) were judged as fasting by ultrasound but full stomach by clinical examination. 9 cases(8.3%) were judged as full stomach by ultrasound but fasting by clinical examination. 3 cases(2.8%) were judged as full stomach by both ultrasound and clinical, (kappa=0.255, P=0.006). There was a well correlation between food intake and CSA in gastric antrum before gastric tube aspiration(r =0.840, P<0.05). Before aspiration, the gastric antrum CSA in the UF group was significantly larger than the UE group(P<0.05); After suction, there was no significant difference in gastric antrum CSA between the two groups(P=0.324). The UF group consumed more formula milk and high-fat food, the amount of food suctioned by the gastric tube and the food intake were more than UE group(P<0.05), The ultrasound interval time in the UF group was shorter than the UE group(P<0.05). The incidence of vomiting in the two groups was 8.3% and 5.2% respectively, and there was no significant difference between the two groups(P=0.674). Conclusion Preoperative gastric antral ultrasonography combined with the type and amount of food intake in children undergoing emergency surgery can effectively help anesthesiologists to make an appropriate judgment of whether the stomach is full under emergency circumstances, so as to adjust the anesthesia strategy in time and choose the appropriate airway management. -
Key words:
- Gastric ultrasonography /
- Pediatric emergency surgery /
- Aspiration /
- Fasting
-
表 1 2组患儿一般资料比较(
$ \bar{x}\pm s $ )Table 1. Comparison of general data between two groups of patients(
$ \bar{x}\pm s $ )指标 UE组
(n = 96)UF组
(n = 12)t/χ2 P 男/女(n) 68/28 7/5 0.307 0.580 年龄(岁) 7.39 ± 2.18 8.00 ± 1.86 −0.933 0.353 BMI(kg/m2) 16.55 ± 2.58 16.37 ± 1.95 0.376 0.708 手术时间(min) 48.33 ± 9.37 45.00 ± 6.74 1.193 0.236 表 2 临床和超声判断胃容量结果一致性评价[n(%)]
Table 2. Consistency of gastric volume measured by clinical and ultrasound[n(%)]
临床判断 超声判断 kappa P UE组 UF组 CE组 92(85.2) 9(8.3) 0.255 0.006* CF组 4(3.7) 3(2.8) *P<0.05。 表 3 超声检查空腹和饱胃相关指标比较[M(Q1,Q3)/n(%)]
Table 3. Comparison of related parameters between UE and UF[M(Q1,Q3)/n(%)]
指标 UE组
(n = 96)UF组
(n = 12)Z/t/χ2 P BCSA(cm2) 2.10(1.80,2.80) 3.90(3.80,4.20) 15.088 <0.001* ACSA(cm2) 1.80(1.70,1.90) 1.85(1.80,2.00) 0.973 0.324 胃管吸引量(mL/kg) 0.3(0.2,0.6) 1.2(1.0,1.3) 23.160 <0.001* 进食种类(1/2/3/4)(n) (64/30/2/0) (1/3/8/0) 34.900 <0.001* 进食至超声检查间隔(h) 5.92 ± 1.06 2.42 ± 0.52 11.208 <0.001* 进食量(g) 120(100,150) 225(203,238) 16.255 <0.001* 呕吐[n(%)] 5(5.2) 1(8.3) 0.177 0.674 BCSA:胃管吸引前CSA,ACSA:胃管吸引后CSA,胃管吸引量和进食量均采用[M(Q1,Q3)]表示;*P < 0.05。 -
[1] Abdulla S. Pulmonary aspiration in perioperative medicine[J]. Acta Anaesthesiol Belg,2013,64(1):11-13. [2] Beck C E,Rudolp D,Becke-jakob K,et al. Real fasting times and incidence of pulmonary aspiration in children: Results of a German prospective multicenter observational study[J]. Paediatr Anaesth,2019,29(10):1040-1045. doi: 10.1111/pan.13725 [3] 董秀云,沈文娟,姚鹏,等. 床旁胃超声指导自发性脑出血患者肠内营养治疗的效果[J]. 中华麻醉学杂志,2022,42(12):1500-1503. [4] Bouvet L,Desgranges F P,Aubergy C,et al. Prevalence and factors predictive of full stomach in elective and emergency surgical patients: A prospective cohort study[J]. Br J Anaesth,2017,118(3):372-379. doi: 10.1093/bja/aew462 [5] Horvath B,Kloesel B,Todd M M,et al. The evolution,current value,and future of the American society of anesthesiologists physical status classification system[J]. Anesthesiology,2021,135(5):904-919. doi: 10.1097/ALN.0000000000003947 [6] Jeffrey L,Madhulika A,Richard T,et al. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: Application to healthy patients undergoing elective procedures[J]. Anesthesiology,2017,126(3):376-393. doi: 10.1097/ALN.0000000000001452 [7] Perlas A,Arzola C,Van de Putte P. Point-of-care gastric ultrasound and aspiration risk assessment: A narrative review[J]. Can J Anaesth,2018,65(4):437-448. doi: 10.1007/s12630-017-1031-9 [8] 杨天意,王杭,袁阳,等. 床旁胃窦超声评估特殊人群胃排空及预防反流误吸的研究进展[J]. 临床麻醉学杂志,2023,39(6):636-640. [9] Moake M M,Jackson B F,Presley B C. Point-of-care ultrasound to assess gastric content[J]. Pediatr Emerg Care,2020,36(8):404-410. doi: 10.1097/PEC.0000000000001939 [10] Johnson E J,Morbach J,Blake C,et al. Sensitivity and specificity of gastric ultrasonography in determination of gastric contents[J]. AANA J,2021,89(1):9-16. [11] 孙震,卜亚男,吕晶,等. 超声评估全麻诱导不同通气压力对幼儿胃胀气的影响[J]. 临床麻醉学杂志,2016,32(3):230-233. [12] Kim E H,Yoon H C,Lee J H,et al. Prediction of gastric fluid volume by ultrasonography in infants undergoing general anaesthesia[J]. Br J Anaesth,2021,127(2):275-280. doi: 10.1016/j.bja.2021.03.039 [13] Moake M M,Presley B C,Hill J G,et al. Point-of-care ultrasound to assess gastric content in pediatric emergency department procedural sedation patients[J]. Pediatr Emerg Care,2022,38(1):178-186. doi: 10.1097/PEC.0000000000002198 [14] 张瑶,袁红梅,秦香,等. 不同饮食对低风险产妇硬膜外分娩镇痛及胃排空时间的影响[J]. 临床麻醉学杂志,2021,37(9):937-940. [15] 黎佳,孙凯,严敏. 床旁胃超声在特殊人群临床应用研究进展[J]. 国际麻醉学与复苏杂志,2021,42(1):80-82. [16] Bouvet L,Mazoit J X,Chassard D,et al. Clinical assessment of the ultrasonographic measurement of antral area for estimating preoperative gastric content and volume[J]. Anesthesiology,2011,114(5):1086-1092. doi: 10.1097/ALN.0b013e31820dee48 [17] Spencer A O,Walker A M,Yeung A K,et al. Ultrasound assessment of gastric volume in the fasted pediatric patient undergoing upper gastrointestinal endoscopy: Development of a predictive model using endoscopically suctioned volumes[J]. Paediatr Anaesth,2015,25(3):301-308. doi: 10.1111/pan.12581 [18] Moser J J,Walker A M,Spencer A O,et al. Point-of-care paediatric gastric sonography: Can antral cut-off values be used to diagnose an empty stomach[J]. Br J Anaesth,2017,119(5):943-947. doi: 10.1093/bja/aex249 [19] Peng J,Tang M,Liu LL,et al. Diagnostic accuracy of ultrasonography for detecting gastric tube placement: An updated meta-analysis[J]. Eur Rev Med Pharmacol Sci,2022,26(17):6328-6339. [20] 黄丽君,严敏,张冯江,等. 胃超声检查评估急诊剖宫产产妇胃排空的效果[J]. 临床麻醉学杂志,2019,35(4):373-376. [21] 万绪娟,周建敏,谢红. 超声下评估患儿术前胃内容物的效果[J]. 临床麻醉学杂志,2020,36(1):77-79. [22] Bouvet L,Chassard D. Ultrasound assessment of gastric content in the obese patient: One more step for patient safety[J]. Anesth Analg,2014,119(5):1017-1018. doi: 10.1213/ANE.0000000000000403 [23] Kruisselbrink R,Arzola C,Jackson T,et al. Ultrasound assessment of gastric volume in severely obese individuals: A validation study[J]. Br J Anaesth,2017,118(1):77-82. doi: 10.1093/bja/aew400 [24] 孟阳,朱玲玲,陈凌,等. 足月新生儿呕吐135例病因分析[J]. 现代医学,2016,44(1):95-97. [25] Desgranges F P,Gagey Riegel A C,Aubergy C,et al. Ultrasound assessment of gastric contents in children undergoing elective ear,nose and throat surgery: A prospective cohort study[J]. Anaesthesia,2017,72(11):1351-1356. doi: 10.1111/anae.14010 -






 下载:
下载: