Effect Analysis of Transurethral Resection of Prostate Combined with Endocrine Therapy for Advanced Prostate Cancer
-
摘要:
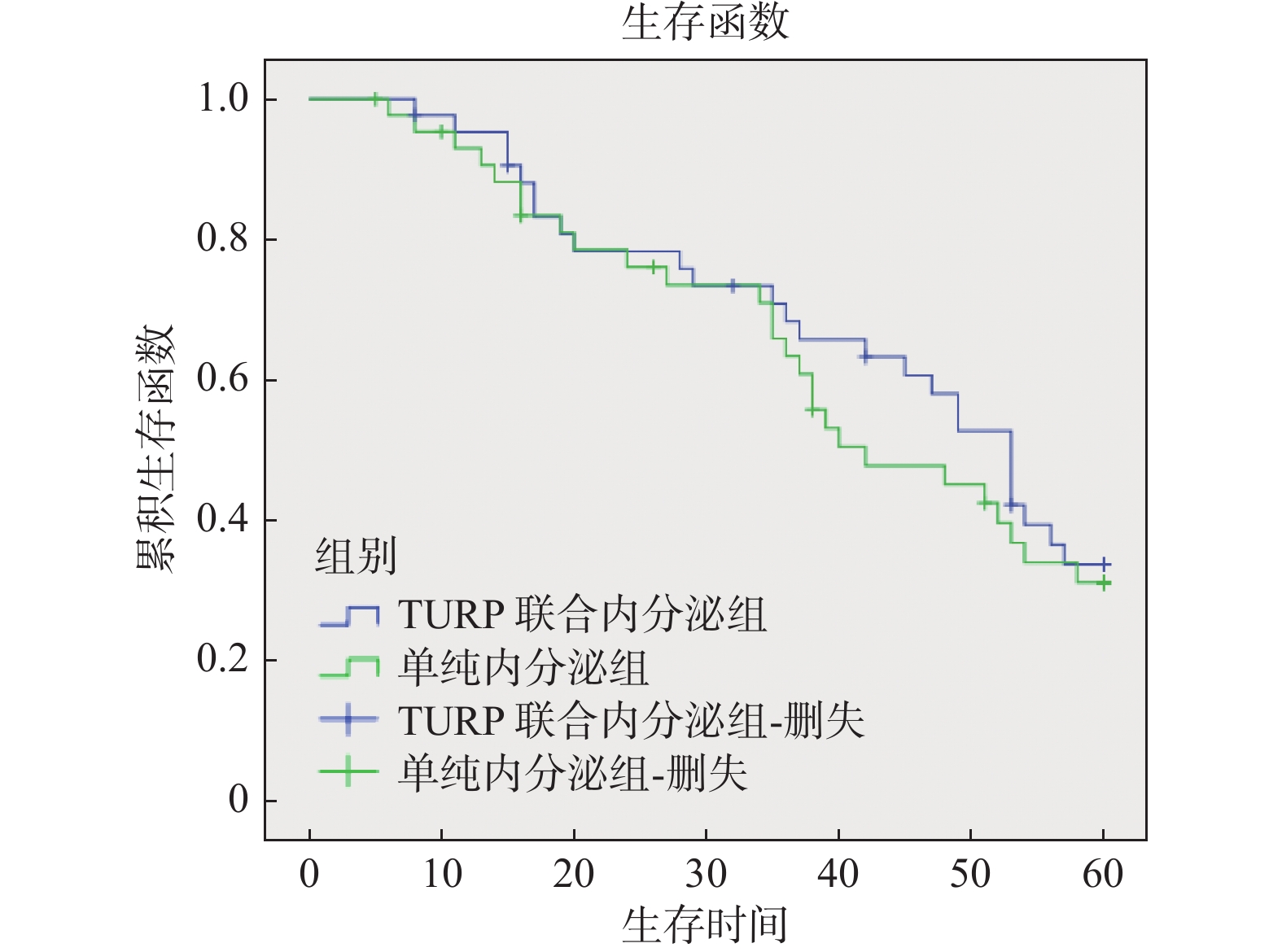
目的 探讨经尿道前列腺电切术联合内分泌治疗对于中晚期前列腺癌患者的疗效与安全性。 方法 回顾性分析2014年1月至2017年12月期间收治87例伴有排尿困难症状的T3b、T4期晚期前列腺癌患者,分为2组。TURP组(n = 48),接受经尿道前列腺电切术治疗,术后再辅以规律内分泌治疗;对照组(n = 39),单纯予以规律内分泌治疗。对比分析2组治疗前后前列腺特异性抗原、最大尿流率、残余尿量、国际前列腺症状评分(IPSS评分)、5 a生存率等指标。 结果 TURP组术后3个月排尿困难症状缓解明显,各项指标较术前明显改善。PSA指标也较术前明显下降。在治疗3个月后,TURP组的IPSS、 Qmax、 RV、 PSA指标较对照组明显改善(P < 0.05)。2组患者在接受规范的治疗后PSA均值都逐渐下降,在刚开始治疗的12个月里,TURP组较对照组PSA均值下降更明显,但在治疗12个月后,2组的PSA均值对比差异无统计学意义(P = 0.056)。对2组患者随访5 a,对比分析发现2组的生存差异无统计学意义(P = 0.734)。 结论 TURP联合规律内分泌治疗能有效改善前列腺癌患者排尿困难症状,明显提升患者生活质量,同时并不会影响患者5 a生存率,是一种安全有效的治疗方式。 Abstract:Objective To evaluate the efficacy and safety of transurethral resection of Prostate(TURP) combined with endocrine therapy in patients with advanced prostate cancer. Methods A retrospective analysis was conducted on 87 cases of late-stage prostate cancer with dysuria admitted between January 2014 and December 2017. We divided them into 2 groups. TURP group (n = 48) received transurethral resection of prostate, followed by regular endocrine therapy. The control group (n = 39) was only given regular endocrine therapy. Comparative analysis of indicators such as prostate-specific antigen before and after treatment, maximum urinary flow rate, residual urine volume, International Prostate Symptom Score(IPSS), and 5-year survival rate was performed between the two groups. Results Three months after TURP surgery, the symptoms of urinary difficulty significantly improved, and various indicators showed significant improvement compared to before the surgery. PSA levels also notably decreased compared to before the surgery. After 3 months of treatment, the TURP group showed significant improvements in IPSS, Qmax, RV, and PSA indicators compared to the control group(P < 0.05). Both groups of patients experienced a gradual decrease in PSA levels after receiving standardized treatment. In the first 12 months of treatment, the PSA levels in the TURP group decreased more significantly compared to the control group, but after 12 months of treatment, the comparison difference was not statistically significant in the PSA levels between the two groups(P = 0.056). A 5-year follow-up comparison of the two groups of patients revealed that there was no statistically significant difference in survival (P = 0.734). Conclusion Transurethral resection of Prostate(TURP) combined with regular endocrine therapy can effectively improve the dysuria in prostate cancer patients, improve the quality of life of patients, and will not affect the five-year survival rate. TURP is a safe and effective treatment for advanced prostate cancer. -
表 1 2组治疗前基线资料对比($\bar x \pm s$)
Table 1. Clinical parameters of the patients before treatment of the two groups($\bar x \pm s$)
组别 IPSS
(分)Qmax
(mL/min)RV
(mL)PSA
(ng/mL)AGE
(岁)TURP组 20.2±2.3. 5.4±1.4 124.9±18.5 34.15±8.14 67.5±8.4 对照组 19.8±5.4 5.7±2.3 113.6±25.4 31.22±6.53 63.2±6.2 t 3.268 1.250 3.157 2.915 3.715 P 0.258 0.732 0.325 0.313 0.682 IPSS: international prostate symptom score,国际前列腺症状评分; Qmax:maximum urinary flow rate,最大尿流率;RV:residual urine volume,残余尿量;PSA:prostate-specific antigen,前列腺特异性抗原;AGE:年龄。 表 2 TURP组治疗前及术后3个月指标变化($ \bar x \pm s $)
Table 2. Clinical parameters of the patients before and after 3-month treatment in TURP group($\bar x \pm s $)
TURP组 IPSS
(分)Qmax
(mL/min)RV
(mL)PSA
(ng/mL)TURP术前 20.2±2.3 5.4±1.4 124.9±18.5 34.15±8.14 TURP术后 2.4±1.7 18.4±9.3 12.6±2.3 3.72±1.21 t 2.381 2.586 4.372 2.862 P 0.003* 0.011* 0.007* 0.006* *P < 0.05。 表 3 TURP组和对照组治疗后3个月变化($\bar x \pm s$)
Table 3. Clinical parameters of the patients after 3-month treatment between the two groups ($\bar x \pm s$)
组别 IPSS
(分)Qmax
(mL/min)RV
(mL)PSA
(ng/mL)TURP组 2.4±1.7 18.4±9.3 12.6±2.3 3.2±1.2 对照组 8±3.8 10.7±6.8 56.7±4.6 5.6±2.3 t 3.641 2.853 6.571 1.283 P 0.007* 0.003* 0.012* 0.025* *P < 0.05。 表 4 TURP组和对照组治疗后PSA均值变化[$\bar x \pm s$,ng/mL]
Table 4. Changes of mean PSA after treatment in the two groups[$\bar x \pm s$,ng/mL]
组别 治疗前 1月 2月 3月 12月 24月 TURP组 34.15±8.14 13.72±6.31 10.24±5.31 3.23±1.21 2.32±1.40 1.58±0.31 对照组 31.22±6.53 28.45±1.92 24.61±5.43 5.64±2.32 2.52±1.31 1.46±0.52 t 8.543 5.431 3.591 7.216 8.623 7.615 P 0.077 0.003* 0.015* 0.009* 0.056 0.076 *P < 0.05。 -
[1] Oelke M,Bachmann A,Descazeaud A,et al. EAU Guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction[J]. Eur Urol,2020,64(1):118-140. [2] Wong M C,Goggins W B,Wang H H,et al. Global incidence and mortality for prostate cancer: Analysis of temporal patterns and trends in 36 countries[J]. Eur Urol,2016,70(5):862-874. doi: 10.1016/j.eururo.2016.05.043 [3] 庞昆,梁清,陈波,等. 经尿道前列腺等离子电切术后晚期前列腺癌患者相关急性尿潴留的临床治疗方案研究[J]. 中华男科学杂志,2023,29(1):25-30. doi: 10.13263/j.cnki.nja.2023.01.004 [4] 黄智峰,钟喨,赖海标,等. 以尿潴留为首发表现的前列腺癌临床分析(附43例)[J]. 现代肿瘤医学,2019,27(7):1184-1188. [5] 任虎,周伟,徐立. 经尿道姑息性手术治疗晚期前列腺癌的效果及对患者VAS评分的影响[J]. 中国性科学,2019,28(3):7-10. [6] 何正宇,余闫宏,申杰,等. 1470nm激光汽化术通道法治疗晚期前列腺癌并膀胱出口梗阻[J]. 中华腔镜泌尿外科杂志(电子版),2018,12(6):411-414. doi: 10.3877/cma.j.issn.1674-3253.2018.06.012 [7] 黄海源,李金喜,陈政锦. 三联疗法治疗中晚期前列腺癌的临床观察[J]. 中国肿瘤外科杂志,2019,11(6):457-459. [8] 莫益江,赵桂熔,刘文龙,等. 经尿道前列腺电切术联合雄激素剥夺治疗晚期前列腺癌的研究进展[J]. 汕头大学医学院学报,2022,35(3):185-187. [9] Forman J D,Order S E,Zinreich E S,et al. The correlation of pretreatment transurethral resection of prostatic cancer with tumor dissemination and disease-free survival. A univariate and multivariate analysis[J]. Cancer,1986,58(8):1770-1778. doi: 10.1002/1097-0142(19861015)58:8<1770::AID-CNCR2820580832>3.0.CO;2-U [10] Krupski T L,Stukenborg G J,Moon K,et al. The relationship of palliative transurethral resection of the prostate with disease progression in patients with prostate cancer[J]. BJU International,2010,106(10):.1477-1483. doi: 10.1111/j.1464-410X.2010.09356.x [11] Young S C,Jeman R,Dalsan Y,et al. Oncological effect of palliative transurethral resection of the prostate in patients with advanced prostate cancer: A propensity score matching study[J]. Journal of Cancer Research and Clinical Oncology,2018,144(4):.751-758. doi: 10.1007/s00432-018-2597-5 [12] 黄凤鸣,李晓红,梁勇. 伴骨转移前列腺癌患者内分泌治疗后出现早期CRPC的危险因素分析[J]. 中华男科学杂志,2018,24(8):690-694. [13] 王林,庞鹏,刘泽龙,等. 经尿道前列腺电切术对前列腺癌合并膀胱出口梗阻患者前列腺症状指标、血清学指标及生存情况的影响[J]. 癌症进展,2022,20(11):1168-1171. [14] 邱腾,胡小桃. 经尿道前列腺电切术联合内分泌治疗晚期前列腺癌的临床疗效及不良反应分析[J]. 滨州医学院学报,2019,42(6):421-423. [15] Bai D S,Chen P,Qian J J,et al. Effect of marital status on the survival of patients with gallbladder cancer treated with surgical resection: A population-based study[J]. Oncotarget,2017,8(16):26404-26413. doi: 10.18632/oncotarget.15476 [16] 崔宁,马永康,马德青,等. 经尿道前列腺癌电切术联合手术去势对前列腺癌患者前列腺功能及TNF-α、IGF-1、PSA水平的影响[J]. 临床医学研究与实践,2023,8(6):62-64. doi: 10.19347/j.cnki.2096-1413.202306018 [17] 许宁,甄晓玲,张祥. 经尿道前列腺癌电切术患者血清VEGF、TGF-β1的水平变化及其临床意义[J]. 海军医学杂志,2019,40(2):147-150. doi: 10.3969/j.issn.1009-0754.2019.02.018 [18] Pelletier J,Cyr S J,Julien A S,et al. Contemporary outcomes of palliative transurethral resection of the prostate in patients with locally advanced prostate cancer[J]. Urol Oncol,2018,36(8):363.e7-363.e11. doi: 10.1016/j.urolonc.2018.05.004 [19] 周俊,陈如,马锋. 经尿道前列腺等离子电切术联合内分泌疗法治疗晚期前列腺癌合并膀胱出口梗阻的临床疗效观察[J]. 国际泌尿系统杂志,2020,40(2):239-242. [20] Crain D S, Amling C L, Kane C J. Palliative transurethral prostate resection for bladder outlet obstruction in patients with locally advanced prostate cancer[J]. J Urol, 2004, 171(2 Pt 1): 668-671. [21] Meeks J J,Habermacher G M,Le B,et al. Delayed diagnosis of prostate cancer with neuroendocrine differentiation after laser TURP[J]. Urology,2008,72(4):948.e11-12. doi: 10.1016/j.urology.2008.01.007 -






 下载:
下载: