The Predictive Value of MMP-9 the and NLR Values for Bleeding Transformation after the Revascularization in Acute Ischemic Stroke
-
摘要:
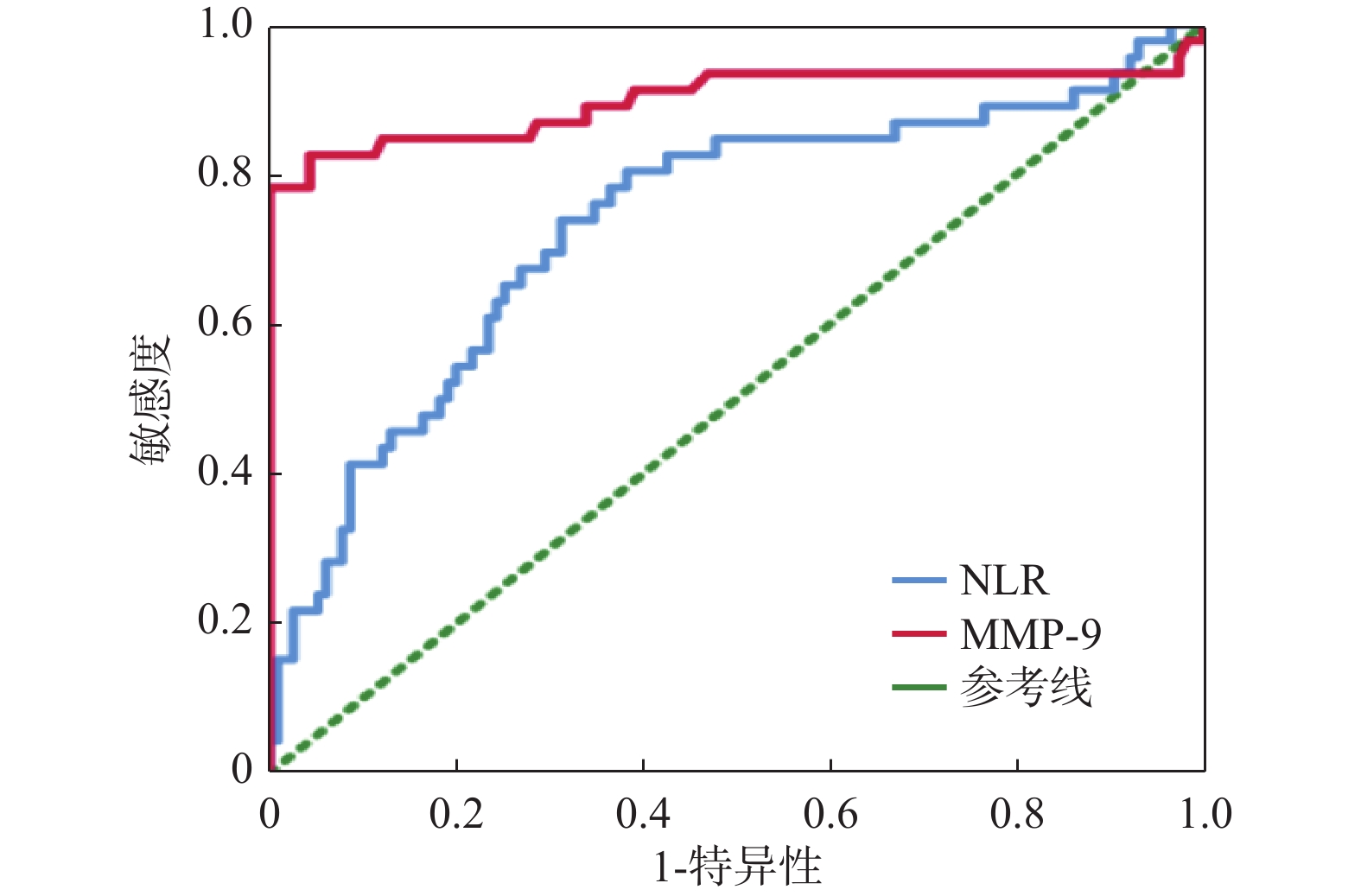
目的 研究急性缺血性卒中(acute ischemic stroke,AIS)血运重建前后金属基质蛋白酶9(matrixmetalloproteinase-9,MMP-9)、中性粒细胞/淋巴细胞比值(NLR值)的变化与出血转化的相关性,以期寻找预测AIS患者血运重建后出血转化的生物标记物。 方法 收集2022年2月至2022年12月曲靖市第一人民医院卒中中心收治的AIS并接受血运重建治疗(静脉溶栓、血管内治疗、同时接受静脉溶栓和血管内治疗)的患者161例,其中出血转化组46例,非出血转化组115例,通过比较血运重建后出血转化组与非出血转化组的一般信息、血运重建前后NLR值及MMP-9等指标。 结果 2组患者一般资料对比,除C反应蛋白存在差异外(P < 0.001),余临床资料对比差异无统计学意义(P > 0.05),出血转化组在治疗前白细胞、中性粒细胞、中性粒细胞百分比、中性粒细胞绝对值、淋巴细胞绝对值、NLR、MMP-9较非出血转化明显升高,差异有统计学意义(P < 0.05),血运重建后血常规各项指标、MMP-9较血运重建前明显升高,出血转化组较非出血转化组升高更加明显,差异有统计学意义(均P < 0.001),ROC曲线示NLR、MMP-9预测AIS血运重建后出血转化的曲线下面积(AUC)为0.74、0.90。 结论 NLR、MMP-9与AIS患者血运重建后出血转化发病风险相关,可作为出血转化风险预测因子。 -
关键词:
- 急性缺血性卒中 /
- 金属基质蛋白-9 /
- 中性粒细胞与淋巴细胞比值 /
- 血运重建
Abstract:Objective To study the correlation between the changes of matrix metalloproteinase-9(MMP-9) and neutrophil/lymphocyte ratio(NLR) before and after the revascularization of acute ischemic stroke(AIS), so as to find biomarkers to predict the bleeding transformation risk of AIS patients. Methods From February 2022 to December 2022, 161 patients admitted to the Stroke Center of Qujing Hospital Affiliated to Kunming Medical University with AIS werre divided in to the hemorrhagic transformation group and the non-hemorrhagic transformation groupand treated with revascularization(intravenous thrombolysis, endovascular treatment, combined the intravenous thrombolysis with endovascular treatment). Among them, there were 46 cases in the hemorrhagic transformation group and 115 cases in the non hemorrhagic transformation group. And the general data, NLR value and MMP-9 before and after the revascularization were compared between the two groups. Results There was no statistical difference in general data between the two groups(all P > 0.05) except for C-reactive protein in hemorrhagic transformation group and in non-hemorrhagic transformation group(P < 0.001). The white blood cells, neutrophils, neutrophil percentage, neutrophil absolute value, lymphocyte absolute value, NLR and MMP-9 value in hemorrhagic transformation group were significantly higher than those in non-hemorrhagic transformation group before the treatment and there was a statistical significance(P < 0.05).After revascularization, the indexes of blood routine and MMP-9 were significantly higher than those before the revascularization, and the increase in hemorrhagic transformation group was more obvious than that in non-hemorrhagic transformation group and there was a statistical significance(P < 0.001), The ROC curve showed that the area under the curve(AUC) of NLR and MMP-9 predicting bleeding transformation after AIS revascularization were 0.74 and 0.90. Conclusion NLR, MMP-9 are associated with the risk of bleeding transformation in AIS patients after the revascularization and can they can be used as the predictive factors for bleeding transformation risk. -
表 1 一般资料比较[($ \bar x \pm s $)/n (%)]
Table 1. General date comparison[($ \bar x \pm s $)/n (%)]
指标 非出血转化组(n=115) 出血转化组(n=46) χ2/Z/t P 男性 74(64.35) 29(63.04) 0.024 0.876 年龄(岁) 64.88 ± 10.62 63.65 ± 15.37 0.496 0.876 高血压 71(61.74) 24(52.17) 1.243 0.265 糖尿病 21(18.26) 8(17.39) 0.017 0.897 心房颤动 17(14.78) 8(17.39) 0.170 0.680 冠心病 10(8.70) 4(8.70) 0.001 0.999 同型半胱氨酸(μmol/L) 14.00(11.00~18.00) 13.50(10.00~17.25) −1.047 0.295 高密度脂蛋白(mmol/L) 1.17 ± 0.28 1.21 ± 0.24 −0.859 0.392 低密度脂蛋白(mmol/L) 2.93 ± 0.80 2.88 ± 0.70 0.350 0.727 总胆固醇(mmol/L) 4.57 ± 1.08 4.53 ± 0.86 0.240 0.810 甘油三酯(mmol/L) 1.32(1.00~1.97) 1.12(0.97~1.53) −1.675 0.094 总胆红素(μmol/L) 13.40(9.80~17.90) 15.90(9.45~22.32) −1.166 0.244 C反应蛋白(mg/L) 2.30(1.30~5.50) 8.90(4.08~12.12) −4.763 <0.001*** 脂蛋白a(mg/L) 127.00(65.00~213.00) 109.50(66.75~265.75) −0.305 0.760 *P<0.05。 表 2 2组治疗前血常规、MMP-9比较($ \bar x \pm s $)
Table 2. Comparison of blood routine results and MMP-9 between two group before treatment($ \bar x \pm s $)
指标 非出血转化组 出血转化组 Z/t P 白细胞(×109/L) 8.30 ± 2.75 10.24 ± 4.20 −2.892 0.005* 中性粒细胞百分比(%) 68.42 ± 11.35 77.86 ± 12.04 −4.689 <0.001* 淋巴细胞百分比(%) 23.70(15.50~31.80) 13.45(8.68~19.28) −4.592 <0.001* 中性粒细胞绝对值(×109/L) 5.41(3.72~7.47) 7.40(5.48~11.12) −3.596 <0.001* 淋巴细胞绝对值(×109/L) 1.69(1.31~2.29) 1.32(0.93~1.76) −3.705 <0.001* NLR 2.94(1.94~5.06) 6.03(3.84~9.95) −4.655 <0.001* MMP-9(ng/mL) 21.09 ± 6.80 58.06 ± 32.54 −7.638 <0.001* *P<0.05。 表 3 2组患者治疗后血常规、MMP-9比较($ \bar x \pm s $)
Table 3. Comparison of blood routine results and MMP-9 between two group after treatment($ \bar x \pm s $)
指标 非出血转化组 出血转化组 t P 白细胞(×109/L) 8.29 ± 2.74 10.85 ± 3.80 −4.155 <0.001* 中性粒细胞百分比(%) 71.78 ± 10.96 81.81 ± 7.93 −6.456 <0.001* 淋巴细胞百分比(%) 18.50(12.80~27.40) 10.10(7.30~16.38) −5.297 <0.001* 中性粒细胞绝对值(×109/L) 5.71(3.97~7.67) 8.66(6.16~11.86) −4.805 <0.001* 淋巴细胞绝对值(×109/L) 1.40(1.04~1.88) 1.14(0.79~1.14) −3.347 0.001* NLR 4.02(2.26~6.35) 8.28(4.61~12.13) −5.287 <0.001* MMP-9(ng/mL) 61.45 ± 27.90 112.01 ± 67.26 −4.931 <0.001* *P<0.05。 表 4 NLR和MMP-9对血运重建后出血转化的预测价值
Table 4. The predictive value of NLR and MMP-9 for bleeding transformation after revascularization
指标 AUC(95%CI) 灵敏度 特异度 P 阈值 NLR 0.74(0.64~0.83) 0.83 0.67 <0.001* 3.10 MMP-9 0.90(0.82~0.97) 0.83 0.96 <0.001* 32.15 *P<0.05。 -
[1] 王拥军,李子孝,谷鸿秋,等. 中国卒中报告2020(中文版)[J]. 中国卒中杂志,2022,17(5):433-477. doi: 10.3969/j.issn.1673-5765.2022.05.001 [2] Liu C,Xie J,Sun S,et al. Hemorrhagic transformation after tissue plasminogen activator treatment in acute ischemic stroke[J]. Cell Mol Neurobiol,2022,42(3):621-646. doi: 10.1007/s10571-020-00985-1 [3] 中华医学会神经病学分会,中华医学会神经病学分会脑血管病学组. 中国急性缺血性脑卒中诊治指南2018[J]. 中华神经科杂志,2018,51(9):666-682. [4] Yaghi S,Willey J Z,Cucchiara B,et al. Treatment and outcome of hemorrhagic transformation after intravenous alteplase in acute ischemic stroke: A scientific statement for healthcare professionals from the American Heart Association/American Stroke Association[J]. Stroke,2017,48(12):e343-e361. [5] 徐慈航,李敬伟,朱晓蕾. 急性缺血性卒中出血转化的研究进展[J]. 中国卒中杂志,2020,15(4):446-451. [6] Lei C,Wu B,Liu M,et al. Asymptomatic hemorrhagic transformation after acute ischemic stroke: Is it clinically innocuous?[J]. J Stroke Cerebrovasc Dis,2014,23(10):2767-2772. doi: 10.1016/j.jstrokecerebrovasdis.2014.06.024 [7] Yu A Y,Hill M D,Coutts S B. Should minor stroke patients be thrombolyzed? A focused review and future directions[J]. Int J Stroke,2015,10(3):292-297. doi: 10.1111/ijs.12426 [8] Zhang J,Yuan C,Deng X,et al. Efficacy and safety of endovascular treatment with or without intravenous alteplase in acute anterior circulation large vessel occlusion stroke: A meta-analysis of randomized controlled trials[J]. Neurol Sci,2022,22(9):207. [9] Wang L,Wei C,Deng L,et al. The accuracy of serum matrix metalloproteinase-9 for predicting hemorrhagic transformation after acute ischemic stroke: A systematic review and meta-analysis[J]. J Stroke Cerebrovascular Diseases,2018,27(6):1653-1665. [10] 王丹,王功锦,赵学渊,等. 血清基质金属蛋白酶9预测大血管闭塞性脑卒中患者机械取栓术后出血转化的临床研究[J]. 中华老年心脑血管病杂志,2023,25(7):720-724. doi: 10.3969/j.issn.1009-0126.2023.07.013 [11] 常青,杨宇英,薛茜,等. NLR、MMP-9对急性缺血性脑卒中静脉溶栓患者出血转化的诊断价值[J]. 中国老年学杂志,2022,42(9):2077-2081. doi: 10.3969/j.issn.1005-9202.2022.09.010 [12] 樊金宇,闫海润,路遥,等. MMP-9/TIMP-1平衡在急性缺血性脑卒中rt-PA溶栓后出血性转化中的临床应用研究[J]. 中国现代医药杂志,2023,25(3):18-22. doi: 10.3969/j.issn.1672-9463.2023.03.004 [13] Park B J,Shim J Y,Lee H R,et al. Relationship of neutrophil-lymphocyte ratio with arterial stiffness and coronary calcium score[J]. Clin Chim Acta,2011,412(11-12):925-929. doi: 10.1016/j.cca.2011.01.021 [14] Shantsila E,Lip GY. Stroke in atrial fibrillation and improving the identification of‘high-risk' patients: The crossroads of immunity and thrombosis[J]. J Thromb Haemost,2015,13(11):1968-1970. doi: 10.1111/jth.13121 [15] 朱一珂,杨君素,黄保岗,等. 急性缺血性脑卒中患者血运重建前后 NLR 值与预后相关性分析[J]. 昆明医科大学学报,2022,43(8):100-105. [16] Zhang R,Wu X,Hu W,et al. Neutrophil-to-lymphocyte ratio predicts hemorrhagic transformation in ischemic stroke: A meta-analysis[J]. Brain Behav,2019,9(9):eo1382. [17] Maestrini I,Strbian D,Gautier S,et al. Higher neutrophil counts before thrombolysis for cerebral ischemia predict worse outcomes[J]. Neurology,2015,85(16):1408-1416. doi: 10.1212/WNL.0000000000002029 [18] Goyal N,Tsivgoulis G,Chang J J,et al. Admission neutrophil-to-lymphocyte ratio as a prognostic biomarker of outcomes in large vessel occlusion strokes[J]. Stroke,2018,49(8):1985-1987. doi: 10.1161/STROKEAHA.118.021477 -






 下载:
下载: