Prospective Clinical Study of Combined Treatment of Periodontal Orthodontics for Chronic Periodontitis
-
摘要:
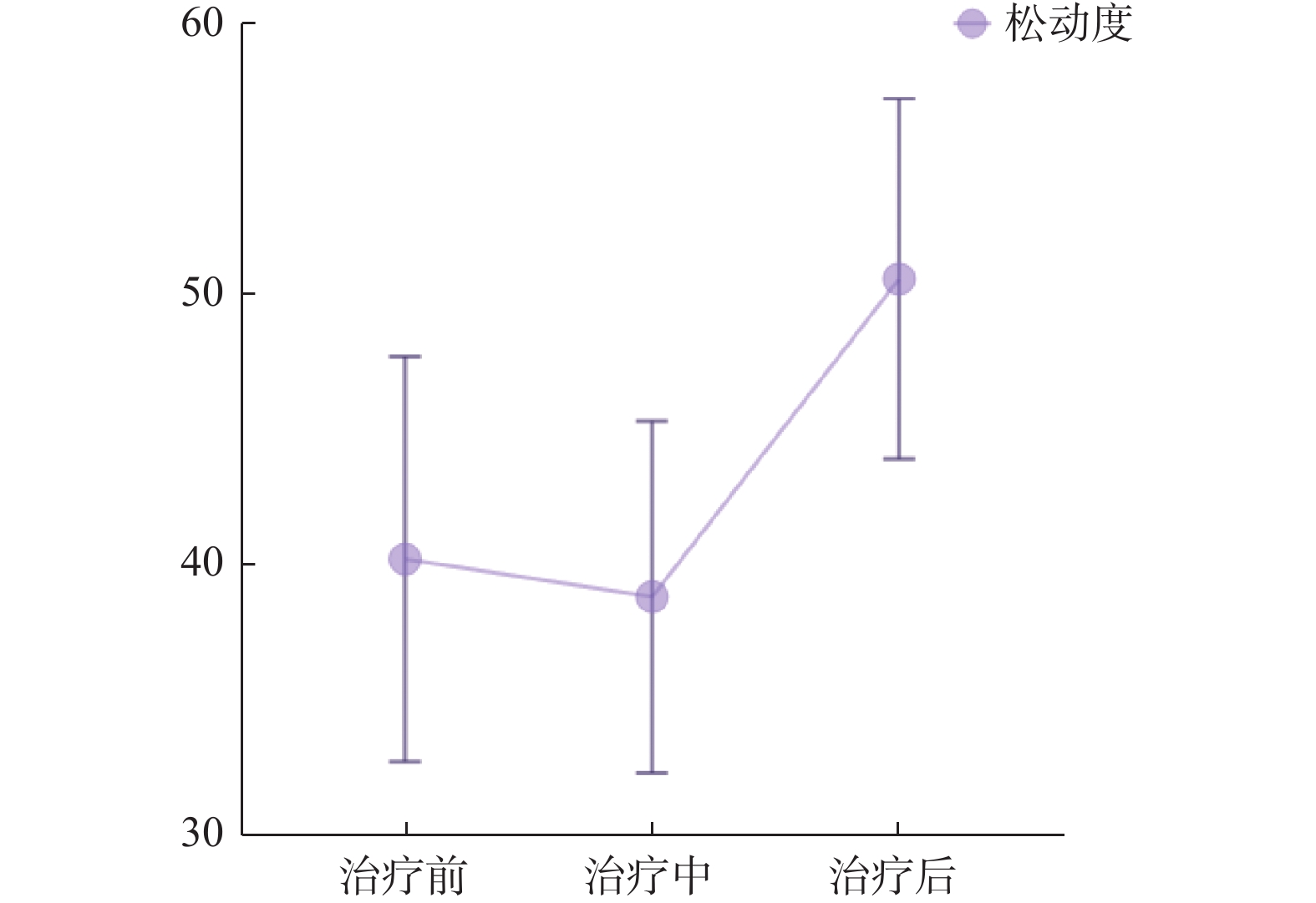
目的 探讨牙周正畸联合治疗过程中咬合力动态监测对于最终治疗效果,以及牙周支持组织改变的影响。 方法 对比20例传统牙周正畸治疗患者与20例运用T-Scan III和Anycheck数字化咬合分析系统辅助分析的牙周正畸联合治疗患者在治疗前、中、后的牙周临床指数的不同,以及实验组咬合力变化、咬合时间变化和牙松动度值变化的情况。 结果 2组患者的牙周-正畸联合治疗后牙周袋深度(PD)、附着丧失(AL)、出血指数(BI)和牙松动度明显降低(P < 0.05);对照组前后牙咬合力百分比变化明显(P < 0.05),咬合平衡改善。 结论 牙周-正畸联合治疗能很好的改善牙周炎患者牙周组织情况,T-Scan系统能很好地观察和指导调整咬合,更好地达到咬合平衡。 Abstract:Objective To investigate the effect of dynamic monitoring of occlusal force on the final therapeutic effect and the change of periodontal supporting tissue during combined periodontal orthodontic treatment. Methods The periodontal clinical index of 20 patients with traditional periodontal orthodontic treatment and 20 patients with combined periodontal orthodontic treatment assisted by T-Scan III and Anycheck digital occlusion analysis system were compared before, during and after treatment, as well as the changes of bite force, bite time and tooth mobility in the experimental group. Results The depth of periodontal pocket(PD), loss of attachment(AL), bleeding index(BI) and tooth looseness were significantly reduced after combined periodontal orthodontic treatment in both groups. In the control group, the percentage of anterior and posterior biting force changed obviously, and the occlusion force balance was improved. Conclusion The combined treatment of periodontitis and orthodontics can improve the periodontal tissue of patients with periodontitis, and T-Scan system can observe and guide the adjustment of occlusal and better achieve occlusion force balance. -
Key words:
- Periodontitis /
- Orthodontic treatment /
- Occlusion force /
- Tooth mobility
-
表 1 A组与B组牙周正畸联合治疗前中后牙周临床指数对比($ \bar x \pm s $)
Table 1. Comparison of periodontal clinical index before,middle and after periodontal orthodontic combined treatment between group A and group B($ \bar x \pm s $)
指标 时间 对照组A 实验组B t P PD(mm) 治疗前 5.12 ± 0.76 5.21 ± 0.82 −2.07 0.052 治疗中 4.96 ± 0.89 4.52 ± 0.86 4.553 < 0.001* 治疗后 4.49 ± 0.85 4.09 ± 0.85 4.381 < 0.001* AL(mm) 治疗前 4.64 ± 0.78 4.74 ± 0.88 1.986 0.062 治疗中 4.100 ± 0.80 4.38 ± 0.88 −3.472 0.003* 治疗后 3.67 ± 0.85 4.03 ± 0.85 −4.56 < 0.001* BI 治疗前 2.49 ± 0.44 5.12 ± 0.76 −29.689 < 0.001* 治疗中 1.62 ± 0.47 1.91 ± 0.43 −2.424 0.025* 治疗后 0.81 ± 0.46 0.83 ± 0.31 −0.202 0.842 *P < 0.05。 表 2 实验组B组牙周-正畸治疗前、中、后咬合力数据($\bar x \pm s $)
Table 2. The data of occlusion force before,during and after periodontal orthodontic treatment in Group B ($\bar x \pm s $)
时间 咬合时间(s) 咬合力百分比(%) 前牙区(APAT) 后牙区(APMT) 治疗前 1.29 ± 0.39 11.54 ± 3.82 88.46 ± 3.82 治疗中 1.07 ± 0.35 16.83 ± 3.43 83.17 ± 3.33 治疗后 0.92 ± 0.37 20.79 ± 4.83 79.21 ± 4.83 t −8.239 0.979 −0.607 P 0.027* 0.034* 0.049* *P < 0.05。 表 3 对照组A组治疗前中后松动度对比
Table 3. Comparison of tooth mobility in Group A before,during and after treatment
参数 治疗前 治疗中 治疗后 Chi-Square 0.000a 10.900b 19.900b df 1 2 2 Asymp 1.000 0.004 0.000 a平均数相差不显著;b平均数相差显著。 表 4 牙周-正畸治疗前牙周临床指数与松动度相关性分析
Table 4. Correlation analysis of periodontal clinical index and tooth mobility before periodontal orthodontic treatment
牙周指数 牙周袋深度 附着丧失 出血指数 r P r P r P 松动度 −0.810 < 0.01* −0.800 < 0.01* −0.776 < 0.01* *P < 0.05。 表 5 牙周-正畸治疗后牙周临床指数与松动度相关性分析
Table 5. Correlation analysis of periodontal clinical index and tooth mobility after periodontal orthodontic treatment
牙周指数 牙周袋深度 附着丧失 出血指数 r P r P r P 松动度 −0.415 < 0.01* −0.420 < 0.01* −0.776 < 0.01* *P < 0.05。 -
[1] 中华口腔医学会. 维护牙周健康的中国口腔医学多学科专家共识(第一版)[J]. 中华口腔医学杂志,2021,56(2):127-135. doi: 10.3760/cma.j.cn112144-20210112-00013 [2] Caton J G,Armitage G,Berglundh T,et al. A new classification scheme for periodontal and peri-implant diseases and conditions - Introduction and key changes from the 1999 classification[J]. J Clin Periodontol,2018,45(Suppl 20):S1-S8. doi: 10.1111/jcpe.12935 [3] 第四次全国口腔健康流行病学调查结果发布. 中国政府网-中央人民政府门户网站[EB/OL]. [2017-09-20]. https://www.gov.cn/xinwen/2017-09/20/content_5226224.htm [4] 刘红蕊,葛少华. 我国牙周病学学科发展的历程回顾[J]. 中华口腔医学杂志,2023,58(12):1205-1216. doi: 10.3760/cma.j.cn112144-20231013-00192 [5] 刘体倩,梁星,刘蔚晴,等. 咬合创伤在牙周炎发生发展中的作用及机制的研究进展[J]. 国际口腔医学杂志,2023,50(1):19-24. doi: 10.7518/gjkq.2023020 [6] Fan J,Caton J G. Occlusal trauma and excessive occlusal forces: Narrative review,case definitions,and diagnostic considerations[J]. J Periodontol,2018,89(Suppl 1):S214-S222. doi: 10.1002/JPER.16-0581 [7] Lindhe J,Svanberg G. Influence of trauma from occlusion on progression of experimental periodontitis in the beagle dog[J]. J Clin Periodontol,1974,1(1):3-14. doi: 10.1111/j.1600-051X.1974.tb01234.x [8] Lindhe J,Ericsson I. The effect of elimination of jiggling forces on periodontally exposed teeth in the dog[J]. J Periodontol,1982,53(9):562-567. doi: 10.1902/jop.1982.53.9.562 [9] Kantor M,Polson A M,Zander H A. Alveolar bone regeneration after removal of inflammatory and traumatic factors[J]. J Periodontol,1976,47(12):687-695. doi: 10.1902/jop.1976.47.12.687 [10] 朱敏姬,滕英,潘慧琦,等. 正畸牙周联合治疗对牙周炎患者咬合创伤改善的研究[J]. 当代医学,2022,28(4):180-182. doi: 10.3969/j.issn.1009-4393.2022.04.068 [11] 姜倩,贾淑娟. 咬合调整治疗慢性牙周炎合并咬合创伤患者的临床效果[J]. 中国医学创新,2021,18(17):116-119. doi: 10.3969/j.issn.1674-4985.2021.17.029 [12] 黄墁珊,寻春雷. T-scan系统结合数字化模型测量咬合力分布的可靠性和准确性研究[J]. 中华口腔正畸学杂志,2020,27(2):90-95. doi: 10.3760/cma.j.cn115797-20191030-20206 [13] 杨瑟飞,施生根,张铭,等. 牙动度与牙周膜宽度关系的实验性研究[J]. 实用口腔医学杂志,2001,17(4):329-331. doi: 10.3969/j.issn.1001-3733.2001.04.019 [14] 吕悦,李玉玲. 牙齿松动度的研究现状[J]. 中华老年口腔医学杂志,2003,1(4):238-240. doi: 10.3969/j.issn.1672-2973.2003.04.017 [15] 李旭明. 80例牙周炎患者病情及相关因素分析研讨[J]. 健康必读,2021(22):28. -






 下载:
下载: