Questionnaire Survey on General Medicine and Pre-hospital First Aid Knowledge Among People in Ludian County,Yunnan Province
-
摘要:
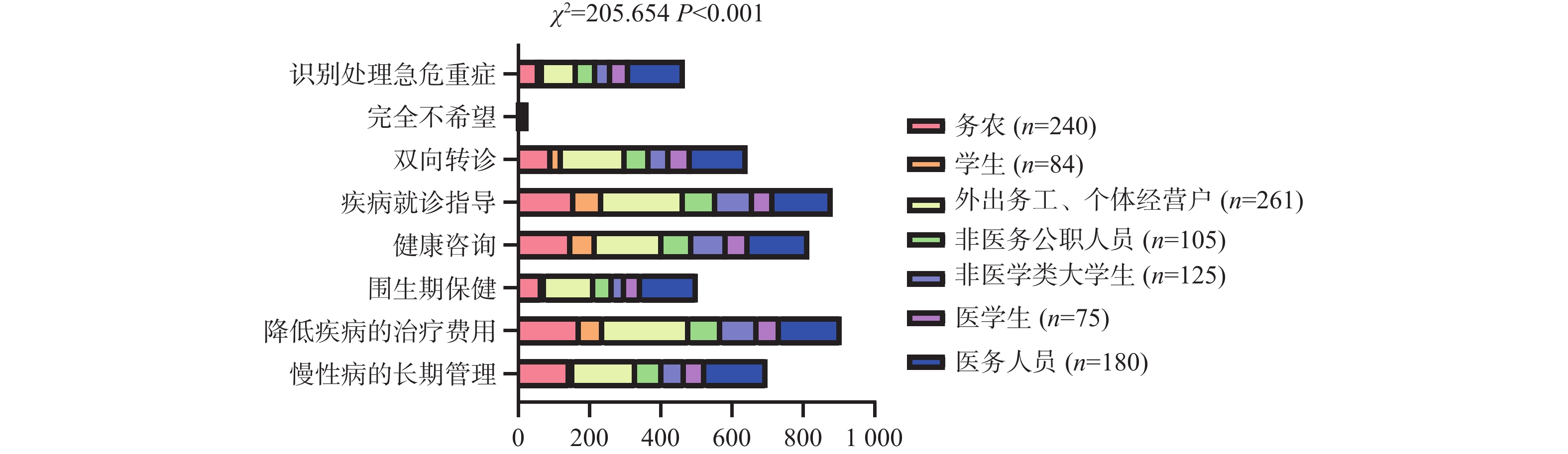
目的 探究云南省鲁甸县居民对全科医学、全科医生以及院前急救相关知识的认知情况以及态度,了解居民对于该类相关知识更易接受的培训学习方法,并对此提出针对性的解决方法。 方法 通过电子问卷、纸质问卷2种形式,对2022年10月15日至2022年12月30日期间菜市场门口核酸采集处以及2023年01月01日至2023年02月28日期间文屏街道卫生院门诊就诊人员,进行完全随机抽样调查。 结果 云南省鲁甸县城区接近50%的居民对全科医学、院前急救相关知识非常欠缺,尤其是对电除颤相关知识;高学历及医学类职业人群对全科医学的了解程度更高,并且对全科医学了解程度越高的人群更愿意参与到院前急救中,平均Ridit值:很熟悉全科医学(0.774) > 了解部分全科医学(0.565) > 完全没听过全科医学(0.400);学历越高、对全科医学了解程度越全面在参与院前急救方面呈正向影响,B值分别为0.624、0.619,OR值95% CI分别为1.867(1.544 ~ 2.257),1.857(1.298 ~ 2.657);以医务人员作为参照,医学生的B值 = 0.942,P = 0.234,差异不显著,非医学类职业人群B值均 < 0,呈负向影响。且大部分居民对院前急救的学习态度积极,有超过接近70%的居民愿意进行院前急救相关知识的学习及培训。 结论 云南省鲁甸县城区居民对全科医学的了解程度差,对全科医生的认可度不高,对全科医生的需求低,对院前急救的重要性认知欠缺。因不同人群认知存在差异,所以需要对不同人群进行分类别的针对性培训。 Abstract:Objective To explore the public's cognition and attitude towards general medicine, general practitioners, and pre-hospital first-aid knowledge in Ludian County, Yunnan Province, to find out the training and learning methods that are more acceptable to the public for this kind of related knowledge, and to propose targeted solutions. Methods A complete random sampling survey was conducted among the nucleic acid collection office at the gate of the vegetable market from October 15, 2022, to December 30, 2022, and the outpatient clinic of Wenping Street Health Center from January 1, 2023, to February 28, 2023, by using electronic questionnaire and paper questionnaire. Results Nearly 50% of the people in Ludian County of Yunnan Province lack the knowledge of general medicine and pre-hospital emergency care, especially the knowledge of electrical defibrillation. People with higher education and the medical profession have a higher understanding of general medicine, and people with a higher understanding of general medicine are more willing to participate in pre-hospital emergency care. The average Ridit value is: very familiar with general medicine (0.774) > Knowledge of some general practices (0.565) > Never heard of general practice (0.400). The higher education level and the more comprehensive understanding of general medicine had a positive impact on participation in pre-hospital emergency care, with B values of 0.624 and 0.619, OR 95% CI of 1.867 (1.544 ~ 2.257) and 1.857 (1.298 ~ 2.657), respectively. Taking medical staff as a reference, the B value of medical students was = 0.942, P = 0.234, the difference was not significant, and the B value of non-medical professional population was all less than 0, the effect is negative. In addition, most people have a positive attitude towards learning pre-hospital first aid, and more than 70% of people are willing to learn and train related knowledge of pre-hospital first aid. Conclusions People in urban areas of Ludian County, Yunnan Province have poor understanding of general practice, low recognition of general practitioners, low demand for general practitioners, and lack of awareness of the importance of pre-hospital emergency treatment. Because of the cognitive differences among different groups, it is necessary to conduct specific training for different groups. -
表 4 全科医学的了解程度对院前急救参与意愿情况分析
Table 4. Analysis and statistics of the understanding degree of general medicine and the willingness to participate in pre-hospital first aid
组别 平均Ridit值 95% CI χ 2 P 完全没听过 0.400 0.376 ~ 0.425 < 0.001 * 了解部分 0.565 0.538 ~ 0.591 158.747 很熟悉 0.774 0.711 ~ 0.837 *P < 0.05。 表 1 不同人群全科医学了解程度情况统计[n(%)]
Table 1. Statistics of general practice understanding of different populations [n(%)]
项目 完全没听过
(n = 525)了解部分
(n = 464)很熟悉
(n = 81)总计
(n =1070 )χ 2 P 工作性质 务农 184(35.05) 50(10.78) 6(7.41) 240(22.43) 377.195 < 0.001 * 学生 68(12.95) 16(3.45) 0(0.00) 84(7.85) 外出务工、个体经营户 159(30.29) 100(21.55) 2(2.47) 261(24.39) 非医务公职人员 27(5.14) 74(15.95) 4(4.94) 105(9.81) 非医学类大学生 65(12.38) 59(12.72) 1(1.23) 125(11.68) 医学生 20(3.81) 45(9.70) 10(12.35) 75(7.01) 医务人员 2(0.38) 120(25.86) 58(71.60) 180(16.82) 学历 文盲 56(10.67) 4(0.86) 0(0.00) 60(5.61) 127.15 < 0.001 * 小学 110(20.95) 37(7.97) 0(0.00) 147(13.74) 初中 120(22.86) 121(26.08) 16(19.75) 257(24.02) 中专、大专 30(5.71) 53(11.42) 5(6.17) 88(8.22) 高中 122(23.24) 98(21.12) 26(32.10) 246(22.99) 本科及以上 87(16.57) 151(32.54) 34(41.98) 272(25.42) 宗教信仰 无宗教信仰 288(54.86) 229(49.35) 44(54.32) 561(52.43) 3.446 0.328 佛教 46(8.76) 45(9.70) 3(3.70) 94(8.79) 伊斯兰教 169(32.19) 174(37.50) 31(38.27) 374(34.95) 其他宗教 22(4.19) 16(3.45) 3(3.70) 41(3.83) 民族 汉族 300(57.14) 241(51.94) 46(56.79) 587(54.86) 3.558 0.313 回族 169(32.19) 174(37.50) 31(38.27) 374(34.95) 白族 34(6.48) 33(7.11) 1(1.23) 68(6.36) 其他民族 22(4.19) 16(3.45) 3(3.70) 41(3.83) 年龄(岁) 18~25 168(32.00) 114(24.57) 19(23.46) 301(28.13) 35.097 < 0.001 * 26~40 197(37.52) 234(50.43) 42(51.85) 473(44.21) 41~60 114(21.71) 106(22.84) 18(22.22) 238(22.24) > 60 46(8.76) 10(2.16) 2(2.47) 58(5.42) 性别 男 253(48.19) 232(50.00) 39(48.15) 524(48.97) − 0.409 0.683 女 272(51.81) 232(50.00) 42(51.85) 546(51.03) *P < 0.05。 表 2 不同人群心肺复苏、电除颤认知情况统计[n(%)]
Table 2. Statistics of cognition of cardiopulmonary resuscitation and electrical defibrillation in different populations [n(%)]
类别 变量 完全不了解
(n = 299)听说过心肺复苏、
自动除颤仪,但不
知道规范操作
(n = 414)会操作心肺复苏,
但不会使用自动
除颤仪(n = 278)可以规范的进行
心肺复苏及使用
自动除颤仪
(n = 79)总计
(n =1070 )χ 2 P 性别 男 134(44.82) 204(49.28) 142(51.08) 44(55.70) 524(48.97) − 1.926 0.054 女 165(55.18) 210(50.72) 136(48.92) 35(44.30) 546(51.03) 年龄
(岁)18~25 72(24.08) 140(33.82) 59(21.22) 30(37.97) 301(28.13) 76.537 < 0.001* 26~40 99(33.11) 175(42.27) 156(56.12) 43(54.43) 473(44.21) 41~60 87(29.10) 84(20.29) 61(21.94) 6(7.59) 238(22.24) > 60 41(13.71) 15(3.62) 2(0.72) 0(0.00) 58(5.42) 民族 汉族 170(56.86) 226(54.59) 143(51.44) 48(60.76) 587(54.86) 7.513 0.057 回族 90(30.10) 150(36.23) 112(40.29) 22(27.85) 374(34.95) 白族 21(7.02) 22(5.31) 20(7.19) 5(6.33) 68(6.36) 其他
民族18(6.02) 16(3.86) 3(1.08) 4(5.06) 41(3.83) 宗教
信仰无宗教
信仰160(53.51) 221(53.38) 139(50.00) 41(51.90) 561(52.43) 7.704 0.053 佛教 31(10.37) 27(6.52) 24(8.63) 12(15.19) 94(8.79) 伊斯兰教 90(30.10) 150(36.23) 112(40.29) 22(27.85) 374(34.95) 其他宗教 18(6.02) 16(3.86) 3(1.08) 4(5.06) 41(3.83) 学历 文盲 52(17.39) 8(1.93) 0(0.00) 0(0.00) 60(5.61) 294.605 < 0.001* 小学 103(34.45) 35(8.45) 9(3.24) 0(0.00) 147(13.74) 初中 75(25.08) 99(23.91) 77(27.70) 6(7.59) 257(24.02) 中专
大专8(2.68) 32(7.73) 45(16.19) 3(3.80) 88(8.22) 高中 39(13.04) 136(32.85) 49(17.63) 22(27.85) 246(22.99) 本科及
以上22(7.36) 104(25.12) 98(35.25) 48(60.76) 272(25.42) 工作
性质务农 153(51.17) 71(17.15) 16(5.76) 0(0.00) 240(22.43) 483.356 < 0.001* 学生 20(6.69) 64(15.46) 0(0.00) 0(0.00) 84(7.85) 外出务工、
个体经营户91(30.43) 130(31.40) 40(14.39) 0(0.00) 261(24.39) 非医务公
职人员12(4.01) 56(13.53) 34(12.23) 3(3.80) 105(9.81) 非医学类
大学生13(4.35) 68(16.43) 40(14.39) 4(5.06) 125(11.68) 医学生 7(2.34) 9(2.17) 37(13.31) 22(27.85) 75(7.01) 医务人员 3(1.00) 16(3.86) 111(39.93) 50(63.29) 180(16.82) *P < 0.05, **P < 0.01。 表 3 旁人出现心跳、呼吸停止时愿意参与救援情况统计[n(%)]
Table 3. Statistics on the willingness of others to participate in rescue when heart or respiratory arrest occurs [n(%)]
项目 类别 不愿意(n = 542) 若是熟悉的人,愿意(n = 219) 愿意(n = 309) 总计(n = 1070 )χ 2 P 年龄
(岁)18~25 147(27.12) 60(27.40) 94(30.42) 301(28.13) 51.965 < 0.001* 26~40 206(38.01) 102(46.58) 165(53.40) 473(44.21) 41~60 138(25.46) 51(23.29) 49(15.86) 238(22.24) > 60 51(9.41) 6(2.74) 1(0.32) 58(5.42) 民族 汉族 304(56.09) 114(52.05) 169(54.69) 587(54.86) 3.821 0.281 回族 180(33.21) 82(37.44) 112(36.25) 374(34.95) 白族 32(5.90) 16(7.31) 20(6.47) 68(6.36) 其他民族 26(4.80) 7(3.20) 8(2.59) 41(3.83) 宗教
信仰无宗教信仰 292(53.87) 108(49.32) 161(52.10) 561(52.43) 4.052 0.256 佛教 44(8.12) 22(10.05) 28(9.06) 94(8.79) 伊斯兰教 180(33.21) 82(37.44) 112(36.25) 374(34.95) 其他宗教 26(4.80) 7(3.20) 8(2.59) 41(3.83) 学历 文盲 58(10.70) 0(0.00) 2(0.65) 60(5.61) 174.413 < 0.001* 小学 119(21.96) 15(6.85) 13(4.21) 147(13.74) 初中 129(23.80) 60(27.40) 68(22.01) 257(24.02) 中专、大专 31(5.72) 21(9.59) 36(11.65) 88(8.22) 高中 135(24.91) 47(21.46) 64(20.71) 246(22.99) 本科及以上 70(12.92) 76(34.70) 126(40.78) 272(25.42) 工作
性质务农 175(32.29) 16(7.31) 49(15.86) 240(22.43) 374.504 < 0.001* 学生 76(14.02) 7(3.20) 1(0.32) 84(7.85) 外出务工、
个体经营户181(33.39) 60(27.40) 20(6.47) 261(24.39) 非医务公职
人员41(7.56) 35(15.98) 29(9.39) 105(9.81) 非医学类
大学生52(9.59) 34(15.53) 39(12.62) 125(11.68) 医学生 2(0.37) 23(10.50) 50(16.18) 75(7.01) 医务人员 15(2.77) 44(20.09) 121(39.16) 180(16.82) 性别 男 244(45.02) 117(53.42) 163(52.75) 524(48.97) − 2.430 0.015* 女 298(54.98) 102(46.58) 146(47.25) 546(51.03) *P < 0.05。 表 5 变量名及赋值
Table 5. Variable name and assignment
变量 赋值 当旁人出现心跳、呼吸停止时是
否愿意行心肺复苏和电除颤0 = 不愿意,1 = 若是熟悉的人,愿意,2 = 愿意 工作性质 1 = 务农,2 = 学生,3 = 外出务工、个体经营户,4 = 非医务公职人员,
5 = 非医学类大学生,6 = 医学生,7 = 医务人员性别 1 = 男,2 = 女 年龄 1 = 18~25岁,2 = 26~40岁,3 = 41~60岁,4 = > 60岁 学历 1 = 文盲,2 = 小学,3 = 初中,4 = 中专、大专,5 = 高中,
6 = 本科及以上全科医学了解程度 1 = 完全没听过,2 = 了解部分,3 = 很熟悉 表 6 院前急救参与意愿影响因素的多分类Logistic回归分析
Table 6. Multivariate Logistic regression analysis of influencing factors of participation intention in pre-hospital emergency care
影响因素 若是熟悉的人,愿意 愿意 回归系数 P OR OR 95% CI 回归系数 P OR OR 95% CI 性别(对照 = 男性) 女 − 0.263 0.142 0.769 0.541~1.092
− 0.246 0.188 0.782 0.542~1.128
工作性质(对照 = 医务人员) 医学生 1.212 0.134 3.360 0.688~16.418 0.942 0.234 2.566 0.543~12.133 非医学类大学生 − 2.363 < 0.001* 0.094 0.039~0.228 − 3.408 < 0.001* 0.033 0.014~0.078 非医务公职人员 − 1.727 < 0.001* 0.178 0.079~0.403 − 2.904 < 0.001* 0.055 0.024~0.124 外出务工、个体经营户 − 1.906 < 0.001* 0.149 0.072~0.305 − 3.501 < 0.001* 0.030 0.014~0.065 学生 − 3.933 < 0.001* 0.020 0.007~0.059 − 6.869 < 0.001* 0.001 0.000~0.009 务农 − 2.693 < 0.001* 0.068 0.028~0.163 − 1.814 < 0.001* 0.163 0.078~0.342 年龄 − 0.126 0.346 0.882 0.679~1.146 − 0.463 0.001* 0.629 0.483~0.819 学历 0.410 < 0.001* 1.507 1.251~1.817 0.624 < 0.001* 1.867 1.544~2.257 全科医学了解程度 0.115 0.524 1.122 0.787~1.599 0.619 0.001* 1.857 1.298~2.657 截距 − 0.363 0.607 0.696 0.175~2.767
− 0.744 0.280 0.475 0.123~1.833 *P< 0.05。 表 7 居民院前急救知识培训、学习方式情况分析[n(%)]
Table 7. Analysis of pre-hospital first-aid knowledge training and learning style of residents [n(%)]
项目 线上视频讲授 医院及社区组织
的规范培训宣传操作手册 课堂,讲座 其他 χ 2 P 工作性质 务农 17(5.57) 38(8.03) 8(3.38) 17(5.12) 4(40.00) 139.884 < 0.001 * 学生 6(1.97) 10(2.11) 15(6.33) 20(6.02) 0(0.00) 外出务工、个体
经营户30(9.84) 88(18.60) 87(36.71) 60(18.07) 1(10.00) 非医务公职人员 34(11.15) 55(11.63) 34(14.35) 28(8.43) 2(20.00) 非医学类大学生 77(25.25) 78(16.49) 43(18.14) 62(18.67) 1(10.00) 医学生 43(14.10) 56(11.84) 5(2.11) 43(12.95) 2(20.00) 医务人员 98(32.13) 148(31.29) 45(18.99) 102(30.72) 0(0.00) 年龄(岁) 18~25 103(33.77) 124(26.22) 62(26.16) 115(34.64) 7(70.00) 25.536 0.012* 26~40 162(53.11) 259(54.76) 122(51.48) 163(49.10) 3(30.00) 41~60 40(13.11) 89(18.82) 52(21.94) 54(16.27) 0(0.00) > 60 0(0.00) 1(0.21) 1(0.42) 0(0.00) 0(0.00) *P < 0.05。 -
[1] Dingwall S,Henderson J,Britt H,et al. Adequacy of Australia's GP workforce: estimating supply and demand,2005-06 to 2015-16[J]. Australian Health Review,2020,44(2):328-333. doi: 10.1071/AH18252 [2] Wang Y,Zhou C C. Promoting social engagement of the elderly to cope with aging of the Chinese population[J]. Biosci Trends,2020,14(4):310-313. doi: 10.5582/bst.2020.03305 [3] Fu Y,Wang J,Sun J,et al. Equity in the allocation of general practitioner resources in China's mainland from 2012 to 2019[J]. Healthcare (Basel),2023,11(3):398. doi: 10.3390/healthcare11030398Fu Y,Wang J,Sun J,et al. Equity in the allocation of general practitioner resources in China's mainland from 2012 to 2019[J]. Healthcare (Basel),2023,11(3):398. doi: 10.3390/healthcare11030398 [4] Meng Q,Mills A,Wang L,et al. What can we learn from China's health system reform?[J]. BMJ,2019,365:12349. [5] Wnent J,Tjelmeland I,Lefering R,et al. To ventilate or not to ventilate during bystander CPR - A EuReCa TWO analysis[J]. Resuscitation,2021,166:101-109. doi: 10.1016/j.resuscitation.2021.06.006 [6] Xie X,Zheng J,Zheng W,et al. Efforts to improve survival outcomes of out-of-hospital cardiac arrest in China: Basic-OHCA[J]. Circulation. Cardiovascular Quality and Outcomes,2022,16(2):e008856. [7] Struwe L A,Rhone K B,Haas D,et al. Comparison of recertification methods on CPR quality[J]. Jouanal of Continuing Education Nursing,2022,53(1):43-48. doi: 10.3928/00220124-20211210-10 [8] Zhou G Z,Wang Y,Sun Z H,et al. Survival outcome among patients with out-of-hospital cardiac arrest who received cardiopulmonary resuscitation in China: A systematic review and meta-analysis[J]. European Journal Medical Research,2023,28(1):8. doi: 10.1186/s40001-022-00955-x [9] Wang J G,He Y B,Chen X L,et al. A retrospective study on epidemiological analysis of pre-hospital emergency care in Hangzhou,China[J]. PLoS One,2023,18(4):e0282870. doi: 10.1371/journal.pone.0282870 [10] Kim S H,Park J H,Jeong J,et al. Bystander cardiopulmonary resuscitation,automated external defibrillator use,and survival after out-of-hospital cardiac arrest[J]. American Journal of Emergency Medicine,2023,66:85-90. doi: 10.1016/j.ajem.2023.01.033 [11] Obling L,Hassager C,Blomberg S N,et al. Inverse association between bystander use of audiovisual feedback from an automated external defibrillator and return of spontaneous circulation[J]. Journal of the American Heart Association,2022,11(4):e023232. doi: 10.1161/JAHA.121.023232 [12] Sohn Y,Cho G C,Cho Y. The interaction effect of bystander cardiopulmonary resuscitation (CPR) and dispatcher CPR on outcomes after out-of-hospital cardiac arrest[J]. Sci Rep,2022,12(1):22450. doi: 10.1038/s41598-022-27096-9 [13] Pei-Chuan Huang E,Chiang W C,Lu T C,et al. Barriers to bystanders defibrillation: A national survey on public awareness and willingness of bystanders defibrillation☆[J]. Journal of the Formosan Medical Association,2020,120(3):974-982. [14] Farquharson B,Dixon D,Williams B,et al. The psychological and behavioural factors associated with laypeople initiating CPR for out-of-hospital cardiac arrest: A systematic review[J]. BMC Cardiovascular Disorders,2023,23(1):19. doi: 10.1186/s12872-022-02904-2 [15] 陈习琼. 云南省人口年龄构成、老龄化空间分异及优化对策[J]. 中国老年学杂志,2018,38(6):1513-1518. doi: 10.3969/j.issn.1005-9202.2018.06.096 [16] Alharbi B A,Masud N,Alajlan F A,et al. Association of elderly age and chronic illnesses: Role of gender as a risk factor[J]. Journal of Family Medicine and Primary Care,2020,9(3):1684-1690. doi: 10.4103/jfmpc.jfmpc_1060_19 [17] Zhai X,Zhang Q,Li X,et al. Association between multimorbidity patterns and catastrophic health expenditure among Chinese older adults living alone[J]. Archives Gerontology and Geriatrics,2023,106:104892. doi: 10.1016/j.archger.2022.104892 [18] Li H,Liu K,Gu J,et al. The development and impact of primary health care in China from 1949 to 2015: A focused review[J]. International Journal Health Planning And Management,2017,32(3):339-350. [19] Tzeng C F, Lu C H, Lin C H. Community socioeconomic status and dispatcher-assisted cardiopulmonary resuscitation for patients with out-of-hospital cardiac arrest[J]. Int J Environ Res Public Health, 2021, 18 (3): 1207. [20] Smith A,Masters S,Ball S,et al. The incidence and outcomes of out-of-hospital cardiac arrest in metropolitan versus rural locations: A systematic review and meta-analysis[J]. Resuscitation,2023,185:109655. doi: 10.1016/j.resuscitation.2022.11.021 [21] 庞爱华,张西英,艾莉,等. 院外心肺复苏"第一目击者"自我效能感及影响因素分析[J]. 中国急救复苏与灾害医学杂志,2022,17(12):1544-1547. doi: 10.3969/j.issn.1673-6966.2022.12.002 [22] 李星星,杨德兴,尹应美,等. 昆明医科大学本科学生院前急救知识掌握情况的问卷调查及对策[J]. 昆明医科大学学报,2016,37(8):44-46. doi: 10.3969/j.issn.1003-4706.2016.08.010 [23] Folke F,Shahriari P,Hansen C M,Gregers,M C T. Public access defibrillation: Challenges and new solutions[J]. Current Opinion in Critical Care,2023,29(3):168-174. doi: 10.1097/MCC.0000000000001051 [24] Delhomme C,Njeim M,Varlet E,et al. Automated external defibrillator use in out-of-hospital cardiac arrest: Current limitations and solutions[J]. Archives of Cardiovascular Diseases,2019,112(3):217-222. doi: 10.1016/j.acvd.2018.11.001 -






 下载:
下载: