Application of Endoscope and Microscope in Tympanoplasty for Middle-aged and Young Patients with CSOM
-
摘要:
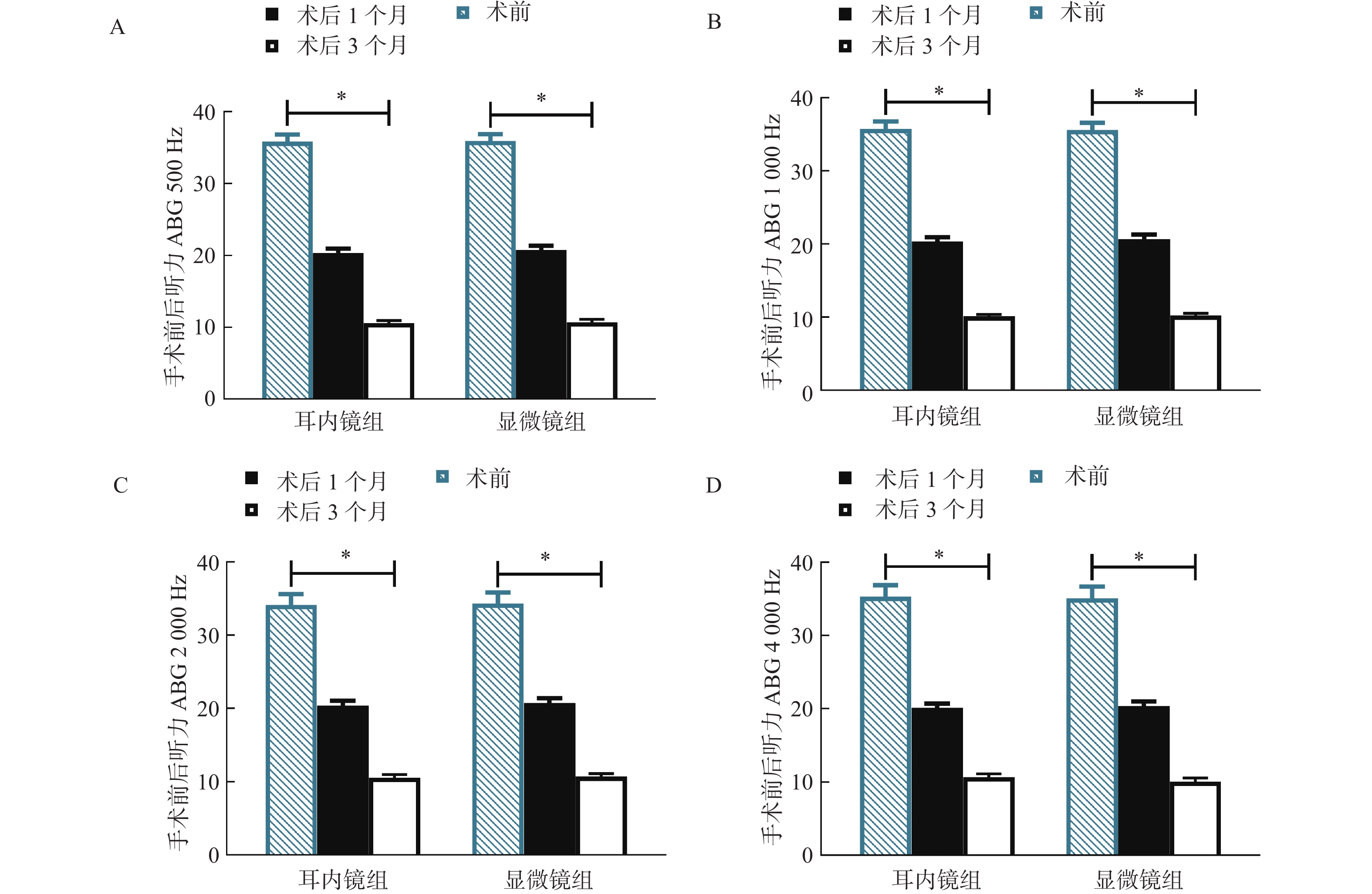
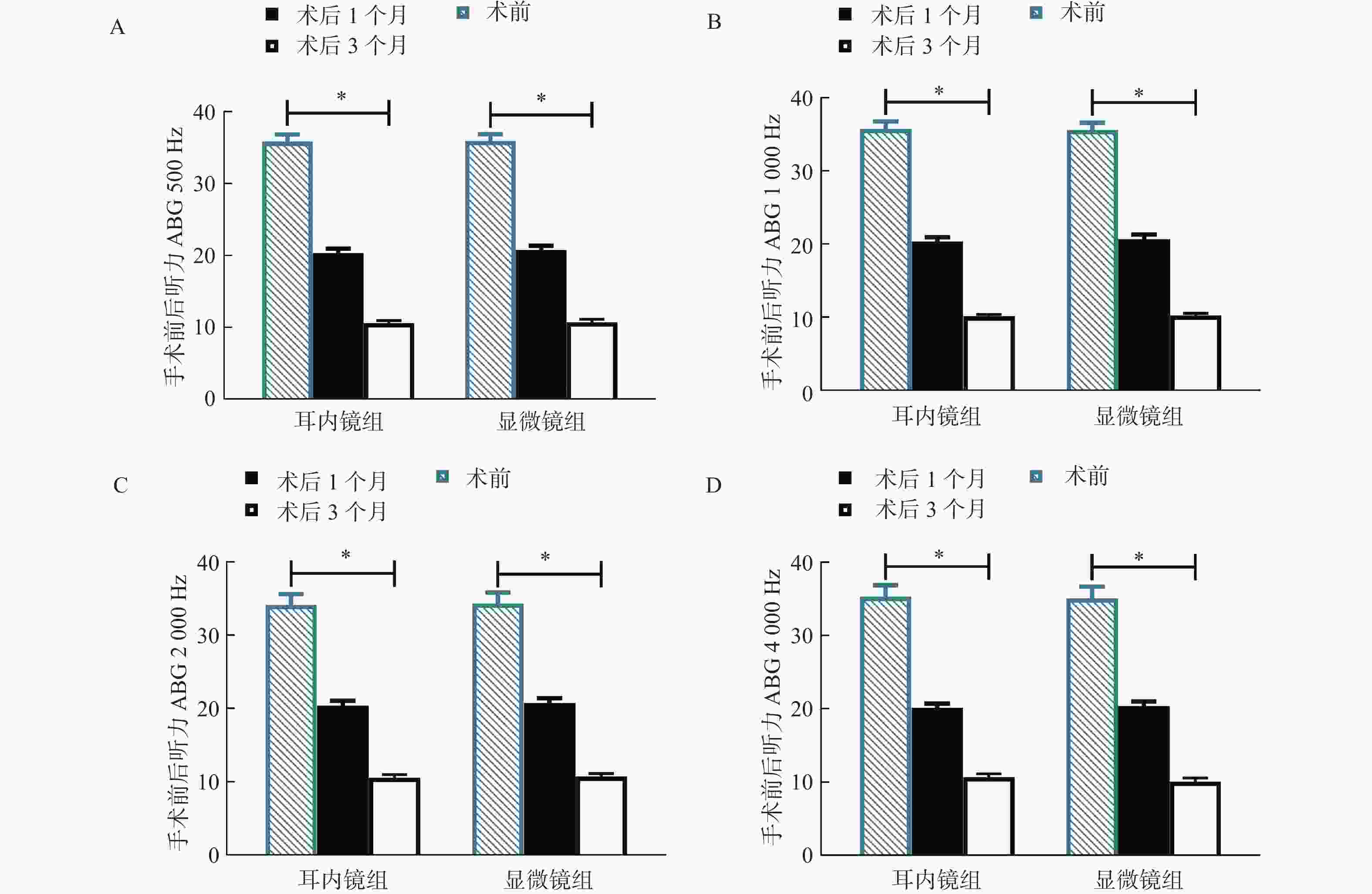
目的 探究耳内镜与显微镜下鼓室成形术在中青年慢性化脓性中耳炎(chronic suppurative otitis media,CSOM)中的应用。 方法 选取2020年4月至2022年6月西藏自治区人民政府驻成都办事处医院收治的104例中青年CSOM患者,随机分为耳内镜组(n = 52)、显微镜组(n = 52)。比较2组手术前后听力情况、血管通透性相关因子[血小板活化因子(platelet activatingfactor,PAF)、纤维连接蛋白(fibronectin,Fn)]、疼痛程度(visual analogue scales,VAS评分)、睡眠质量(pittsburgh sleep quality index,PSQI评分)、炎症状态[转化生长因子-β1(transforming growth factor-β1,TGF-β1)、转化生长因子-β2(transforming growth factor-β2,TGF-β2)、白介素-8(interleukin-8,IL-8)、可溶性白细胞介素-2受体(soluble interleukin 2 receptor,sIL-2R)]及并发症。 结果 术后1个月、3个月,2组各频率气骨导差(air bone gap,ABG)比较,差异无统计学意义(P > 0.05);耳内镜组术后1个月、3个月VAS、PSQI评分均低于显微镜组( P < 0.05);耳内镜组术后1个月、3个月PAF水平低于显微镜组,Fn水平高于显微镜组( P < 0.05);术后1个月、3个月,耳内镜组血清TGF-β1、TGF-β2、IL-8、sIL-2R均低于显微镜组( P < 0.05);耳内镜组并发症发生率与显微镜组比较,差异无统计学意义( P > 0.05)。 结论 2种手术方式是中青年CSOM患者安全可靠的治疗方案,与显微镜手术相比,耳内镜下鼓室成形术后恢复时间更短,利于疼痛缓解,改善生活质量,并改善血管通透性,减轻机体炎症反应。 -
关键词:
- 化脓性中耳炎 /
- 耳内镜;显微镜;鼓室成形术 /
- 疼痛程度 /
- 炎症状态 /
- 并发症
Abstract:Objective To explore the application of otoscopic and microscopic tympanoplasty in the treatment of chronic suppurative otitis media (CSOM) in young and middle-aged patients, and provide a reference for clinical treatment. Methods A total of 104 young and middle-aged patients with CSOM admitted to Chengdu Office Hospital of the People’ s Government of the Xizang Autonomous Region from April 2020 to June 2022 were randomly divided into an Ear endoscopy group (52 cases) and a Microscope group (52 cases). The two groups were compared in terms of pre- and post-operative hearing conditions, vascular permeability-related factors [platelet activating factor (PAF), fibronectin (Fn)], pain intensity (visual analogue scales, VAS score), sleep quality (Pittsburgh Sleep Quality Index, PSQI score), inflammatory status [transforming growth factor-β1 (TGF-β1), transforming growth factor-β2 (TGF-β2), interleukin-8 (IL-8), soluble interleukin 2 receptor (sIL-2R)], and complications. Results There was no significant difference in air bone gap (ABG) at each frequency between the two groups at 1 month and 3 months after surgery. (P > 0.05). The VAS and PSQI scores in the Ear endoscopy group were lower than those in the Microscope group 1 month and 3 months after surgery ( P < 0.05) . The PAF level in the Ear endoscopy group was lower and the Fn level was higher than that in the Microscope group 1 month and 3 months after surgery ( P < 0.05); serum TGF-β1, TGF-β2, IL-8, and sIL-2R levels were lower in the Ear endoscopy group than in the Microscope group 1 month and 3 months after surgery ( P < 0.05). There was no significant difference in the incidence of complications between the Ear endoscopy group and the Microscope group ( P > 0.05). Conclusion Both surgical methods are safe and reliable treatment options for young and middle-aged patients with CSOM. Compared with microscopic surgery, otic endoscopic tympanoplasty has a shorter recovery time, facilitates pain relief, improves quality of life, and improves vascular permeability, reducing the body's inflammatory response. -
表 1 基线资料[n(%)/( $ \bar x \pm s $)]
Table 1. Baseline data[n(%)/( $ \bar x \pm s$)]
基线资料 耳内镜组(n=52) 显微镜组(n=52) χ2/t/u P 年龄(岁) 29.55±5.43 30.22±5.07 0.650 0.517 性别 0.346 0.556 男 28(53.85) 25(48.08) 女 24(46.15) 27(51.92) 病程(a) 2.98±0.84 3.21±0.62 1.589 0.115 患耳 0.347 0.556 右耳 29(55.77) 26(50.00) 左耳 23(44.23) 26(50.00) 纯音测听/气骨导差(ABG) 0.215 0.975 46~60 dB 3(5.77) 2(3.85) 36~45 dB 17(32.67) 17(32.69) 26~35 dB 32(61.54) 33(63.46) 表 2 2组手术前后听力ABG比较( $ \bar x \pm s $,dB)
Table 2. Comparison of hearing ABG before and after operation between the two groups ( $ \bar x \pm s $,dB)
频率 组别 n 术前 术后1个月 术后3个月 F P 500 Hz 耳内镜组 52 35.80±3.61 20.34±2.15a 10.59±1.35a 1294.344 <0.001* 显微镜组 52 35.91±3.47 20.79±2.06a 10.71±1.43a 1369.209 <0.001* t 0.158 1.090 0.440 P 0.874 0.278 0.661 1000 Hz耳内镜组 52 35.76±3.58 20.34±2.12a 10.12±0.89a 1435.709 <0.001* 显微镜组 52 35.59±3.61 20.68±2.25a 10.26±0.92a 1334.926 <0.001* t 0.241 0.793 0.789 P 0.810 0.430 0.432 2000 Hz耳内镜组 52 34.16±5.28 20.39±2.34a 10.58±1.49a 615.293 <0.001* 显微镜组 52 34.33±5.31 20.71±2.57a 10.70±1.53a 590.872 <0.001* t 0.164 0.664 0.405 P 0.870 0.508 0.686 4000 Hz耳内镜组 52 35.28±5.72 20.12±2.19a 10.64±1.73a 594.891 <0.001* 显微镜组 52 35.10±5.64 20.38±2.25a 10.02±1.95a 609.185 <0.001* t 0.162 0.597 1.051 P 0.872 0.552 0.296 与同组术前比较,aP < 0.05; *P < 0.05。 表 3 2组手术前后血管通透性相关因子比较[( $ \bar x \pm s $),ng/mL]
Table 3. Comparison of vascular permeability-related factors between the two groups before and after surgery [( $ \bar x \pm s $),ng/mL]
因子 组别 n 术前 术后1个月 术后3个月 F P PAF(ng/mL) 耳内镜组 52 123.20±20.77 97.89±11.54a 92.62±10.41ab 61.954 <0.001* 显微镜组 52 121.43±20.91 108.85±12.52a 98.02±11.03ab 29.921 <0.001* t 0.433 4.642 2.568 P 0.666 <0.001* 0.012* Fn(mg/L) 耳内镜组 52 120.73±13.47 154.63±15.17a 181.92±22.84ab 157.080 <0.001* 显微镜组 52 123.42±15.10 140.70±16.21a 156.36±20.04ab 47.459 <0.001* t 0.959 4.525 6.066 P 0.340 <0.001* <0.001* 与同组术前比较,aP < 0.05;与同组术后1个月比较, bP < 0.05; *P < 0.05。 表 4 2组手术前后VAS评分、PSQI评分比较( $ \bar x \pm s $,分)
Table 4. Comparison of VAS score and PSQI score before and after operation between the two groups ( $ \bar x \pm s$,points)
评分 组别 n 术前 术后1个月 术后3个月 F P VAS评分 耳内镜组 52 5.52±1.22 2.61±0.50a 1.35±0.48ab 362.434 <0.001* 显微镜组 52 5.47±1.35 3.58±0.63a 2.84±0.52ab 115.251 <0.001* t 0.198 8.697 15.183 P 0.843 <0.001* <0.001* PSQI评分 耳内镜组 52 17.39±1.14 9.67±0.80a 6.08±0.75ab 2082.438 <0.001* 显微镜组 52 17.12±1.10 12.73±1.05a 10.36±0.79ab 624.958 <0.001* t 1.229 16.716 28.333 P 0.222 <0.001* <0.001* 与同组术前比较,aP < 0.05;与同组术后1个月比较, bP < 0.05; *P < 0.05。 表 5 2组手术前后炎症状态比较( $ \bar x \pm s $)
Table 5. Comparison of inflammation status before and after surgery between the two groups ( $ \bar x \pm s $)
指标 组别 n 术前 术后1个月 术后3个月 F P TGF-β1(μg/L) 耳内镜组 52 95.80±22.13 53.72±10.52a 43.61±8.48ab 177.766 <0.001* 显微镜组 52 93.75±26.43 68.65±12.47a 55.42±10.63ab 61.145 <0.001* t 0.429 6.599 6.263 P 0.669 <0.001* <0.001* TGF-β2(μg/L) 耳内镜组 52 15.70±3.88 9.65±1.92a 4.82±1.26ab 228.053 <0.001* 显微镜组 52 15.46±4.01 12.63±2.81a 8.56±2.10ab 66.116 <0.001* t 0.310 6.314 11.013 P 0.757 <0.001* <0.001* IL-8(ng/L) 耳内镜组 52 15.39±4.21 11.34±1.78a 6.35±1.27ab 142.127 <0.001* 显微镜组 52 15.74±4.02 12.25±2.45a 10.04±2.38ab 46.300 <0.001* t 0.434 2.167 9.864 P 0.666 0.033* <0.001* sIL-2R(U/mL) 耳内镜组 52 614.75±22.38 422.19±15.08a 382.47±14.69ab 2550.547 <0.001* 显微镜组 52 619.72±22.36 487.83±17.34a 419.68±15.82ab 1535.268 <0.001* t 1.133 20.598 12.429 P 0.260 <0.001* <0.001* 与同组术前比较,aP < 0.05;与同组术后1个月比较, bP < 0.05; *P < 0.05。 -
[1] Filipe M,Karppinen M,Kuatoko P,et al. Suppurative otitis media in Angola: Clinical and demographic features[J]. Trop Med Int Health,2020,25(10):1283-1290. doi: 10.1111/tmi.13466 [2] Tajdini A,Hatami N,Rahmaty B,et al. Comparing audiometric parameters between crushed and intact cartilage tympanoplasty: A double-blinded,randomised,controlled trial study[J]. J Laryngol Otol,2020,134(12):1060-1064. doi: 10.1017/S0022215120002327 [3] Si Y,Chen Y,Xu G,et al. Cartilage tympanoplasty combined with eustachian tube balloon dilatation in the treatment of adhesive otitis media[J]. Laryngoscope,2019,129(6):1462-1467. doi: 10.1002/lary.27603 [4] 谷长宏,王升举. 完壁式乳突根治并鼓室成形术治疗慢性化脓性中耳炎的临床有效性分析[J]. 临床和实验医学杂志,2021,20(1):104-107. [5] Zakir I,Ahmad A N,Pasha H A,et al. Comparison of endoscopic versus microscopic tympanoplasty[J]. Iran J Otorhinolaryngol,2022,34(122):139-143. [6] 中华医学会耳鼻咽喉头颈外科学分会耳科学组,中华耳鼻咽喉头颈外科杂志编辑委员会耳科组. 中耳炎临床分类和手术分型指南(2012)[J]. 中华耳鼻咽喉头颈外科杂志,2013,48(1):5. [7] Hwang W Y,Kim K,Cho H Y,et al. The voiding VAS score is a simple and useful method for predicting POUR after laparoscopy for benign gynaecologic diseases: A pilot study[J]. J Obstet Gynaecol,2022,42(6):2469-2473. doi: 10.1080/01443615.2022.2071149 [8] Liu D,Kahathuduwa C,Vazsonyi A T. The Pittsburgh Sleep Quality Index (PSQI): Psychometric and clinical risk score applications among college students[J]. Psychol Assess,2021,33(9):816-826. doi: 10.1037/pas0001027 [9] Stefan I,Stefanescu C D,Vlad A M,et al. Postoperative outcomes of endoscopic versus microscopic myringoplasty in patients with chronic otitis media-A systematic review[J]. Medicina (Kaunas),2023,59(6):1074. doi: 10.3390/medicina59061074 [10] Mishra A K,Mallick A,Galagali J R,et al. Mastoid cavity obliteration using bone pâté versus bioactive glass granules in the management of chronic otitis media (squamous disease): A prospective comparative study[J]. J Laryngol Otol,2021,135(6):492-500. doi: 10.1017/S0022215121001195 [11] Lubianca Neto J F, Koerig Schuster A, Neves Lubianca J P, et al. Comparison of inlay cartilage butterfly and underlay temporal fascia tympanoplasty[J]. OTO Open, 2022, 6(3): 2473974X221108935. [12] Erden B,Gülşen S. Evaluation of surgical and audiological outcomes of push-through myringoplasty and underlay cartilage tympanoplasty in repairing anterior tympanic membrane perforations[J]. J Craniofac Surg,2020,31(6):1709-1712. doi: 10.1097/SCS.0000000000006459 [13] 王忠勋,刘勇,李超,等. 湿耳条件下耳内镜鼓膜修补术对慢性化脓性中耳炎患者听力及咽鼓管功能的影响[J]. 山西医药杂志,2021,50(23):3235-3238. [14] 谭聪明,刘文军,刑园,等. 微创及传统开放式鼓室成形术治疗慢性化脓性中耳炎的临床观察[J]. 贵州医药,2022,46(10):1586-1587. [15] Tuoheti A,Gu X,Cheng X,et al. Silencing Nrf2 attenuates chronic suppurative otitis media by inhibiting pro-inflammatory cytokine secretion through up-regulating TLR4[J]. Innate Immun,2021,27(1):70-80. doi: 10.1177/1753425920933661 [16] Serban R,Filip C,Radulescu L M,et al. IL-1α,IL-6 and IL-8 serum values in patients with chronic suppurative otitis media[J]. Exp Ther Med,2021,22(5):1226. doi: 10.3892/etm.2021.10660 [17] 郜元坤,孙建芳. 左氧氟沙星联合地塞米松滴耳治疗化脓性中耳炎临床观察[J]. 中国药业,2020,29(4):79-81. [18] 曾涛. 盐酸左氧氟沙星滴耳液联合曲安奈德对急性化脓性中耳炎患者血清炎症因子和听力阈值的影响[J]. 中南医学科学杂志,2021,49(1):90-94. [19] 张帅刚,贺松坡,王海涛,等. 微创及传统开放式鼓室成形术治疗慢性化脓性中耳炎的比较[J]. 广东医学,2021,42(7):819-823. [20] Bozgul S M K,Ak G,Soyer N A,et al. Biomarker diversity in increased inflammation: Secondary hemophagocytic syndrome vs systemic inflammatory response syndrome[J]. Int J Lab Hematol,2023,45(2):213-220. -





 下载:
下载: