慢性阻塞性肺疾病急性加重期患者并发呼吸道合胞病毒感染的影响因素及与血清HSP70、KLF5、MIP-2水平的相关性
doi: 10.12259/j.issn.2095-610X.S20251114
Factors Influencing Respiratory Syncytial Virus Infection in Patients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease and Correlation with Serum Levels of HSP70,KLF5,MIP-2
-
摘要:
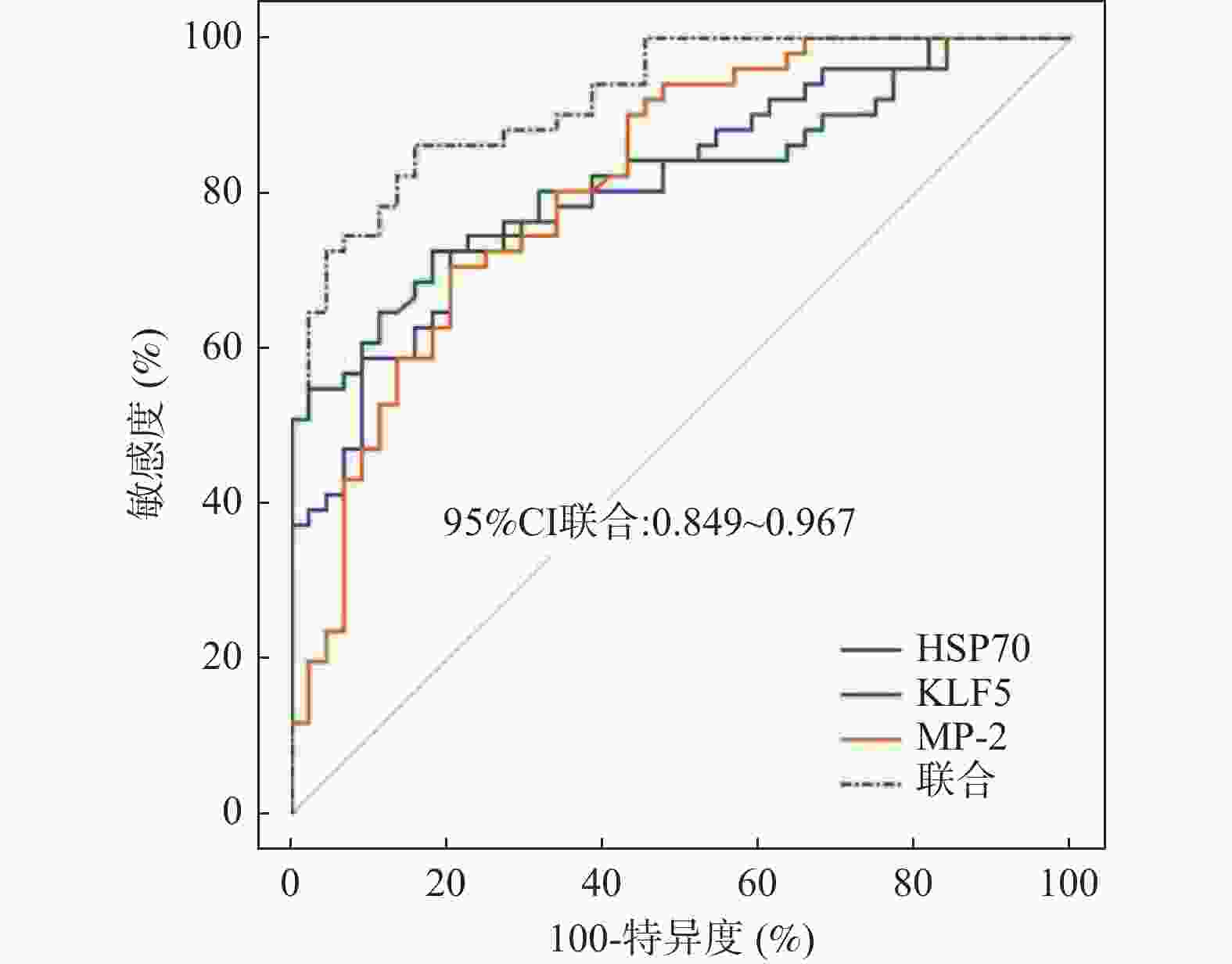
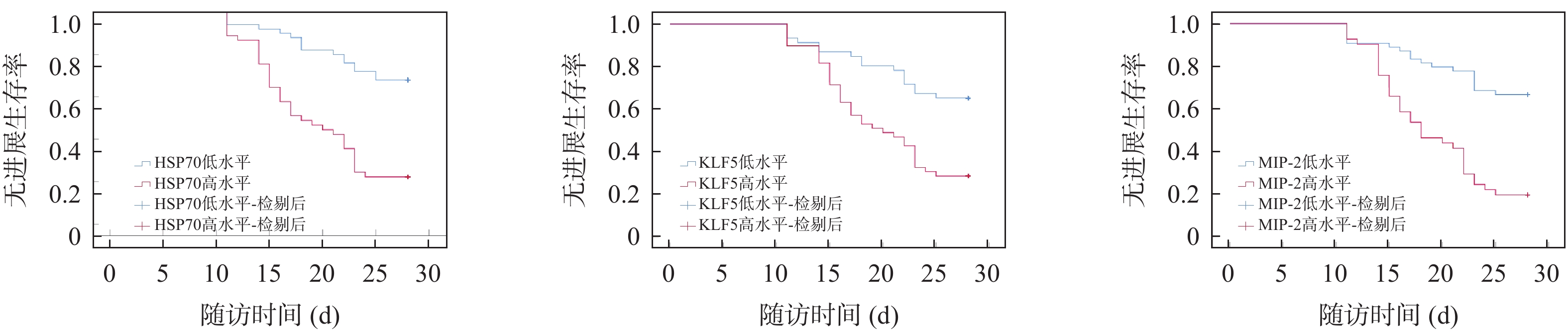
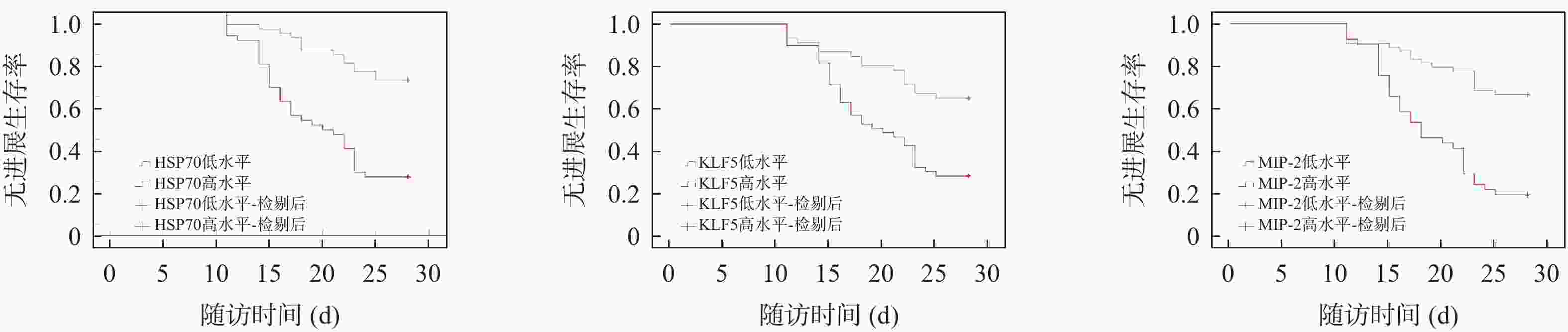
目的 探讨慢性阻塞性肺疾病急性加重期(AECOPD)患者并发呼吸道合胞病毒(RSV)感染的影响因素及与血清热休克蛋白70(HSP70)、Krüppel样因子5(KLF5)、巨噬细胞炎症蛋白-2(MIP-2)水平的相关性。 方法 前瞻性纳入195例AECOPD患者,根据RSV感染状态分为感染组(n = 95)与未感染组(n = 100),根据感染组患者病情严重程度分为轻、中、重度组(31例、35例、29例),根据预后情况分为预后不良组(n = 51)和预后良好组(n = 44)。ELISA法检测各组血清HSP70、KLF5、MIP-2水平,并分析其与相关临床指标的相关性;多因素Cox回归分析AECOPD患者并发RSV感染的风险因素;相对危险度分析高、低水平HSP70、KLF5、MIP-2对AECOPD合并RSV感染患者预后的影响;Kaplan-Meier生存曲线分析患者生存情况;绘制受试者工作特征曲线(ROC)分析血清HSP70、KLF5、MIP-2水平对AECOPD合并RSV感染患者预后预测价值。 结果 感染组呼吸衰竭人数占比及1年内加重次数、CRP、HSP70、KLF5、MIP-2水平显著高于未感染组(P < 0.05),而FEV1% pred显著低于未感染组(P < 0.05)。血清HSP70、KLF5、MIP-2分别与呼吸衰竭、1年内加重次数及CRP水平均呈正相关(P < 0.05),与FEV1% pred呈负相关(P < 0.05)。呼吸衰竭、1年内加重次数≥3次及低FEV1% pred和高CRP、HSP70、KLF5、MIP-2水平是AECOPD患者并发RSV感染的危险因素(P < 0.05)。随着病情加重,血清HSP70、KLF5、MIP-2水平逐渐升高(P < 0.05)。相较于预后良好组,预后不良组血清水平显著升高(P < 0.05)。高水平HSP70、KLF5、MIP-2患者的预后不良风险更大,28 d无进展生存率更低(P < 0.05)。三者联合预测的曲线下面积(AUC)显著优于单项指标预测(P = 0.015)。 结论 血清HSP70、KLF5、MIP-2水平与AECOPD合并RSV感染患者病情严重程度及预后密切相关,联合检测有助于临床早期评估病情、制定干预策略。 -
关键词:
- 慢性阻塞性肺疾病急性加重期 /
- 呼吸道合胞病毒 /
- 热休克蛋白70 /
- Krüppel样因子5 /
- 巨噬细胞炎症蛋白-2
Abstract:Objective To explore the factors associated with respiratory syncytial virus (RSV) infection in patients with acute exacerbation of chronic obstructive pulmonary disease (AECOPD) and its correlation with serum levels of heat shock protein 70 (HSP70), Krüppel-like factor 5 (KLF5), and macrophage inflammatory protein-2 (MIP-2). Methods A total of 195 AECOPD patients were prospectively enrolled and categorized into an RSV-infected group (n = 95) and an uninfected group (n = 100) based on RSV infection status. The infected group was further subdivided by disease severity into mild, moderate, and severe subgroups (31 cases, 35 cases, 29 cases), and by prognosis into poor prognosis (n = 51) and good prognosis subgroups (n = 44) . ELISA method was used to measure the serum levels of HSP70, KLF5, and MIP-2 in each group, and their correlation with relevant clinical indicators was analyzed. Multivariate Cox regression analysis was used to explore risk factors for RSV infection in AECOPD patients. Relative risk analysis was used to explore the impact of high and low levels of HSP70, KLF5, and MIP-2 on the prognosis of AECOPD patients with RSV infection. Kaplan-Meier survival curves analyzed patient survival outcomes. Receiver operating characteristic (ROC) curves were plotted to analyze the predictive value of serum HSP70, KLF5, and MIP-2 levels for the prognosis of AECOPD patients with RSV infection. Results The infected group had significantly higher proportions of respiratory failure, higher number of exacerbations within one year, and higher levels of CRP, HSP70, KLF5, and MIP-2 compared to the non-infected group (P < 0.05), while FEV1% pred were significantly lower (P < 0.05). Serum HSP70, KLF5, MIP-2 levels were positively correlated with respiratory failure, number of exacerbations within one year, and CRP levels (P < 0.05), and negatively correlated with FEV1% pred (P < 0.05). Multivariate Cox regression identified respiratory failure, number of AECOPD exacerbations within one year ≥ 3 times, low FEV1% pred, and high levels of CRP, HSP70, KLF5, and MIP-2 as independent risk factors for RSV infection in AECOPD patients (P < 0.05). As the condition worsens, the levels of serum HSP70, KLF5, and MIP-2 gradually increase (P < 0.05). The poor prognosis subgroup had prominently higher serum levels than the good prognosis subgroup(P < 0.05). Patients with high levels of HSP70, KLF5, and MIP-2 have a greater risk of poor prognosis and a lower 28-day progression-free survival rate (P < 0.05). The areas under the ROC curve (AUC) predicted by the combination of the three indicators was significantly better than that predicted by a single indicator (P = 0.015). Conclusion Respiratory failure, the number of AECOPD exacerbations within one year ≥ 3 times, low FEV1% pred, high CRP level, and high serum levels of HSP70, KLF5, and MIP-2 are risk factors for RSV infection in AECOPD patients. Serum levels of HSP70, KLF5, MIP-2 are closely related to disease severity and prognosis in AECOPD patients with RSV infection. The combined detection of the three biomarkers has significant predictive value for patient prognosis, which is helpful for early clinical assessment and the formulation of intervention strategies. -
表 1 比较感染组和未感染组临床资料及血清HSP70、KLF5、MIP-2水平[n(%)/($ \bar x \pm s$)]
Table 1. Comparison of clinical data and serum HSP70,KLF5,and MIP-2 levels between infected and uninfected groups[n(%)/($ \bar x \pm s$)]
指标 感染组(n = 95) 未感染组(n = 100) t/χ2 P 年龄(岁) 67.24 ± 7.15 66.57 ± 6.92 0.665b 0.507 性别 1.506a 0.220 男 53(55.79) 47(47.00) 女 42(44.21) 53(53.00) COPD病程(年) 8.17 ± 2.24 7.85 ± 2.06 1.039b 0.300 吸烟史 55(57.89) 42(42.00) 4.923a 0.026* 基础疾病 高血压 27(28.42) 19(19.00) 2.399a 0.121 糖尿病 25(26.32) 17(17.00) 2.502a 0.114 接种疫苗 36(37.89) 54(54.00) 5.085a 0.024* 呼吸衰竭 32(33.68) 10(10.00) 16.171a < 0.001* 1年内加重次数(次) 12.234a < 0.001* ≥ 3 52(54.74) 30(30.00) < 3 43(45.26) 70(70.00) 入院前糖皮质激素使用史 21(22.11) 23(23.00) 0.022a 0.881 基线用药情况(LABA/LAMA/ICS) 0.766a 0.682 单独用药 23(24.21) 20(20.00) 联合用药 25(26.32) 31(31.00) 无上述用药 47(49.47) 49(49.00) 合并细菌感染 28(29.47) 25(25.00) 0.493a 0.483 FEV1% pred 42.27 ± 7.80 48.74 ± 9.22 5.277b < 0.001* CRP(mg/L) 53.39 ± 18.83 45.62 ± 11.45 5.287b < 0.001* HSP70(ng/mL) 24.74 ± 7.40 17.39 ± 4.25 8.558b < 0.001* KLF5(ng/mL) 6.68 ± 1.89 4.91 ± 1.53 7.204b < 0.001* MIP-2(pg/mL) 381.94 ± 57.05 317.75 ± 53.81 8.086b < 0.001* 注:合并细菌感染判定标准:痰培养检出致病菌(如肺炎链球菌、流感嗜血杆菌等)或血清降钙素原(PCT) > 0.5 ng/mL;*P < 0.05;a为χ2检验;b为t检验;LABA为长效β2受体激动剂,LAMA为长效抗胆碱能药物,ICS为吸入性糖皮质激素。 表 2 血清HSP70、KLF5、MIP-2与感染组患者相关临床指标水平的相关性
Table 2. Correlation between serum HSP70,KLF5,MIP-2 levels and relevant clinical indicators in infected patients
指标及赋值 HSP70 KLF5 MIP-2 r/rpb P r/rpb P r/rpb P 吸烟史(有 = 1,无 = 0) 0.085 0.233 0.063 0.297 0.101 0.156 接种疫苗(是 = 1,否 = 0) −0.112 0.125 −0.098 0.210 −0.077 0.289 呼吸衰竭(是 = 1、否 = 0) 0.472 < 0.001* 0.457 < 0.001* 0.581 < 0.001* 1年内加重次数(≥ 3次 = 1,< 3次 = 0) 0.464 < 0.001* 0.462 < 0.001* 0.574 < 0.001* FEV1% pred −0.577 < 0.001* −0.567 < 0.001* −0.503 < 0.001* CRP 0.573 < 0.001* 0.598 < 0.001* 0.487 < 0.001* *P < 0.05。 表 3 AECOPD患者并发RSV感染的多因素Cox回归分析
Table 3. Multivariate Cox regression analysis of factors associated with RSV infection in patients with AECOPD
自变量及赋值 β SE Waldχ2 P HR 95%CI 吸烟史(有 = 1,无 = 0) 0.710 0.405 3.073 0.080 2.034 0.920~4.499 接种疫苗(否 = 1,是 = 0) 0.652 0.375 3.026 0.082 1.920 0.921~4.004 呼吸衰竭(是 = 1、否 = 0) 0.750 0.362 4.298 0.038* 2.118 1.042~4.306 1年内加重次数(≥ 3次 = 1,< 3次 = 0) 0.906 0.366 6.131 0.013* 2.475 1.208~5.071 FEV1% pred(实测值) −0.478 0.219 4.765 0.029* 0.620 0.404~0.952 CRP(实测值) 0.833 0.324 6.615 0.010* 2.301 1.219~4.342 HSP70(实测值) 0.798 0.313 6.499 0.011* 2.221 1.203~4.102 KLF5(实测值) 0.956 0.406 5.539 0.019* 2.600 1.173~5.762 MIP-2(实测值) 0.829 0.321 6.669 0.010* 2.291 1.221~4.298 *P < 0.05。 表 4 比较轻、中、重度组血清HSP70、KLF5、MIP-2水平($ \bar x \pm s $)
Table 4. Comparison of serum HSP70,KLF5,and MIP-2 levels Among mild,moderate,and severe subgroups($ \bar x \pm s$)
组别 n HSP70(ng/mL) KLF5(ng/mL) MIP-2(pg/mL) 轻度组 31 13.17 ± 4.43 4.50 ± 1.49 317.08 ± 49.46 中度组 35 24.53 ± 7.82a 6.08 ± 1.74a 381.24 ± 58.65a 重度组 29 37.36 ± 10.07ab 9.73 ± 2.50ab 452.13 ± 63.23ab F − 73.253 57.369 41.589 P − < 0.001* < 0.001* < 0.001* *P < 0.05;与轻度组相比,aP < 0.05;与中度组相比,bP < 0.05。 表 5 比较预后良好、预后不良组血清HSP70、KLF5、MIP-2水平($ \bar x \pm s$)
Table 5. Comparison of serum HSP70,KLF5,and MIP-2 levels between good and poor prognosis subgroups($ \bar x \pm s$)
组别 n HSP70(ng/mL) KLF5(ng/mL) MIP-2(pg/mL) 预后良好组 44 17.97 ± 4.99 5.02 ± 1.53 331.13 ± 51.81 预后不良组 51 30.58 ± 9.48 8.11 ± 2.20 425.78 ± 61.57 t − 7.923 7.824 8.033 P − < 0.001* < 0.001* < 0.001* *P < 0.05。 表 6 感染组HSP70、KLF5、MIP-2高、低水平对患者预后不良的相对危险度分析
Table 6. Relative risk analysis of high and low levels of HSP70,KLF5,and MIP-2 for poor prognosis in the infected group
指标 预后良好(n = 44) 预后不良(n = 51) 相对危险度(95%CI) χ2 P HSP70 高水平 10 35 2.431(1.576~3.748) 19.961 < 0.001* 低水平 34 16 KLF5 高水平 14 35 2.054(1.331~3.168) 12.815 < 0.001* 低水平 30 16 MIP-2 高水平 8 33 2.415(1.609~3.625) 20.841 < 0.001* 低水平 36 18 *P < 0.05;HSP70、KLF5、MIP-2水平平均值分别为:24.74 ng/mL、6.68 ng/mL、381.94 pg/mL。 表 7 血清HSP70、KLF5、MIP-2水平对AECOPD合并RSV患者预后预测价值分析
Table 7. Analysis of the predictive value of serum HSP70,KLF5,and MIP-2 levels for prognosis in AECOPD patients with RSV infection
变量 AUC 截断值 95%CI 敏感度(%) 特异度(%) Youden指数 HSP70 0.812 21.68 ng/mL 0.719~0.885 72.55 79.55 0.521 KLF5 0.820 6.14 ng/mL 0.728~0.891 72.55 81.82 0.544 MIP-2 0.814 383.21 pg/mL 0.722~0.887 70.59 79.55 0.501 联合 0.922 − 0.849~0.967 86.27 84.09 0.704 -
[1] Xu Z, Li F, Xin Y, et al. Prognostic risk prediction model for patients with acute exacerbation of chronic obstructive pulmonary disease (AECOPD): A systematic review and meta-analysis[J]. Respir Res, 2024, 25(1): 410. doi: 10.1186/s12931-024-03033-4 [2] Gao P, Chen L, He L, et al. Respiratory virus infections and adenovirus characteristics during acute exacerbation of chronic obstructive pulmonary disease[J]. Technol Health Care, 2024, 32(6): 4203-4221. doi: 10.3233/THC-240010 [3] Mulpuru S, Andrew M K, Ye L, et al. Impact of respiratory viral infections on mortality and critical illness among hospitalized patients with chronic obstructive pulmonary disease[J]. Influenza Other Respir Viruses, 2022, 16(6): 1172-1182. doi: 10.1111/irv.13050 [4] 彭伟, 刘畅, 李勇, 等. 慢性阻塞性肺疾病急性加重患者血清热休克蛋白70和硫化氢水平变化及其与炎症因子关系[J]. 临床急诊杂志, 2020, 21(1): 74-78. [5] Zheng F, Liu T, Zhu J, et al. FoxF1 protects rats from paraquat-evoked lung injury following HDAC2 inhibition via the microRNA-342/KLF5/IκB/NF-κB p65 axis[J]. Exp Cell Res, 2020, 395(2): 112208. doi: 10.1016/j.yexcr.2020.112208 [6] Salama A, El-Fadaly A A, Elgohary R. Effect of atorvastatin on lipopolysaccharide-induced lung inflammation and hypoxia in mice; modulation of HIF-1α, CINC and MIP-2[J]. Immunopharmacol Immunotoxicol, 2025, 47(1): 85-93. doi: 10.1080/08923973.2024.2436089 [7] Agustí A, Celli B R, Criner G J, et al. Global initiative for chronic obstructive lung disease 2023 report: GOLD executive summary[J]. Eur Respir J, 2023, 61(4): 2300239. doi: 10.1183/13993003.00239-2023 [8] 岳佩瑜, 徐罕鲤, 陈双燕. AECOPD感染呼吸道合胞病毒对炎症反应及预后的意义[J]. 中华肺部疾病杂志(电子版), 2022, 15(1): 94-96. [9] Chen C Y J, Chen C Y J, Yew M S, et al. Predictors of influenza PCR positivity in acute exacerbations of chronic obstructive pulmonary disease[J]. Int J Chron Obstruct Pulmon Dis, 2022, 17: 25-32. doi: 10.2147/COPD.S338757 [10] 黄晓晨, 张永, 钱朝霞. 郑氏卧位康复操联合呼吸排痰阀对重度慢性阻塞性肺疾病患者的疗效观察[J]. 中华全科医学, 2023, 21(2): 259-262. [11] Collinson N, Snape N, Beagley K, et al. COPD is associated with elevated IFN-β production by bronchial epithelial cells infected with RSV or hMPV[J]. Viruses, 2021, 13(5): 911. doi: 10.3390/v13050911 [12] Yang X, Liao J, Zhu S, et al. Association of high-sensitivity CRP and FEV1%pred: A study on non-pulmonary disease in a population in Beijing, China[J]. BMJ Open Respir Res, 2024, 11(1): e001699. doi: 10.1136/bmjresp-2023-001699 [13] Hlapčić I, Grdić Rajković M, Čeri A, et al. Increased HSP70 and TLR2 gene expression and association of HSP70 rs6457452 single nucleotide polymorphism with the risk of chronic obstructive pulmonary disease in the Croatian population[J]. Diagnostics (Basel), 2021, 11(8): 1412. doi: 10.3390/diagnostics11081412 [14] Zhang B, Qi R. The dual-function of HSP70 in immune response and tumor immunity: From molecular regulation to therapeutic innovations[J]. Front Immunol, 2025, 16: 1587414. doi: 10.3389/fimmu.2025.1587414 [15] Li Q, Liao Y, Zeng J, et al. KLF5 shapes developing respiratory tubules by inhibiting actin asymmetry in epithelial cells[J]. Am J Respir Cell Mol Biol, 2025, 72(6): 663-677. doi: 10.1165/rcmb.2024-0140OC [16] 范素芳, 吕侯强, 张瑾. 慢性阻塞性肺疾病急性加重期合并Ⅱ型呼吸衰竭患者血清KLF5和CXCL12水平变化及意义[J]. 检验医学与临床, 2024, 21(19): 2806-2810. [17] 王太珊, 尹贵珍, 刘国跃. 非编码RNA在高氧性急性肺损伤中作用的研究进展[J]. 中华危重病急救医学, 2024, 36(4): 430-434. [18] 蔡溦, 朱御坤, 许建中. 骨关节炎中枢纽基因及在免疫浸润中作用的生物信息学分析与鉴定[J]. 中国组织工程研究, 2025, 29(18): 3747-3757. [19] 陈柳, 邱敏, 代解杰. 病原体感染角膜炎机制及动物模型研究进展[J]. 中国比较医学杂志, 2022, 32(4): 137-144. [20] Drouin M, Saenz J, Chiffoleau E. C-type lectin-like receptors: Head or tail in cell death immunity[J]. Front Immunol, 2020, 11: 251. doi: 10.3389/fimmu.2020.00251 [21] Kricker J A, Norris V, Page C, et al. Effects of EP395, a novel macrolide, on acute neutrophilic airway inflammation[J]. Pulm Pharmacol Ther, 2025, 90: 102364. doi: 10.1016/j.pupt.2025.102364 -





 下载:
下载: