Inhibitory Effect of Low-molecular-weight Heparin and Insulin Supplemented with Fenofibrate Capsules on Local Inflammation in Patients with Hypertriglyceridemic Acute Pancreatitis
-
摘要:
目的 探究低分子肝素、胰岛素联合非诺贝特的用药方案对高脂血症性急性胰腺炎(HL-SAP)患者局部炎症的影响。 方法 纳入2022年1月至2024年2月西安市第三医院消化内科收治的157例HL-SAP患者,随机分为常规组(n = 79)与联合组(n = 78),其中常规组采用常规治疗联合非诺贝特胶囊干预,给予联合组患者常规治疗联合低分子肝素、胰岛素辅以非诺贝特胶囊用药,观察两组症状、血脂水平、炎症因子、肝肾功能、胰腺酶学指标以及MCTSI评分、胰腺水肿、局部并发症、不良反应和疗效。 结果 相较常规组,联合组有效率明显提升(P < 0.05);治疗1周后联合组腹痛缓解时间、腹膜炎体征消失时间、胃肠功能恢复进程及住院时长均短于常规组(P < 0.05);联合组患者TC、TG和CRP、TNF-α及IL-6、ALT、AST、Scr、BUN、LPS、AMS、APACHE II评分及MCTSI评分改善情况较常规组更好(P < 0.05);联合组患者的胰腺水肿体积变小,改善情况优于常规组患者;并发症与不良反应发生情况联合组低于常规组(P < 0.05)。 结论 低分子肝素、胰岛素辅以非诺贝特胶囊能有效提高HL-SAP患者的临床疗效,降低炎症因子水平,稳定血脂,改善肝肾功能及胰腺酶学指标,同时可以减少患者胰腺局部并发症和不良反应,临床价值与治疗安全性良好,值得临床推广。 Abstract:Objective To investigate the effect of low-molecular-weight heparin, insulin, combined with fenofibrate on local inflammation in patients with hyperlipidemic acute pancreatitis (HL-SAP). Methods 157 HL-SAP patients admitted to the Gastroenterology Department of Xi'an Third Hospital from January 2022 to February 2024 were enrolled and randomly divided into a conventional group (n = 79) and a combined group (n = 78). The conventional group received standard treatment combined with fenofibrate capsules, while the combined group received standard treatment combined with low-molecular-weight heparin, insulin supplemented with fenofibrate capsules. The symptoms, blood lipid levels, inflammatory factors, liver and kidney functions, pancreatic enzyme indicators, MCTSI scores, pancreatic edema, local complications, adverse reactions and efficacy of the two groups were analyzed. Results Compared with the conventional group, the combined group showed significantly improved effectiveness (P < 0.05). After one week of treatment, the combined group had shorter times for abdominal pain relief, peritoneal sign resolution, gastrointestinal function recovery, and hospital stay (P < 0.05). The combined group showed better improvements in TC, TG, CRP, TNF-α, IL-6, ALT, AST, Scr, BUN, LPS, AMS, APACHE II scores, and MCTSI scores compared to the conventional group (P < 0.05). Pancreatic edema volume was smaller in the combined group, with superior improvement; complications and adverse reactions were lower in the combined group (P < 0.05). Conclusion Low-molecular-weight heparin, insulin combined with fenofibrate capsules can effectively improve clinical outcomes in HL-SAP patients, reduce inflammatory factor levels, stabilize blood lipids, improve liver and kidney function and pancreatic enzyme indicators, reduce local pancreatic complications and adverse reactions, and demonstrate good clinical value and treatment safety, warranting further clinical promotion. -
表 1 两组基线资料比较[($\bar x \pm s $)/n(%)]
Table 1. Comparison of baseline data between the two groups [($\bar x \pm s $)/n(%)]
指标 常规组(n=79) 联合组(n=78) t/χ2 P 男性 37(46.84) 38(48.72) 0.056 0.813 年龄(岁) 40.36 ± 6.76 39.45 ± 7.02 0.827 0.409 诊断间隔(h) 5.33 ± 1.34 5.16 ± 1.40 0.777 0.438 疾病程度 0.235 0.889 轻度 38(48.10) 39(50.00) 中度 24(30.38) 21(26.92) 重度 17(21.52) 18(23.08) 表 2 两组临床疗效比较[n = 76,n(%)]
Table 2. Comparison of clinical efficacy between the two groups[n = 76,n(%)]
组别 显效 有效 无效 有效率 常规组 11(14.47) 46(60.53) 19(25.00) 57(75.00) 联合组 48(63.16) 20(26.32) 8(10.53) 68(89.47) χ2 5.449 P 0.020* *P < 0.05。 表 3 两组腹痛缓解、腹膜炎体征、肠胃功能情况比较[n = 76,($\bar x \pm s $)]
Table 3. The relief of abdominal pain,peritonitis signs and gastrointestinal function of the two groups[n = 76, ($\bar x \pm s $)]
指标 常规组 联合组 t P 腹痛缓解时间(h) 47.53 ± 6.70 30.35 ± 6.27 16.322 <0.001* 腹膜炎体征消失时间(d) 5.62 ± 1.14 3.35 ± 0.89 13.683 <0.001* 肠胃功能恢复时间(d) 5.78 ± 1.48 4.15 ± 0.63 8.834 <0.001* *P < 0.05。 表 4 两组血脂情况比较[n = 76,($\bar x \pm s $)]
Table 4. Comparison of lipid profiles between the two groups[n = 76, ($\bar x \pm s $)]
指标 时间 常规组 联合组 t P TC(mmol/L) 治疗前 8.39 ± 2.90 7.97 ± 3.24 0.842 0.401 治疗后 6.73 ± 3.22 4.53 ± 2.25 4.882 <0.001* t 3.340 7.603 P 0.001△ <0.001△ TG(mmol/L) 治疗前 19.53 ± 6.23 19.35 ± 6.24 0.178 0.859 治疗后 7.98 ± 3.14 4.23 ± 2.76 7.820 <0.001* t 14.433 19.319 P <0.001△ <0.001△ 与常规组比较,*P < 0.05;与治疗前比较,△P < 0.05。 表 5 两组炎症因子情况比较[n = 76,($\bar x \pm s $)]
Table 5. Comparison of inflammatory factor conditions in the two groups[n = 76,($\bar x \pm s $)]
指标 时间 常规组 联合组 t P CRP(ng/L) 治疗前 58.42 ± 13.14 59.32 ± 13.36 −0.419 0.676 治疗后 19.85 ± 9.73 10.57 ± 6.34 6.966 <0.001* t 20.565 28.739 P <0.001△ <0.001△ TNF-α(ng/L) 治疗前 365.36 ± 13.05 363.46 ± 13.55 0.880 0.380 治疗后 236.31 ± 10.62 112.35 ± 10.03 73.979 <0.001* t 66.866 129.854 P <0.001△ <0.001△ IL-6(ng/L) 治疗前 65.25 ± 12.10 64.26 ± 11.33 0.521 0.603 治疗后 36.29 ± 8.94 22.59 ± 7.13 10.445 <0.001* t 16.782 27.137 P <0.001△ <0.001△ 与常规组比较,*P < 0.05;与治疗前比较,△P < 0.05。 表 6 两组肝肾功能比较[n = 76,($\bar x \pm s $)]
Table 6. Comparison of liver and kidney functions between the two groups[n = 76,($\bar x \pm s $)]
指标 时间 常规组 联合组 t P ALT(U/L) 治疗前 42.35 ± 5.21 41.98 ± 5.02 0.446 0.656 治疗后 35.67 ± 4.89 28.34 ± 3.56 10.565 <0.001* t 8.150 19.322 P <0.001△ <0.001△ AST(U/L) 治疗前 38.76 ± 4.89 39.12 ± 5.11 −0.444 0.658 治疗后 32.45 ± 4.21 25.67 ± 3.21 11.164 <0.001* t 8.525 19.430 P <0.001△ <0.001△ Scr(μmol/L) 治疗前 85.67 ± 6.32 86.23 ± 6.11 −0.555 0.579 治疗后 82.34 ± 5.89 75.45 ± 4.89 7.846 <0.001* t 3.360 12.009 P 0.001△ 0.009△ BUN(mmol/L) 治疗前 5.23 ± 0.87 5.31 ± 0.91 −0.554 0.580 治疗后 4.38 ± 0.76 4.12 ± 0.65 2.267 0.025* t 6.415 8.575 P <0.001△ <0.001△ 与常规组比较,*P < 0.05;与治疗前比较,△P < 0.05。 表 7 两组胰腺酶学指标、MCTSI评分对比[n = 76,($\bar x \pm s $)]
Table 7. Comparison of pancreatic enzyme indicators and MCTSI scores between the two groups[n = 76,($\bar x \pm s $)]
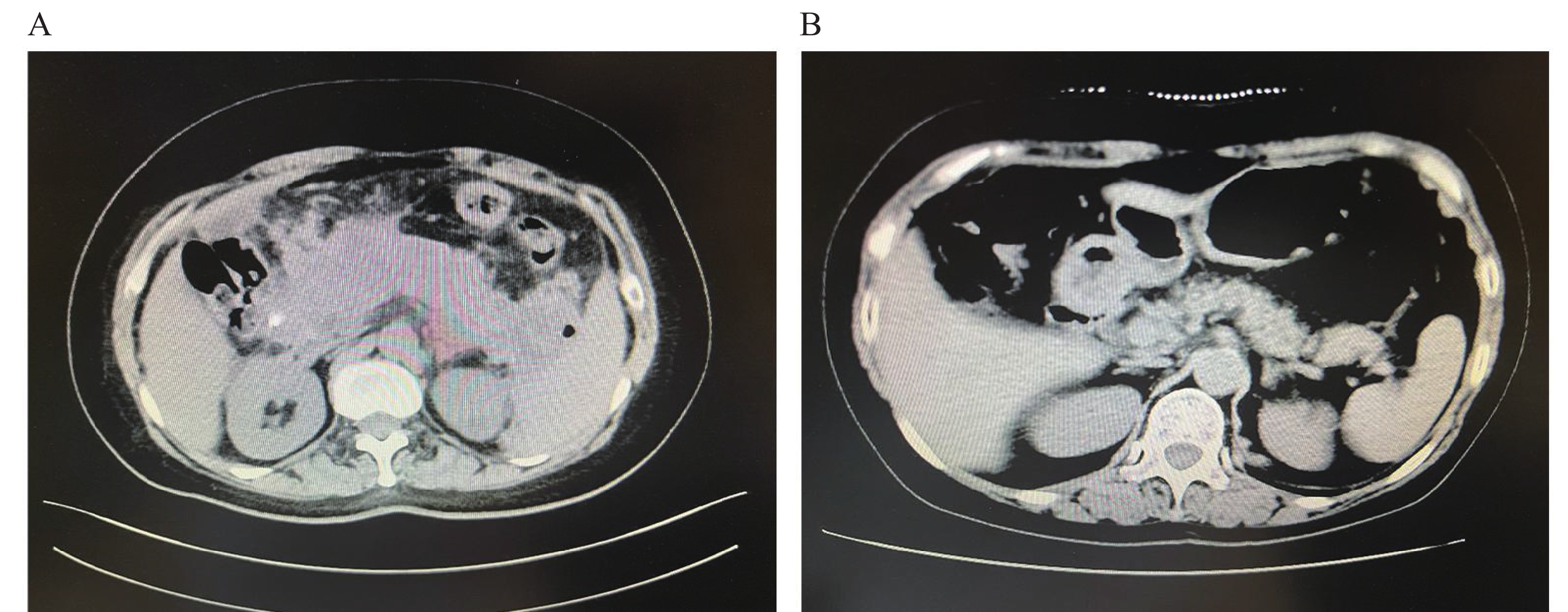
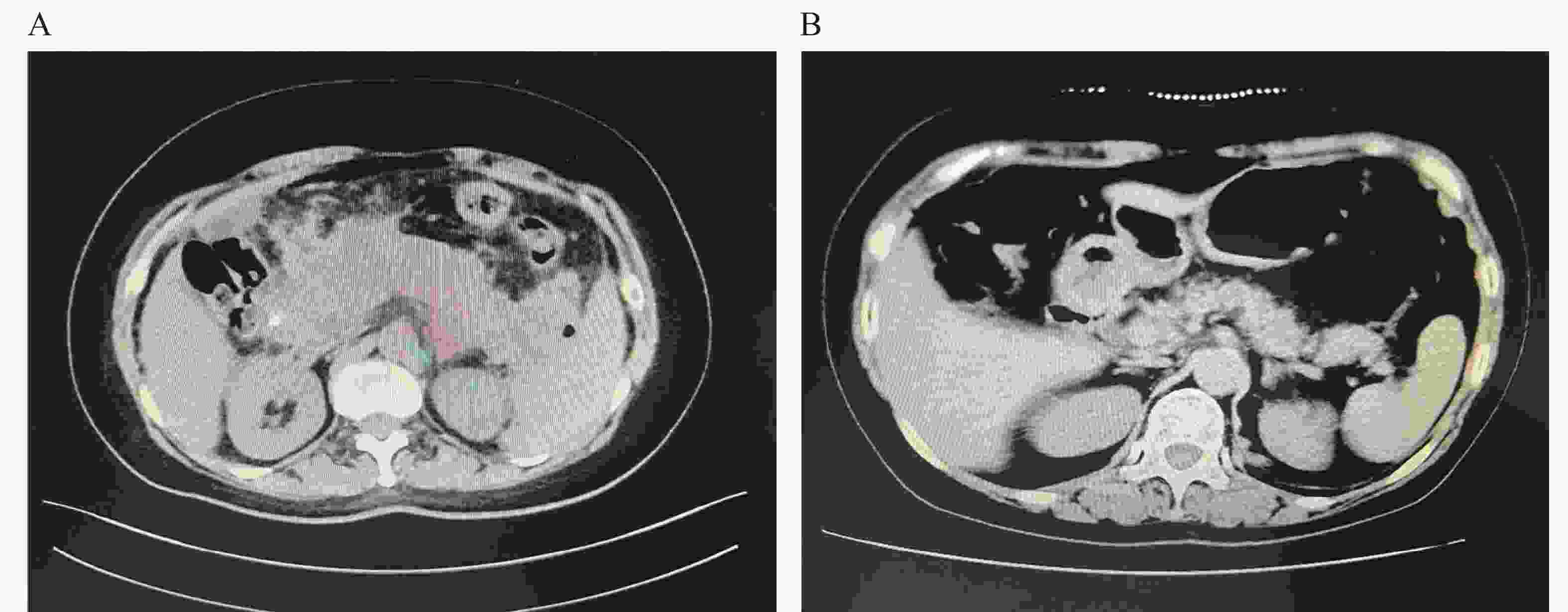
指标 时间 常规组 联合组 t P LPS(U/L) 治疗前 285.67 ± 32.12 288.90 ± 30.87 −0.632 0.528 治疗后 220.34 ± 28.90 150.12 ± 22.34 16.759 <0.001* t 13.181 31.750 P <0.001△ <0.001△ AMS(U/L) 治疗前 456.78 ± 45.23 460.12 ± 43.11 −0.466 0.642 治疗后 380.23 ± 35.67 280.45 ± 28.90 18.948 <0.001* t 11.585 30.179 P <0.001△ <0.001△ APACHE II(分) 治疗前 8.23 ± 1.23 8.34 ± 1.32 −0.532 0.596 治疗后 7.12 ± 1.01 5.34 ± 0.89 11.527 <0.001* t 6.080 16.428 P <0.001△ <0.001△ MCTSI(分) 治疗前 5.67 ± 0.98 5.78 ± 1.02 −0.678 0.499 治疗后 4.89 ± 0.87 3.21 ± 0.65 13.486 <0.001* t 5.189 18.524 P <0.001△ <0.001△ 与常规组比较,*P < 0.05;与治疗前比较,△P < 0.05。 表 8 两组胰腺体积对比[n = 76,($\bar x \pm s $)]
Table 8. Comparison of pancreatic volumes between the two groups[ n = 76, ($\bar x \pm s $)]
指标 时间 常规组 联合组 t P 胰腺体积(cm3) 治疗前 197.28 ± 16.53 197.44 ± 16.79 −0.059 0.953 治疗后 166.33 ± 15.29 140.50 ± 11.37 11.818 <0.001* t 11.983 24.480 P <0.001△ <0.001△ 与常规组比较,*P < 0.05;与治疗前比较,△P < 0.05。 表 9 两组胰腺局部并发症情况对比[n = 76,n(%)]
Table 9. Comparison of local pancreatic complications between the two groups[n = 76,n(%)]
组别 胰腺局部并发症 不良反应 胰腺肿大 胰腺周围积液 胰腺脓肿 总发生率 肌肉无力或酸痛 胃肠功能失调 过敏性皮肤反应 总发生率 常规组 17(22.37) 13(17.11) 11(14.47) 40(52.63) 13(17.11) 11(14.47) 12(15.79) 36(47.37) 联合组 9(11.84) 6(7.89) 5(6.58) 20(26.32) 2(2.63) 3(3.95) 3(3.95) 8(10.53) χ2 2.969 2.947 2.515 11.014 8.950 5.035 15.79 25.077 P 0.085 0.086 0.113 0.001* 0.003* 0.025* 3.95 <0.001* *P < 0.05。 -
[1] Zhong B. Clinical features and therapeutic strategies of hyperlipidemic acute pancreatitis[J]. Chinese General Practice, 2015, 13(7): 1088-1090. [2] 马宏娟, 潘国忠. 他汀联合贝特类降脂治疗的研究进展[J]. 中国心血管病研究杂志, 2014, 12(3): 258-261. [3] Qiao L S, Chen Y K, Luo G G, et al. Synergistic mechanism of traditional Chinese medicine based on target combination of PepT1 and PPARα[J]. Zhong Guo Zhong Yao Za Zhi, 2017, 42(11): 2146-2151. [4] 周南希. 他汀类药物与其他药物联用时所致不良反应的临床分析[J]. 中华养生保健, 2020, 38(11): 184-185. [5] Hong S J, Lee Y J, Lee S J, et al. Treat-to-target or high-intensity statin in patients with coronary artery disease: A randomized clinical trial[J]. JAMA, 2023, 329(13): 1078-1087. doi: 10.1001/jama.2023.2487 [6] 刘波, 罗强, 张毅, 等. 低分子肝素联合强化胰岛素在基层医院治疗高脂血症性急性胰腺炎的临床观察[J]. 医学理论与实践, 2019, 32(3): 322-324+347. [7] 董元航, 李宗远, 吴洪玉, 等. 生物化学标志物预测高脂血症性急性胰腺炎脏器衰竭的临床价值[J]. 中华胰腺病杂志, 2019, 19(4): 252-255. doi: 10.3760/cma.j.issn.1674-1935.2019.04.003 [8] 刘国雄, 匡桥贵, 喻欣荷, 等. 加味大承气汤治疗湿热蕴结型高脂血症性急性胰腺炎的疗效及作用机制[J]. 中国实验方剂学杂志, 2021, 27(5): 91-97. [9] Bahtouee M, Eghbali S S, Maleki N, et al. Acute physiology and chronic health evaluation II score for the assessment of mortality prediction in the intensive care unit: A single-centre study from Iran[J]. Nurs Crit Care, 2019, 24(6): 375-380. doi: 10.1111/nicc.12401 [10] Xu L, Yu H, Chen L, et al. The modified computed tomography severity index combined with low skeletal muscle mass can better predict the severity of hypertriglyceridemia-induced pancreatitis[J]. J Hepatobiliary Pancreat Sci, 2022, 29(12): 1336-1345. doi: 10.1002/jhbp.1198 [11] 杨晓佳, 赵凯亮, 李满, 等. NADPH氧化酶通过调节Akt/GSK3β通路参与高脂血症性急性胰腺炎大鼠胰腺损伤[J]. 中华急诊医学杂志, 2019, 28(12): 1501-1506. [12] Meng Y, Han P, Ma X, et al. Research progress on the mechanism of acute hypertriglyceridemic pancreatitis[J]. Pancreas, 2024, 53(8): e700-e709. doi: 10.1097/MPA.0000000000002364 [13] 宋觉非, 左芳. 前列地尔联合低分子肝素钙治疗高脂血症性胰腺炎的疗效观察[J]. 中国医药指南, 2019, 17(2): 67-68. [14] 戴伟, 周瑞祥, 严骏, 等. 低分子量肝素钙联合胰岛素治疗高脂血症性重症胰腺炎的临床观察[J]. 华中科技大学学报(医学版), 2020, 49(4): 500-503. [15] Chilbert M R, VanDuyn D, Salah S, et al. Combination therapy of ezetimibe and rosuvastatin for dyslipidemia: Current insights[J]. Drug Des Devel Ther, 2022, 16: 2177-2186. [16] 洪佳昌, 郭巍, 蔡素芳. 胰岛素联合低分子肝素对高脂血症性急性胰腺炎的影响[J]. 中国卫生标准管理, 2024, 15(16): 127-130. doi: 10.3969/j.issn.1674-9316.2024.16.030 [17] 邓丽芸, 肖涌, 刘劼, 等. 低分子肝素钙联合胰岛素治疗重症高脂血症性急性胰腺炎的疗效及对血清氧化应激和炎症因子的影响[J]. 广西医科大学学报, 2019, 36(2): 209-213. [18] Asghar R, Atefeh M, Mohammad R , et al. Association between serum levels of high sensitive C-reactive protein and inflammation activity in chronic gastritis patients[J]. Scandinavian Journal of Gastroenterology, 2016, 51(5): 531-537. [19] 周国强, 黄宗青, 张志, 等. 增强型体外反搏对缺血性脑卒中患者超敏C反应蛋白和内皮素1的影响[J]. 中国神经精神疾病杂志, 2016, 42(3): 129-133. [20] 董永春. 高脂血症性与胆源性急性胰腺炎患者血脂、血淀粉酶、尿淀粉酶水平的比较[J]. 胃肠病学和肝病学杂志, 2017, 26(7): 761-764. doi: 10.3969/j.issn.1006-5709.2017.07.012 [21] Salih Z, Mammdoh J, Taqa A. Evaluate the anti-inflammatory effects of nanocinnamon gel on salivary cytokines: Tumor necrosis factor-alpha(TNF-α)and interleukine-6(IL-6) in chronic gingivitis[J]. Al-Rafidain Dental Journal, 2021, 21(1): 62-74. doi: 10.33899/rden.2020.127851.1047 [22] 张莉, 陈美如, 陈倩, 等. 低分子肝素联合胰岛素对高脂血症性急性胰腺炎的疗效及预后观察[J]. 河北医药, 2023, 45(17): 2598-2602. [23] 郭晓丹, 周建华, 冯亚娟, 等. 柴芍承气汤联合低分子肝素对高脂血症性胰腺炎患者炎症介质、血脂水平及凝血功能的影响[J]. 中国实验方剂学杂志, 2018, 24(18): 175-179. [24] 陈俞兵, 周宇, 申屠刚. 胰岛素联合低分子肝素治疗高脂血症性急性胰腺炎的临床效果及安全性分析[J]. 中国中西医结合消化杂志, 2020, 28(5): 370-373. [25] 张艳青, 郭安兵, 彭利军. 血脂康胶囊联合非诺贝特胶囊治疗高脂血症性胰腺炎的疗效观察[J]. 临床和实验医学杂志, 2023, 22(17): 1809-1813. [26] 李非, 曹锋. 中国急性胰腺炎诊治指南(2021)[J]. 中国实用外科杂志, 2021, 41(7): 739-746. [27] Ozcelik S, Baş S, Ozcelik M, et al. Efficacy of insulin, heparin and fenofibrate combination treatment in severe hypertriglyceridemia: Double center experience[J]. Acta Endocrinol (Buchar), 2019, 15(4): 460-465. [28] Tolento Cortes L, Trinh J, Le M, et al. Safety and efficacy of insulin and heparin in the management of hypertriglyceridemia-Induced pancreatitis in a patient without diabetes: A case report[J]. Case Rep Endocrinol, 2022, 2022(1): 7905552. -





 下载:
下载: