Clinical Significance of Uterine Artery and Luteal Blood Flow Doppler Parameters Pregnancy of Uncertain Viability
-
摘要:
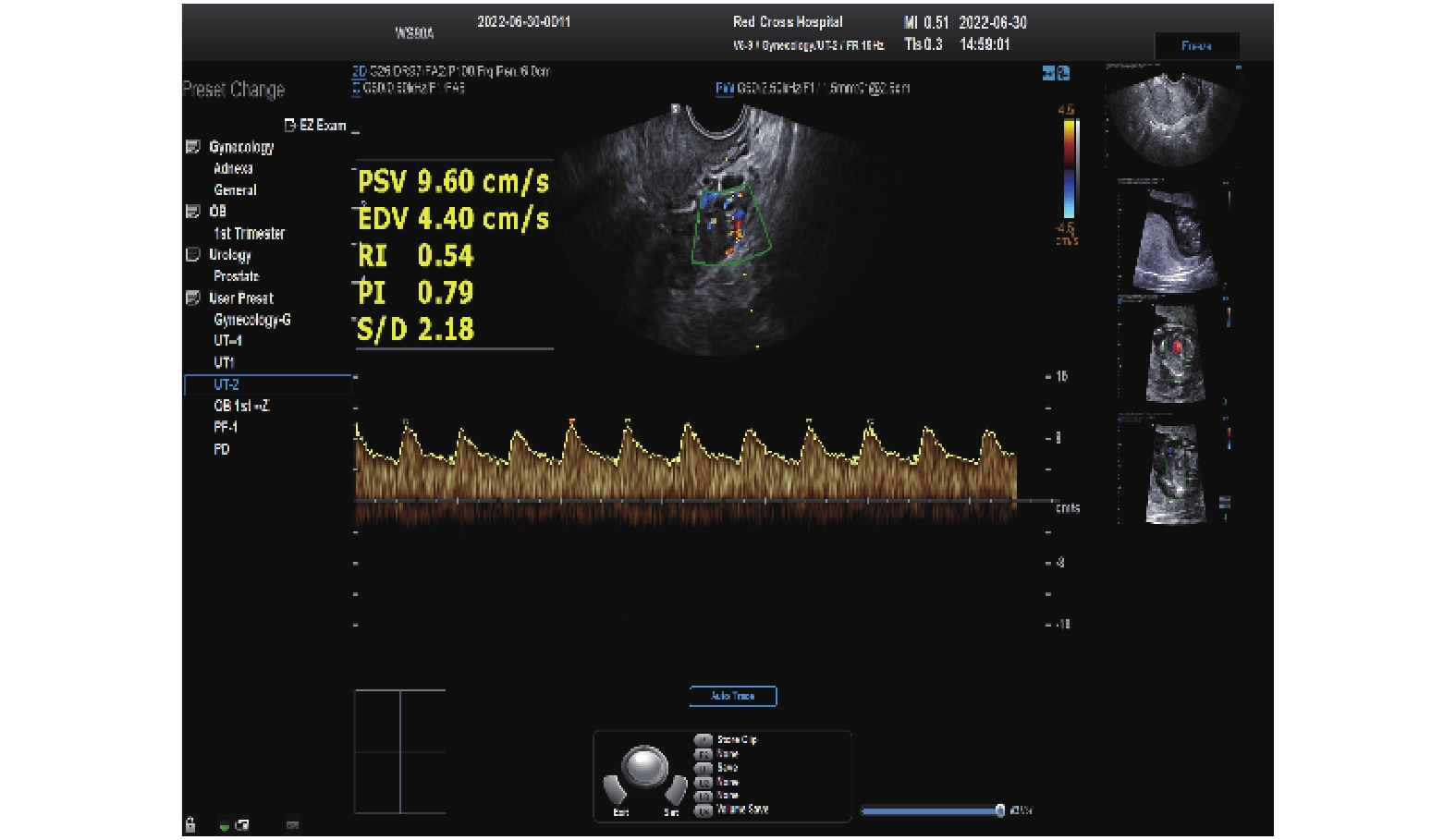
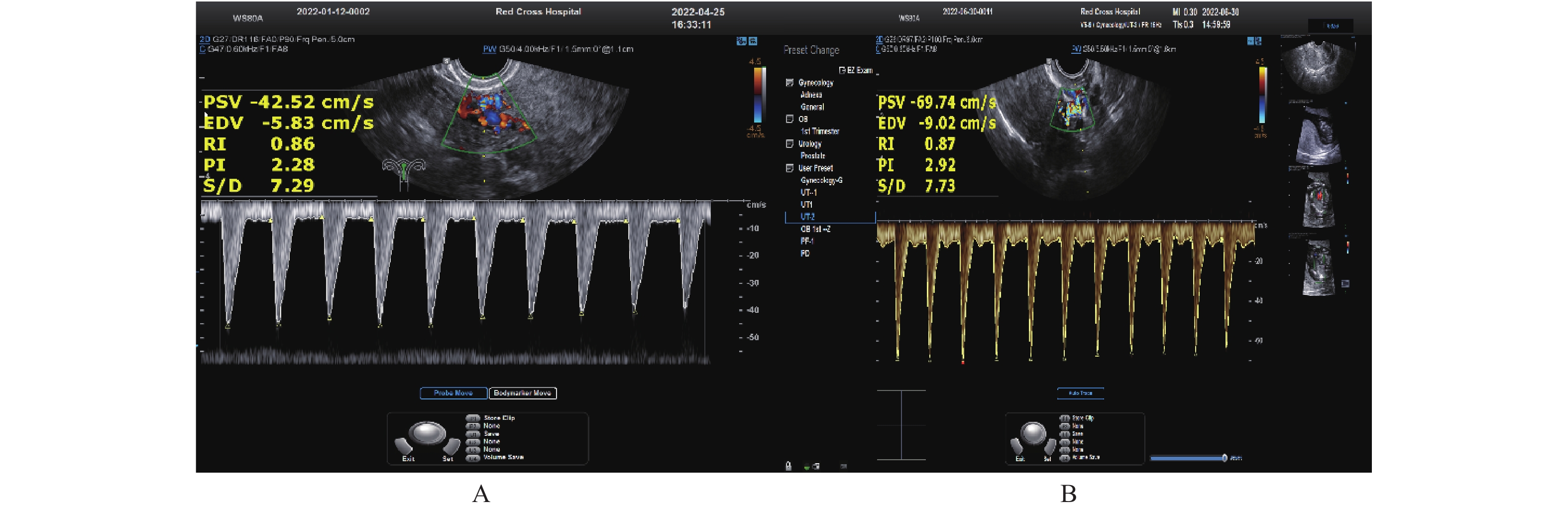
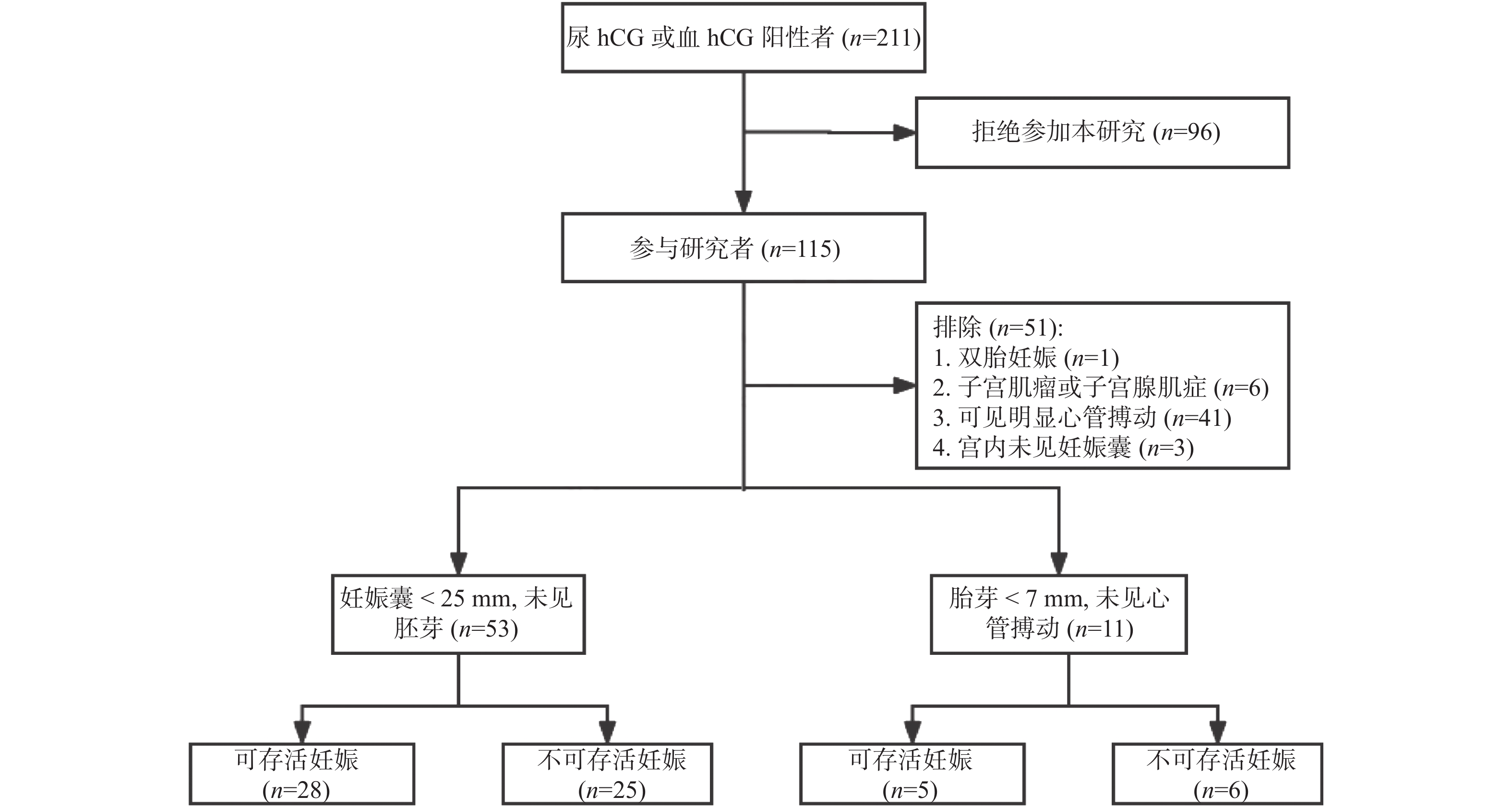
目的 探讨子宫动脉及黄体血流多普勒参数在早期妊娠不确定丢失中的临床意义。 方法 以64例早期妊娠胚胎存活力不确定的孕妇为研究对象,经阴道超声检查测量其子宫动脉及黄体血流参数,以随访后的明确诊断为依据,将不可存活宫内妊娠者纳入研究组,可存活宫内妊娠者纳入对照组。 结果 不可存活妊娠组mUAPI(2.16±0.50)、mUARI(0.82±0.07),低于可存活妊娠组mUAPI(2.93±0.48)、mUARI(0.89±0.05),差异有统计学意义(P < 0.05);不可存活妊娠组黄体血流PI(0.85±0.13)、RI(0.56±0.06)、高于对照组黄体血流PI(0.75±0.13)、黄体血流RI(0.50±0.06),差异有统计学意义(P < 0.05)。 结论 子宫动脉及黄体血流搏动指数对早期存活力不确定妊娠临床咨询有指导意义。 Abstract:Objective To explore the clinical significance of uterine artery and luteal flow Doppler parameters in pregnancy of uncertain viability. Methods A total of 64 women with pregnancy of uncertain viability in first trimester were selected as the research subjects. The uterine artery and luteal blood flow parameters were measured by transvaginal ultrasound. Based on the definite diagnosis after follow-up, non-viable intrauterine pregnancies were included in the study group, and viable intrauterine pregnancies were included in the control group. Results The mUAPI (2.16±0.50) and mUARI (0.82±0.07) in the non-viable pregnancy group were significantly lower than the mUAPI (2.93±0.48) and mUARI (0.89±0.05) in the viable pregnancy group, with statistically significant differences (P < 0.05). The luteal blood flow PI (0.85±0.13) and RI (0.56±0.06) in the non-viable pregnancy group were significantly higher than the luteal blood flow PI (0.75±0.13), luteal blood flow RI (0.50±0.06) in control group, with statistically significant ( P < 0.05). Conclusion Uterine artery and corpus luteum blood flow Doppler parameters are useful for guiding clinical consultations in pregnancies of uncertain viability. -
Key words:
- Ultrasonography /
- Abortion /
- Uterine artery /
- Corpus luteum
-
住院医师规范化培训(简称“住培”)已在中国实施多年,并逐渐从制度建设阶段过渡到以临床岗位胜任力为导向,以质量为核心的质量提升阶段,因此对临床教学提出了更高的要求[1−2]。高效的临床教学需要基于学习者的学习风格因材施教,以更好满足学习需求和教学要求[3]。近年来,由美籍教育工作者大卫库伯(David Kolb)所提出的Kolb学习风格受到了极大关注,并提出学习由具体实践(concrete experience,CE)、反思观察(reflective observation,RO)、抽象概念(abstract conceptualization,AC)和主动实践(active experimentation,AE) 4个学习环节构成[4]。4个阶段,2个学习环节分别组合形成了4个学习类型:发散型、吸收型、聚集型、调节型[5]。国内相关研究表明,基于学习者学习风格的教学有助于增加其学习态度的积极性,更便于学习者对课程的了解与把握,且不同教学风格与考核成绩相关[6]。临床医师岗位胜任力是指临床医师在平时诊疗管理工作中,熟练运用互动沟通技术、基础知识、手段、临床思维、情感表达及个人感受,从而使受到诊疗服务的个人和人群获益[7]。
目前,在临床医师岗位胜任力方面的相关研究,多从评价体系构建的角度出发,但从培养方面的探讨相对较少。所以,本研究将对住培生的Kolb学习风格和临床医师岗位胜任力进行现状研究,旨在了解临床医学实习生在临床实践中的学习风格,并分析比较不同学习风格实习生在临床医师岗位胜任力上的差异。为更有效地基于不同学习风格实习生,提升其临床医生岗位胜任力的临床带教方案的制定与实施提供参考。
1. 对象与方法
1.1 研究对象
2023年9月1日至2023年10月31日采用问卷星对昆明医科大学第一附属医院住培生进行问卷调查,纳入标准:参加住院医师规范化培训1 a以上;已完成包括内、外、妇、儿、急诊等科室的轮转;知情并同意参加本研究。排除标准:请假累计超过1个月。
1.2 研究方法
1.2.1 测评工具
(1)一般资料调查表:由本研究团队自行编制,包括性别、民族、年龄等个人基本信息。(2)Kolb学习风格量表(learning style inventory,LSI)[8]该量表是由Kolb等人基于经验学习理论编制,用于测评学习者学习风格偏好,其Cronbach’ s系数为0.81,内部效度与外部效度均较高。经验学习理论认为学习过程包括CE、AC、RO、AE 4个阶段。该量表由12个问题构成,学习者按照自身的偏好程度分别用1、2、3、4四个数字进行排序,12个问题中代表某学习阶段的部分选项的分数之和,即为该学习阶段的最终得分。按照学习者对四个阶段的偏好差异,把其互相对立存在的学习模式作为一个维度,将学习方式偏好分成2个维度,加工信息维度(主动实践-反思观察)中,若AE-RO≤6或AE-RO≥7分别为偏好反思分析和自主实践的学习模式;感知信息维度(抽象定义-具体经验)中,若AC-CE≤7或AC-CE≥8分别为偏好具体经验和抽象概念的学习模式。Kolb等由此建立了4个学习风格类别,发散型(AC-CE≤7及AE-RO≤6),吸收型(AC-CE≥8及AE-RO≤6),聚合型(AC-CE≥8及AE-RO≥7)和调节型(AC-CE≤7及AE-RO≥7),以此得出学习者的学习风格偏好。(3)临床医师岗位胜任力调查问卷[9]:采用的问卷是《中国临床医师岗位胜任力调查问卷》,由中国北方医学教育发展中心研制,通过李克特五级评分量表的方法,对临床医师的岗位胜任力状况开展了自主评估的研究[10]。问卷包括八个方面,分别涉及临床基本能力、医生职业精神与素养、医患沟通能力、学习与运用医学知识、团队合作能力、基本公共卫生服务能力、信息与管理能力、学术研究能力[11]。
1.2.2 资料收集方法
研究中对住培生的一般资料、Kolb学习风格和临床医师岗位胜任力使用问卷法,发放前,向调查对象阐明调查目的并讲解问卷填写方法,问卷填报完毕由调查员统一收集。
1.2.3 统计学方法
用SPSS 26.0对数据进行分析,计量资料以均数±标准差($ \bar x \pm s $)表示,组间比较采用单因素方差分析,计数资料以频数、百分比[n(%)]表示,P < 0.05为差异具有统计学意义。
2. 结果
2.1 住培生一般资料情况
本调查累计发出有效问卷200份,收集有效问卷163份,有效回收率82%,故选取163份有效问卷,进行数据分析。163名住培生中,男生67(40.9%),女生96(59.1%);汉族123名(75.5%),少数名族40(24.5%);年龄<25岁69人(42.3%),年龄≥25岁94人(57.7%)。
2.2 住培生学习风格类型情况
本研究163名住培生的学习风格类型中,偏好聚合型学习风格的人最多,共75人(46.1%),调节型、发散型次之,偏好吸收型学习风格的人最少,共22人(13.7%),见表1。
表 1 临床医学生学习风格类型($ \bar x \pm s $,n=163)Table 1. Types of learning styles of clinical medical students($ \bar x \pm s $,n=163)学习风格类型 n 百分比(%) 调节型 38 23.2 发散型 28 17.1 聚合型 75 46.1 吸收型 22 13.7 合计 163 100 2.3 不同学习风格临床专业医学生的临床医师岗位胜任力情况
不同学习风格临床专业医学生的临床医师岗位胜任力情况,比较四种不同学习风格住培生的岗位胜任力得分,吸收型得分最高,发散型、调节型次之,聚合型最低。吸收型学习风格的住培生在临床基本技能、医患沟通能力和团队合作能力上分数最高,调节型和发散型分别在掌握与运用医学知识、学术研究能力得分最高,差异均有统计学意义(P < 0.05)。而医生职业精神和素养、基本公共卫生服务能力和信息与管理能力3个方面的得分,比较差异无统计学意义(P > 0.05),见表2。
表 2 不同学习风格临床专业医学生的临床医师岗位胜任力情况[($ \bar x \pm s $),分]Table 2. Clinician post competency of clinical medical students with different learning styles[($ \bar x \pm s $),scores]项目 调节型 发散型 聚合型 吸收型 F P 岗位胜任力 3.83±0.66 3.91±0.56 3.80±0.40 4.28±0.71 3.74 <0.001* 临床基本能力 3.99±0.59 3.60±0.73 4.04±0.58 4.10±0.75 5.58 <0.001* 医生职业精神和素养 4.06±0.54 3.92±0.68 4.08±0.60 4.22±0.65 1.68 0.173 医患沟通能力 4.08±0.56 3.89±0.61 4.07±0.60 4.26±0.58 2.93 <0.001* 掌握与运用医学知识 4.10±0.71 3.72±0.74 4.07±0.59 3.98±0.57 3.31 <0.001* 团队合作能力 4.36±0.50 3.91±0.69 4.17±0.56 4.38±0.63 4.03 <0.001* 基本公共卫生服务能力 3.99±0.48 3.89±0.68 4.14±0.55 4.20±0.77 2.05 0.109 信息与管理能力 3.94±0.50 3.80±0.63 4.06±0.62 4.13±0.70 2.24 0.085 学术研究能力 3.82±0.67 4.14±0.74 4.01±0.64 4.07±0.81 3.27 <0.001* *P < 0.05。 3. 讨论
3.1 住培生的学习风格中以聚合型为主
本研究中,住培生的学习风格以聚合型(46.1%)为主,调节型(23.2%)和发散型(17.1%)次之,吸收型(13.7%)最少。本研究结果与郭蕾蕾等[12]研究结果:学生学习风格以调节型和聚合型为主,具有部分一致。但和Rassin等[13]的研究结论有所不同,国外学生则偏向于以发散型和吸收型为主。中外学生在学习风格上存在差距,可能由于中外教学理念和培训模式差异造成。
聚合型学习者较偏好抽象概念与主动实践,思考严谨,擅长掌握基础知识和处理现实问题,并通过演绎推理,发现问题,也擅长解决问题,但处理人际关系存在短板[14]。由此可见,虽然住培生以聚合型为主,对抽象理论和实际运用感兴趣,比较擅长利用理论知识和专业技术练习来提升临床能力,但相对欠缺想像力和把理论知识运用于实际的能力,不太重视人际关系和创新思维的培养。因此,面对临床问题能够更加理性面对、积极解决,但由于缺乏临床工作经验,在解决实际问题时仍存在短板。因此,在住培期间需要带教老师的讲解以及操作技术、临床实践能力的培训,使其在理论和技能得到全面发展。也要鼓励住培生积极进行沟通交流,促进协同发展,从而更好地处理临床工作,更好地为患者服务。
3.2 不同学习风格临床专业医学生的临床医师岗位胜任力分析
不同学习风格住培生的临床医师岗位胜任力之间差异有统计学意义(P < 0.05),其中,吸收型学习风格的住培生临床医师岗位胜任力得分最高。同时,该类型学习风格学生,在临床基本能力、医患沟通能力、团队合作能力均取得最高分数,且不同学习风格住培生,在此3方面间的差别也具有统计意义(P < 0.05)。可能与吸收型学习风格的住培生倾向于具体经验和主动实践,擅于依靠直接经验学习并付诸行动,且乐于与人交往[15]。本研究中,发散型学习风格的住培生在学术研究能力方面分数最高(P < 0.05),而在临床基本能力方面分数最低,此类学习风格的住培生想像力更加丰富、思维活跃,擅于理解人或通过观察的方法寻找解决的办法,但处理专业技术方面的工作能力稍有欠缺[16]。而临床医学的专业技术性较强,因此,根据发散型学习风格的住培生制订课程实施方案时,除了充分发挥其擅长观察教学和人际沟通等优点之外,同时需要克服相对弱点,多设置实际操作科目,训练动手作业的能力,使理论知识在实践中经一步强化。调节型学习风格的住培生的掌握与运用医学知识方面得分最高(P < 0.05),这种学习风格学习者思维能力强,对抽象概念和知识点了解扎实,但不擅长解决人际关系[17−18]。该类学习风格住培生,对理论知识的学习理解能力较强,但需要更多团队合作项目,以逐渐改善短板,提高综合能力。
由此可知,不同学习风格在岗位胜任力的不同方面有一定的倾向性,因此,通过对学习风格的了解,可以针对性的对不同学习风格类型的住培生开展相应培训,以整体提高住培生的临床医师岗位胜任力。
-
表 1 2组孕妇人口统计学特征及临床资料[($\bar x \pm s $)/n(%)]
Table 1. Demographic characteristics and clinical data of pregnant women in the two groups [($\bar x \pm s $)/n(%)]
人口统计学及临床特征 不可存活妊娠组 可存活妊娠组 χ2/t P 年龄(岁) 29.32 ± 5.08 27.00 ± 4.85 1.870 0.066 体重(kg) 54.00 ± 7.54 55.52 ± 10.07 −0.678 0.501 BMI(kg/㎡) 21.12 ± 3.02 21.52 ± 3.47 0.319 0.626 平均动脉压(mmHg) 85.35 ± 6.87 83.25 ± 5.78 1.024 0.067 停经时间(d) 49.4 ± 7.8 46.2 ± 8.3 1.768 0.089 是否吸烟 是 2(6.46) 1(3.03) 0.607# 否 29(93.54) 32(96.97) 孕次 1次(首次怀孕) 10(32.26) 11(33.33) 0.008 0.927 ≥2次 21(67.74) 22(66.67) 产次 0次(未经产) 14(45.16) 19(57.58) 0.986 0.321 ≥1次 17(54.84) 14(42.42) 血清hCG(IU/L) 7752.97 ± 4240.45 13926.00 ± 4958.90 −4.351 < 0.001* 胚芽 可见 6(19.35) 5(15.15) 0.198 0.656 未见 25(80.65) 28(84.85) 平均孕囊直径(mm) 14.8 ± 6.7 9.9 ± 3.7 3.609 0.001* BMI为体质指数(体重除以身高的平方);*P < 0.05。#该处P值由FISHER确切概率法所得,故无χ2值。 表 2 2组子宫动脉及黄体血流多普勒参数比较($\bar x \pm s $)
Table 2. Comparison of Doppler ultrasound parameters of uterine artery and luteal blood flow between two groups ($\bar x \pm s $)
组别 n 子宫动脉多普勒参数 黄体血流多普勒参数 mUARI mUAPI RI PI 不可存活组 31 0.82 ± 0.07 2.16 ± 0.50 0.56 ± 0.06 0.85 ± 0.13 可存活组 33 0.89 ± 0.05 2.93 ± 0.48 0.50 ± 0.06 0.75 ± 0.13 t −4.297 −6.228 3.481 3.001 P < 0.001* < 0.001* 0.001* 0.004* *P < 0.05。 -
[1] Doubilet P M,Benson C B,Bourne T,et al. Diagnostic criteria for nonviable pregnancy early in the first trimester[J]. N Engl J Med,2013,369(15):1443-1451. [2] Richardson A,Deb S,Campbell B,et al. Serum concentrations of Ang-2 and Flt-1 may be predictive of pregnancy outcome in women with pregnancies of uncertain viability:A phase I exploratory prognostic factor study[J]. J Obstet Gynaecol,2018,38(3):321-326. doi: 10.1080/01443615.2017.1353596 [3] Webster K,Eadon H,Fishburn S,et al. Ectopic pregnancy and miscarriage:Diagnosis and initial management:Summary of updated NICE guidance[J]. BMJ,2019,367(1):l6283. [4] Stamatopoulos N,Condous G. Ultrasound follow-up in the first trimester when pregnancy viability is uncertain[J]. Australas J Ultrasound Med,2017,20(3):95-96. [5] Doubilet P M,Benson C B,Bourne T,et al. Diagnostic criteria for nonviable pregnancy early in the first trimester[J]. New Engl J Med,2013,369(15):1443-1451. doi: 10.1056/NEJMra1302417 [6] Dane B,Batmaz G,Ozkal F,et al. Effect of parity on first-trimester uterine artery doppler indices and their predictive value for pre gnancy complications[J]. Gynecol Obstet Invest,2014,77(1):24-28. [7] Jauniaux E,Johnson M R,Jurkovic D,et al. The role of relaxin in the development of the uteroplacental circulation in early pregnancy[J]. Obstet Gynecol,1994,84(3):338-342. [8] Poon L C,Stratieva V,Piras S,et al. Hypertensive disorders in pregnancy:Combined screening by uterine artery Doppler,blood pressure and serum PAPP-A at 11-13 weeks[J]. Prenat Diagn,2010,30(3):216-223. doi: 10.1002/pd.2440 [9] Taylor T J,Quinton A E,De Vries B S,et al. First-trimester ultrasound features associated with subsequent miscarriage:A prospective study[J]. Aust N Z J Obstet Gynaecol,2019,59(5):641-648. doi: 10.1111/ajo.12944 [10] Guo J,Chaemsaithong P,Huang J,et al. Comparison of uterine artery Doppler measurements at 6 weeks of pregnancy after IVF between pregnanci es that resulted in miscarriage and ongoing pregnancies[J]. Int J Gynaecol Obstet,2021,152(2):249-255. doi: 10.1002/ijgo.13371 [11] Jauniaux E,Zaidi J,Jurkovic D,et al. Comparison of colour Doppler features and pathological findings in complicated early pregnancy[J]. Hum Reprod,1994,9(12):2432-2437. [12] Huppertz B,Weiss G,Moser G. Trophoblast invasion and oxygenation of the placenta:Measurements versus presumptions[J]. Journal of Reproductive Immunology,2014,101-102:74-79. [13] Brezinka C. 3D ultrasound imaging of the human corpus luteum[J]. Reproductive Biology,2014,14(2):110-114. doi: 10.1016/j.repbio.2013.11.002 [14] Henriquez S,Kohen P,Xu X,et al. Estrogen metabolites in human corpus luteum physiology:differential effects on angiogenic activity[J]. Fertil Steril,2016,106(1):230-237. [15] ] Takasaki A,Tamura H,Taniguchi K,et al. Luteal blood flow and luteal function[J]. Journal of Ovarian Research,2009,2(1):1. doi: 10.1186/1757-2215-2-1 [16] Tamura H,Takasaki A,Taniguchi K,et al. Changes in blood-flow impedance of the human corpus luteum throughout the luteal phase and during early pregnancy[J]. Fertil Steril,2008,90(6):2334-2339. doi: 10.1016/j.fertnstert.2007.10.056 [17] Sgs D T,Gda G,Bashir S T,et al. Follicle vascularity coordinates corpus luteum blood flow and progesterone production[J]. Reproduction Fertility and Development,2017,29(3):448-457. doi: 10.1071/RD15223 [18] Kanazawa T,Seki M,Iga K. Early pregnancy diagnosis based on luteal morphology and blood flow on Days 17-21 post-artificial insemination in Japanese Black cattle[J]. Theriogenology,2022,181:69-78. [19] Lek S M,Ku C W,Allen J C,et al. Validation of serum progesterone < 35 nmol/L as a predictor of miscarriage among women with threatened miscarriage[J]. BMC Pregnancy and Childbirth,2017,17(1):78. [20] Han H,Mo X,Ma Y,et al. The role of blood flow in corpus luteum measured by transvaginal two-dimensional and three-dimensional ultrasound in the prediction of early intrauterine pregnancy outcomes[J]. Frontiers in Pharmacology,2019,10(7):767. -






 下载:
下载:
 下载:
下载: