Clinical Analysis of Two Methods in the Treatment of Cholecystolithiasis Combined with Choledocholithiasis
-
摘要:
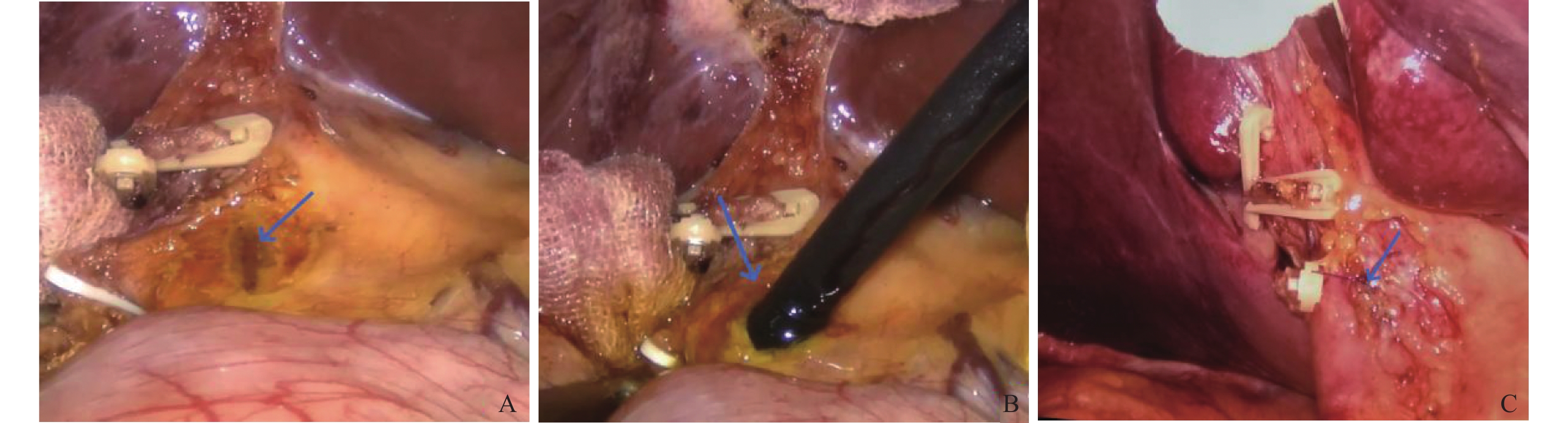
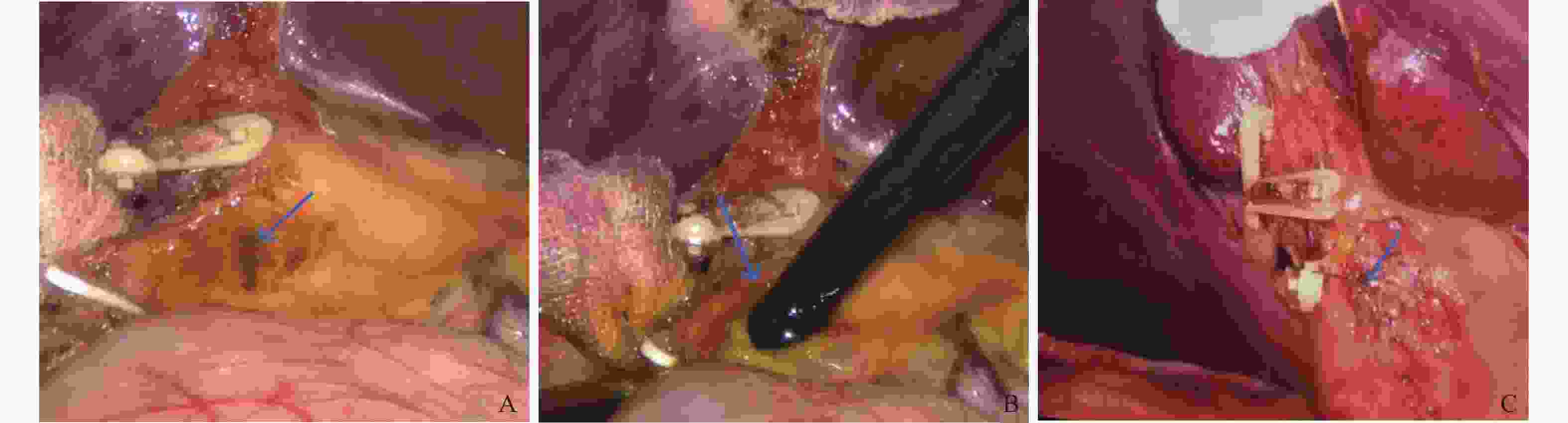
目的 比较腹腔镜胆囊切除术(LC)+腹腔镜胆总管探查一期缝合术(LBEPS)及LC+腹腔镜经胆囊管胆总管探查术(LTCBDE)2种术式的临床治疗效果。 方法 回顾性分析2018年1月至2023年6月昆明医科大学第二附属医院肝胆胰外科收治的64例采用LC+LBEPS及LC+LTCBDE治疗的胆囊结石并胆总管结石患者的临床资料,其中35例行LC+LBEPS,29例行LC+LTCBDE,比较2组患者的手术时间、术中出血量、腹腔引流时间、手术成功率、总住院时间、总住院费用、手术并发症发生率及结石复发率。 结果 2组患者基线资料、手术成功率及术后并发症发生率比较差异无统计学意义(P>0.05);LC+LBEPS组手术时间[160.00(150.00,167.50)] min vs [114.00(95.00,126.00)] min、术中出血量[30.00(27.40,40.00)] mL vs [22.00(20.00,25.00)] mL、腹腔引流时间[5.00(5.00,6.00)] d vs [3.00(3.00,4.00)] d、总住院时间(8.31±1.98 ) d vs(6.14±2.07 ) d及总住院费用[2.82(2.32,3.44)] 万元 vs [1.68(1.61,1.86)]万元均高于LC+LTCBDE组,差异有统计学意义(P < 0.05)。 结论 LC+LBEPS及LC+LTCBDE均是治疗胆囊结石并胆总管结石的2种免T管有效治疗方式,但LC+LTCBDE手术时间、术中出血量、腹腔引流时间、总住院时间、总住院费用更低,临床治疗效果更优,在满足手术适应症的前提下可优先选择。 Abstract:Objective To compare the clinical therapeutic effects of Laparoscopic cholecystectomy (LC) + laparoscopic common bile duct exploration and primary suture (LBEPS) and LC + laparoscopic common bile duct exploration through cystic duct (LTCBDE). Methods The clinical data of 64 patients with cholecystolithiasis complicated with choledocholithiasis treated by LC + LBEPS and LC + LTCBDE from January 2018 to June 2023 were analyzed retrospectively, including 35 patients with LC + LBEPS and 29 patients with LC + LTCBDE. Besides, the operation time, intraoperative bleeding, abdominal drainage time, operation success rate, total hospitalization time, total hospitalization expenses, surgical complications and stone recurrence rate between the two groups were compared. Results There was no significant difference in baseline data, surgical success rate and postoperative complication rate between these two groups (P > 0.05). The operation time, blood loss, abdominal drainage time, total hospitalization time and total hospitalization cost in the LC + LBEPS group were significantly higher than those in LC + LTCBDE group (P < 0.05). Conclusions LC + LBEPS and LC + LTCBDE are two effective treatment methods for cholecystolithiasis complicated with choledocholithiasis without T tube. However, LC + LTCBDE has lower operation time, intraoperative bleeding, abdominal drainage time, total hospitalization time and total hospitalization cost, as well as better clinical treatment effect, so that it can be preferred on the premise of meeting surgical indications. -
表 1 2组患者基线资料比较 [n(%)/($ \bar x \pm s$)/M(P25,P75)]
Table 1. Comparison of baseline data between two groups of patients [n(%)/($\bar x \pm s $)/M(P25,P75)]
项目 LC+LBEPS组(n=35) LC+LTCBDE组(n=29) Z/t/χ2 P 性别 男 14(40.0) 14(48.3) 0.441 0.506 女 21(60.0) 15(51.7) 年龄(岁) 48.49±17.84 51.90±18.29 0.753 0.454 胆总管直径(cm) 1.10(1.00,1.20) 1.10(1.00,1.20) −0.145 0.885 结石直径(cm) 0.60(0.50,0.60) 0.60(0.50,0.70) −1.598 0.110 结石个数(个) 2.00(2.00,3.00) 2.00(2.00,3.00) −0.445 0.656 合并高血压 6(17.1) 5(17.2) Fisher 1.00 合并糖尿病 6(17.1) 4(13.8) Fisher 1.00 谷丙转氨酶(U/L) 90.00(86.50,100.50) 93.00(80.00,100.00) −0.655 0.513 谷草转氨酶(U/L) 98.00(88.00,120.00) 100.00(86.00,110.00) −0.716 0.474 谷氨酰转肽酶(U/L) 216.00(179.50,231.00) 218.00(174.50,233.00) −0.263 0.792 总胆红素(mmol/L) 48.83±15.92 46.93±18.94 0.436 0.665 表 2 2组患者手术相关指标比较 [n(%)/M(P25,P75)/($\bar x \pm s $)]
Table 2. Comparison of surgery-related indexes between the two groups [n(%)/M(P25,P75)/($\bar x \pm s $)]
观察指标 LC+LBEPS组(n=35) LC+LTCBDE组(n=29) t P 手术成功率 35(100.0) 26(89.7) Fisher 0.088 手术时间(min) 160.00(150.00,167.50) 114.00(95.00,126.00) −6.285 <0.001* 术中出血量(mL) 30.00(27.40,40.00) 22.00(20.00,25.00) −4.290 <0.001* 腹腔引流时间(d) 5.00(5.00,6.00) 3.00(3.00,4.00) −6.274 <0.001* 总住院天数(d) 8.31±1.98 6.14±2.07 4.291 <0.001* 总住院费用(万元) 2.82(2.32,3.44) 1.68(1.61,1.86) −6.413 <0.001* *P < 0.05。 表 3 2组患者术后并发症比较 [ n(%)]
Table 3. Comparison of postoperative complications between the two groups [ n(%)]
项目 LC+LBEPS组 LC+LTCBDE组 P 胆漏 3(8.6) 0(0.0) 0.245 出血 0(0.0) 0(0.0) − 残余结石 1(2.9) 2(6.9) 0.586 胆管炎 0(0.0) 0(0.0) − 胆管狭窄 1(2.9) 0(0.0) 1.00 结石复发 1(2.9) 0(0.0) 1.00 总并发症 6(17.1) 2(6.9) 1.00 -
[1] Lujian P,Xianneng C,Lei Z. Risk factors of stone recurrence after endoscopic retrograde cholangiopancreatography for common bile duct stones[J]. Medicine (Baltimore),2020,99(27):e20412. [2] Tian H L,Zhou J,Bai D S,et al. Comparison of repeated recurrence of common bile duct stones and occurrence of hepatolithiasis after synchronous laparoscopic cholecystectomy combined with laparoscopic common bile duct exploration or with endoscopic sphincterotomy: A 10-year retrospective study[J]. J Gastrointest Surg,2023,27(6):1167-1176. doi: 10.1007/s11605-023-05645-5 [3] Navaratne L, AI-Musawi J, Vutipongsatorn K, et al. Leveraging access to technology and enhanced surgical technique (LATEST) in laparoscopic bile duct exploration (LBDE)[J]. Surg Endosc,2023,37(3):2367-2378. [4] Bhardwaj A M,Trehan K K,Sharma V. Laparoscopic common bile duct exploration after failed endoscopic retrograde cholangio-pancreatography: Our patient series over a period of 10 years[J]. J Minim Access Surg,2022,18(4):533-538. doi: 10.4103/jmas.jmas_207_21 [5] Shao M Y, Aburrous M, Huson D, et al. Development and validation of a hybrid simulator for ultrasound-guided laparoscopic common bile duct exploration[J]. Surg Endosc,2023,37(9):6943-6953. [6] Yin Y,He K,Xia X. Comparison of primary suture and t-tube drainage after laparoscopic common bile duct exploration combined with intraoperative choledochoscopy in the treatment of secondary common bile duct stones: A single-center retrospective analysis[J]. J Laparoendosc Adv Surg Tech A,2022,32(6):612-619. doi: 10.1089/lap.2021.0418 [7] Deng Y,Tian H W,He L J,et al. Can t-tube drainage be replaced by primary suture technique in laparoscopic common bile duct exploration? A meta-analysis of randomized controlled trials[J]. Langenbecks Arch Surg,2020,405(8):1209-1217. doi: 10.1007/s00423-020-02000-z [8] 段建文,袁磊,孙运鹏,等. 腹腔镜一步法与内镜联合腹腔镜两步法治疗80岁以上胆囊结石合并胆总管结石的疗效比较[J]. 中华肝胆外科杂志,2023,29(3):185-189. [9] 李珂佳,刘昂,李炎阳,等. 同步三镜联合胆管一期缝合技术在胆囊结石合并扩张性胆总管结石患者中的应用[J]. 昆明医科大学学报,2022,43(7):134-139. [10] Pavlidis E T, Pavlidis T E. Current management of concomitant cholelithiasis and common bile duct stones[J]. World J Gastrointest Surg,2023,15(2):169-176. [11] 郭志唐,魏东,李伟思,等. 全麻仰卧位下同步双镜联合在Ⅰ型Mirizzi综合征并胆总管结石手术中的应用价值[J]. 中华普通外科杂志,2020,35(9):681-684. [12] Lee S J,Choi I S,Moon J I,et al. Optimal treatment for concomitant gallbladder stones with common bile duct stones and predictors for recurrence of common bile duct stones[J]. Surg Endosc,2022,36(7):4748-4756. doi: 10.1007/s00464-021-08815-1 [13] Pan L,Chen M,Ji L,et al. The safety and efficacy of laparoscopic common bile duct exploration combined with cholecystectomy for the management of cholecysto-choledocholithiasis: An up-to-date meta-analysis[J]. Ann Surg,2018,268(2):247-253. doi: 10.1097/SLA.0000000000002731 [14] Huang X X,Wu J Y,Bai Y N,et al. Outcomes of laparoscopic bile duct exploration for choledocholithiasis with small common bile duct[J]. World J Clin Cases,2021,9(8):1803-1813. doi: 10.12998/wjcc.v9.i8.1803 [15] Hori T. Comprehensive and innovative techniques for laparoscopic choledocholithotomy: A surgical guide to successfully accomplish this advanced manipulation[J]. World J Gastroenterol,2019,25(13):1531-1549 doi: 10.3748/wjg.v25.i13.1531 [16] Huang J, Hu W, Liu J, et al. Laparoscopic transcystic common bile duct exploration: 8-year experience at a single institution[J]. J Gastrointest Surg,2023,27(3):555-564. [17] Wahi J E, Warmack T, Barghout R, et al. Five-year experience with transcystic laparoscopic common bile duct exploration[J]. J Laparoendosc Adv Surg Tech A,2023,33(3):276-280. [18] Fang L,Huang J,Zheng H,et al. Laparoscopic transcystic common bile duct exploration in patients with a nondilated common bile duct[J]. Ann Palliat Med,2021,10(12):12845-12856. doi: 10.21037/apm-21-3609 [19] 武亚东,汪栋,徐维宇,等. 日间手术与次日出院的腹腔镜经胆囊管胆道探查取石术回顾性病例对照研究[J]. 国际外科学杂志,2022,49(12):825-832. [20] 张井虹,尚海涛,刘军舰,等. 腹腔镜胆总管一期缝合与内镜取石治疗继发性胆总管结石的临床疗效比较[J]. 中国普通外科杂志,2021,30(8):877-885. [21] 刘楠, 刘奇, 陈德兴. 腹腔镜下经胆囊管切开胆总管探查取石术的研究进展[J]. 中国微创外科杂志(中英文),2024,24(5):363-368. [22] 张志,李晓松,屠政斌,等. "隔膜"切开技术在腹腔镜经胆囊管胆总管探查术中的应用分析[J]. 中华肝胆外科杂志,2023,29(9):651-654. [23] 曾明文,凌俊,万文武,等. 两种微创手术治疗胆囊结石合并胆总管结石的疗效比较[J]. 中国普通外科杂志,2022,31(2):160-167. [24] 冯矗,罗浩,左亮,等. 腹腔镜胆囊切除联合胆道镜经胆囊管探查取石术与经胆总管取石术治疗胆囊合并胆总管结石的疗效比较[J]. 同济大学学报(医学版),2023,44(1):105-109 [25] 彭沙沙,裴斐. 腹腔镜胆囊管汇入部微切开胆总管探查取石一期缝合术的临床疗效[J]. 国际外科学杂志,2022,49(8):528-532. -





 下载:
下载: