Association of Mismatch Repair Deficiency and Clinicopathological Parameters in Patients withLeft and Right-side Sporadic Colon Cancer
-
摘要:
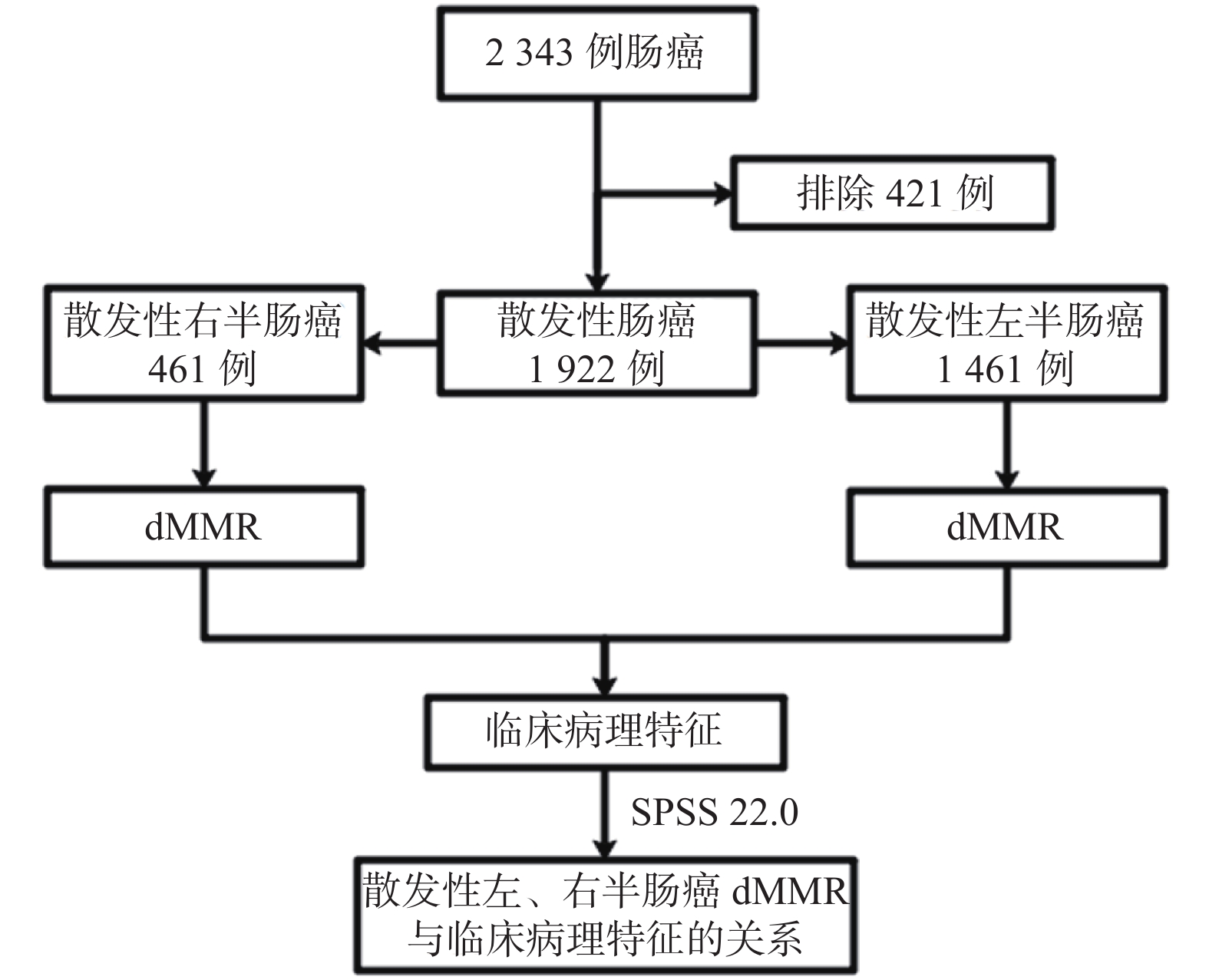
目的 在散发性左、右半肠癌中分别分析错配修复蛋白功能缺失(deficient mismatch repair,dMMR)与临床病理特征的相关性。 方法 收集昆明医科大学第一附属医院2014年1月至2019年9月经病理证实为腺癌的1 922例患者的临床病理资料,分别在散发性左、右半肠癌中分析dMMR与性别、年龄、体重指数(body mass index,BMI)、民族、血型、术前癌胚抗原(carcino-embryonic antigen,CEA)水平、病理类型、肿瘤分化程度、肿瘤直径、pT分期、pN分期、淋巴结检出数目、远处转移、(union for international cancer control,UICC)UICC分期、脉管侵犯、神经侵犯的关联。 结果 共有1922例散发性肠癌符合纳入标准,散发性右半肠癌患者占23.99%(461/1922),散发性左半肠癌患者占76.01%(1461/1922)。所有散发性肠癌患者dMMR率为23.47%(451/1922),散发性右半肠癌dMMR率38.83%(179/461);散发性左半肠癌dMMR率18.62%(272/1461)。与既往研究一致的是,所有散发性肠癌的dMMR更多见于年龄 < 62岁(OR = 1.551,P < 0.001)、右半肠癌(OR = 2.603,P < 0.001)、肿瘤直径≥4 cm(OR = 1.362,P = 0.009)、病理分化程度为中低分化(OR = 1.538,P = 0.046)、低分化(OR = 2.124,P = 0.013)及未分化(OR = 1.850,P = 0.045)、UICC分期I~II期(OR = 1.340,P = 0.014)、无神经侵犯者(OR = 1.407,P = 0.004)。在散发性右半肠癌中,dMMR多见于年龄 < 62岁(OR = 1.888,P = 0.001),pT1~T2(OR = 3.778,P = < 0.001)以及肿瘤直径≥4 cm者(OR = 1.856,P = 0.012);在散发性左半肠癌中,dMMR多见于年龄 < 62岁(OR = 1.525,P = 0.002),肿瘤直径≥4 cm(OR = 1.391,P = 0.016),无神经侵犯(OR = 1.454,P = 0.009)。 结论 不论肠道肿瘤原发部位如何,dMMR均多见于年龄 < 62岁,肿瘤直径≥4 cm者,而无神经侵犯及pT1~T2分别多见于散发性左半及右半肠癌。 -
关键词:
- 散发性结直肠癌 /
- 错配修复蛋白功能缺失 /
- 左半肠癌 /
- 右半肠癌 /
- 临床病理特征
Abstract:Objective To analyze the correlation between mismatch repair-deficient (dMMR) and clinicopathological characteristics in left and right-side sporadic colorectal cancers. Methods The clinicopathological data of 1922 patients who were pathologically confirmed as adenocarcinoma from January 2014 to September 2019 in the First Affiliated Hospital of Kunming Medical University were collected, and the dMMR and gender, age, and body mass index (BMI), ethnicity, blood type, preoperative CEA level, pathological type, tumor differentiation, tumor diameter, T stage, N stage, number of lymph nodes detected, distant metastasis, UICC stage, vascular invasion, perineural invasion were analyzed in sporadic left and right colorectal cancers. Results A total of 1922 cases of sporadic colorectal cancer met the inclusion criteria. Patients with sporadic right-side colon cancer accounted for 23.99% (461/1922), and patients with sporadic left-side colorectal cancer accounted for 76.01% (1461/1 922). The dMMR rate of all patients with sporadic colorectal cancer was 23.47% (451/1922), the dMMR rate of sporadic right-side colon cancer was 38.83% (179/461), and the dMMR rate of sporadic left-side colorectal cancer was 18.62% (272/1461). Consistent with previous studies, the dMMR of all sporadic colorectal cancers in this study is more common in age < 62 years (OR = 1.551, P < 0.001), right-side colon (OR = 2.603, p < 0.001), tumor diameter≥4 cm (OR = 1.362, P = 0.009), the degree of pathological differentiation is moderate-poorly differentiated (OR = 1.538, P = 0.046), poorly differentiated (OR = 2.124, P = 0.013)and undifferentiated (OR = 1.850, P = 0.045)), UICC stages I~II (OR = 1.340, P = 0.014), and patients without perineural invasion (OR = 1.407, P = 0.004). In sporadic right colon cancer, dMMR is more common in patients younger than 62 years old (OR = 1.888, P = 0.001), pT1~T2 (OR = 3.778, P = 0.000)and tumor diameter≥4 cm (OR = 1.856, p = 0.012); in sporadic left-side colorectal cancer, dMMR is more common in age < 62 years (OR = 1.525, P = 0.002), tumor diameter ≥4 cm (OR = 1.391, P = 0.016), and no perineural invasion (OR = 1.454, P = 0.009). Conclusions Regardless of the primary site of intestinal tumors, dMMR is more common in patients younger than 62 years and tumor diameter≥4 cm, while no perineural invasion and pT1~T2 are more common in sporadic left-side and right-side colorectal cancers, respectively. -
结直肠癌(colorectal cancer,CRC)是常见的消化道恶性肿瘤,其发病率及死亡率分别占恶性肿瘤中第三位和第二位[1],通常由微卫星不稳定(microsatellite instability,MSI)、染色体不稳定(chromosomal instability,CIN)及CpG岛甲基化3条途径引起[2-3]。新近研究证实,由微卫星不稳定途径引发的微卫星高度不稳定(microsatellite instability-high,MSI-H)/错配修复蛋白缺失(deficient mismatch repair protein,dMMR)状态的肠癌患者预后较好[4-5],通过检测MSI-H/dMMR可指导结直肠癌化疗药物的选择[6],用于结直肠癌患者预后评估[7]。MSI-H/dMMR分别可通过多重荧光聚合酶链反应(polymerase chain reaction,PCR)及免疫组化(immunohistochemistry,IHC)进行检测,两者特异性及敏感性均 > 90%[8],可认为MSI-H≈dMMR,由于IHC价格低廉、耗时较短[9],因此临床上更多用IHC进行检测。
既往研究提示dMMR状态与结直肠癌患者临床病理特征存在相关性[10]。dMMR更多见于年轻、右半结肠、低分化、肿瘤直径更大,粘液腺癌[11]以及UICC分期为I~II期[12]的结直肠癌患者。
为分析散发性左、右半肠癌dMMR与临床病理特征的相关性,笔者收集了1 922例散发性肠癌患者资料,分析散发性左、右半肠癌dMMR状态与临床病理特征的关联。
1. 对象与方法
1.1 实验对象
收集昆明医科大学第一附属医院2014年1月至2019年9月共计2343例所有散发性肠癌患者资料,其中1922例符合入组标准。散发性右半肠癌患者占23.99%,散发性左半肠癌患者占76.01%。男女比例为1.43:1;中位年龄62岁;CEA < 5 ng/mL占61.34%,CEA≥5 ng/mL占38.66%;中位肿瘤直径为4 cm;病理类型:普通腺癌89.07%,粘液腺癌2.86%,混合腺癌(普通腺癌+粘液腺癌)8.07%;肿瘤分化程度:高分化肿瘤14.62%;中高分化肿瘤31.01%;中分化肿瘤42.09%;中低分化肿瘤6.71%,低分化肿瘤2.81%,未分化肿瘤2.76%;pT分期:pT1~T2者24.14%,pT3~T4者75.86%;淋巴结转移者40.48%,淋巴结未转移者59.52%,UICC分期:I~II期者57.54%,III~IV期者42.46%,淋巴结数目 < 12个28.93%,淋巴结数目≥12个71.07%,远处转移5.78%,无远处转移94.22%,脉管侵犯者21.75%,无脉管侵犯者78.25%,神经侵犯者39.33%,无神经侵犯者60.67%,见表1。本研究为单中心临床回顾性研究,经伦理委员会批准,豁免签署病人知情同意书。
表 1 1922例散发性肠癌MMR表达与临床病理特征的关系[n(%)]Table 1. Relationship between different MMR status and clinicopathological characteristics of all patients with sporadic colorectal cancer in the cohort [n(%)]临床病理特征 MMR χ2 P pMMR(n = 1471) dMMR(n = 451) 性别 0.612 0.434 男 872(77.17) 258(22.83) 女 599(75.63) 193(24.37) 年龄(岁) 13.188 < 0.001* < 62 675(72.89) 251(27.11) ≥62 796(79.92) 200(20.08) BMI(kg/m2) 0.309 0.857 < 18.5 136(77.71) 39(22.29) 18.5~24 854(76.11) 268(23.89) ≥24 481(76.96) 144(23.04) 民族 0.174 0.677 汉族 1409(76.45) 434(23.55) 少数民族 62(78.48) 17(21.52) 血型 1.236 0.744 A+(Rh+) 507(76.70) 154(23.30) B+(Rh+) 381(74.85) 128(25.15) O+(Rh+) 453(77.44) 132(22.56) AB+(Rh+) 130(77.84) 37(22.16) CEA(ng/mL) 2.514 0.113 < 5 888(75.32) 291(24.68) ≥5 583(78.47) 160(21.53) 肿瘤部位 79.708 < 0.001* 右半肠癌 282(61.17) 179(38.83) 左半肠癌 1189(81.38) 272(18.62) 病理学类型 13.165 0.001* 普通腺癌 1331(77.75) 381(22.25) 粘液腺癌 35(63.64) 20(36.36) 混合腺癌 105(67.74) 50(32.26) 病理分化程度 26.828 < 0.001* 高 224(79.72) 57(20.28) 中高 471(79.03) 125(20.97) 未 33(62.26) 20(37.74) 中低 87(67.44) 42(32.56) 低 31(57.41) 23(42.59) 中 625(77.26) 184(22.74) 肿瘤直径(cm) 22.392 < 0.001* < 4 715(81.53) 162(18.47) ≥4 756(72.34) 289(27.66) pT 分期 4.538 0.209 T1 69(83.13) 14(16.87) T2 286(75.07) 95(24.93) T3 750(75.45) 244(24.55) T4 366(78.88) 98(21.12) pT 分期 0.000 0.988 T1~T2 355(76.51) 109(23.49) T3~T4 1116(76.54) 342(23.46) pN 分期 6.651 0.084 N0 853(74.56) 291(25.44) N1 409(78.65) 111(21.35) N2a 111(81.02) 26(18.98) N2b 98(80.99) 23(19.91) 清扫淋巴结数目 15.782 < 0.001* < 12 459(82.55) 97(17.45) ≥12 1012(74.08) 354(25.92) 远处转移 0.203 0.652 阴性 1388(76.64) 423(23.36) 阳性 83(74.77) 28(25.23) UICC 分期 7.366 0.061 Ⅰ 279(75.00) 93(25.00) Ⅱ 547(74.52) 187(25.48) Ⅲ 569(79.92) 143(20.08) Ⅳ 76(73.08) 28(26.92) UICC 分期 4.972 0.026* Ⅰ-Ⅱ 826(74.68) 280(25.32) Ⅲ-Ⅳ 645(79.04) 171(20.96) 脉管侵犯 2.417 0.120 阴性 1163(77.33) 341(22.67) 阳性 308(73.68) 110(26.32) 神经侵犯 6.090 0.014* 阴性 870(74.61) 296(23.59) 阳性 601(79.50) 155(20.50) *P < 0.05。 1.2 纳入与排除标准
纳入标准:(1)经手术切除病理学证实为腺癌的散发性肠癌;(2)临床病理信息完善者。
排除标准:(1)经手术切除病理学证实为非腺癌的肠癌;(2)遗传性肠癌(家族性腺瘤性息肉病、Lynch综合征及其他类型遗传性肠癌);(3)异时性或同时性多重癌;(4)术前接受新辅助治疗者[14];(5)临床病理信息不全者。
1.3 观测指标
本研究以脾曲为界,近端为右半结肠,远端为左半结直肠。分别在散发性左、右半肠癌中收集错配修复蛋白(MLH1、MSH2、MSH6、PMS2)、性别、年龄、体重指数(BMI)、民族、血型、术前CEA水平、肿瘤部位、病理类型、肿瘤分化程度、肿瘤直径、pT分期、pN分期、淋巴结检出数目、远处转移、UICC分期、脉管侵犯(+)、神经侵犯(+)共18项临床病理数据。
1.4 MMR检测
1.4.1 MMR检测方法
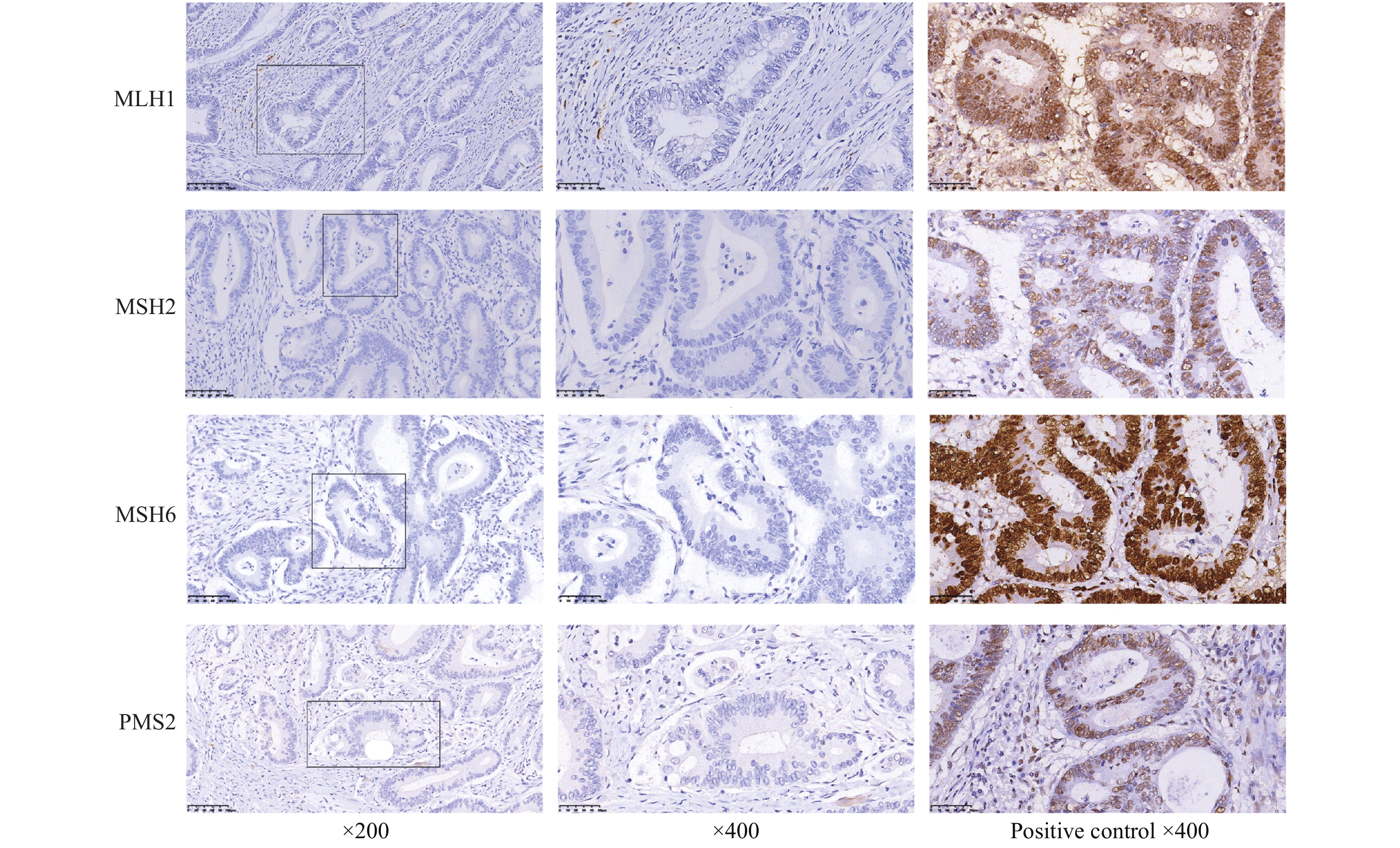
所有标本均经 10% 中性甲醛液固定、石蜡包埋、HE 染色。免疫组化采用 Max Vision 二步法,石蜡切片脱蜡、水化后 PBS 冲洗,过氧化物酶阻断剂封闭内源性过氧化酶活性,加入一抗,室温孵育,加生物素标记的二抗,加链霉素抗生物素的过氧化酶溶液,孵育后滴加 DAB 显色,苏木素复染,常规脱水,透明,封片。一抗为MSH2、MSH6、MLH1及PMS2,抗体及所用免疫组化试剂均购于中国福州迈新生物技术开发有限公司。
1.4.2 MMR结果判定
4种蛋白的判断标准一致[15-16],结果由2名资深病理医师双盲独立观察评估。4种蛋白阳性表达均位于细胞核中,呈棕褐色;以正常上皮细胞或淋巴细胞作为阳性内对照,4个错配修复蛋白(MLH1、MSH2、MSH6、PMS2)均阳性表达时可判定为错配修复蛋白功能完整(proficient mismatch repair,pMMR);4种蛋白中任意一个或几个出现表达缺失时,判定为错配修复蛋白功能缺失(deficient mismatch repair,dMMR)。
1.5 统计学处理
采用SPSS 22.0统计软件进行统计学分析;计数资料采用率(%)表示,各项临床病理因素与错配蛋白表达之间的单因素分析选用χ2检验或Fisher确切概率法;多因素分析采用二元Logistic回归模型,P < 0.05为差异具有统计学意义。
2. 结果
2.1 1 922例散发性肠癌错配修复蛋白功能缺失情况
1 922例患者dMMR率为23.47%,右半肠癌dMMR率38.83%;左半肠癌dMMR率18.62%。其中MLH1、MSH2、MSH6及PMS2分别单独表达缺失者分别为46例(2.39%)、18例(0.94%)、14例(0.73%)及146例(7.60%),MLH1与PMS2共同缺失者131例(6.82%),MSH2与MSH6共同缺失者23例(1.20%),4 种蛋白共同缺失者11例(0.57%),其他形式蛋白缺失者62例(3.23%),见图2,表2。
表 2 1922例散发性肠癌dMMR表型情况[n(%)]Table 2. Different dMMR phenotype of all patients with sporadic colorectal cancer in the cohort [n(%)]dMMR 总数 比率(%) 右半肠癌 左半肠癌 MLH1 46 2.39(46/1922) 10(0.52) 36(1.87) MSH2 18 0.94(18/1922) 5(0.26) 13(0.68) MSH6 14 0.73(14/1922) 4(0.21) 10(0.52) PMS2 146 7.60(146/1922) 49(2.55) 97(5.05) MLH1 + PMS2 131 6.82(131/1922) 71(3.69) 60(3.12) MSH2 + MSH6 23 1.20(23/1922) 15(0.78) 8(0.42) MLH1 + MSH2 + MSH6 + PMS2 11 0.57(11/1922) 3(0.16) 8(0.41) Other* 62 3.23(62/1922) 22(1.14) 40(2.08) Other*:MLH1 + MSH2(14例);MLH1 + MSH6(4例);MSH2 + PMS2(10例);MSH6 + PMS2(11例);MLH1 + MSH2 + MSH6(5例);MLH1 + MSH2+PMS2(10例);MLH1 + MSH6 + PMS2(4例);MSH2 + MSH6 + PMS2(4例)。 2.2 1 922例散发性肠癌dMMR与临床病理特征的关系
在1 922例散发性肠癌中,dMMR与临床病理特征的单因素分析结果提示,dMMR与年龄,肿瘤直径,分化程度、肿瘤部位、病理类型、神经侵犯、淋巴结检出数目及UICC分期相关,见表1;多因素分析结果提示,dMMR更多见于年龄 < 62岁,右半结肠癌、肿瘤直径≥4 cm、中低分化、低分化及未分化、UICC分期为I~II期及无神经侵犯者,见表3。
表 3 1922例散发性肠癌dMMR与临床病理特征的多因素分析Table 3. Multivariate results of the relationship between dMMR status and clinicopathological features of all patients with sporadic colorectal cancer in the cohort临床病理特征 dMMR OR 95% CI P 年龄(岁) < 62 1.551 1.243~1.936 < 0.001* ≥62 Reference 肿瘤部位 右半肠癌 2.603 2.044~3.314 < 0.001* 左半肠癌 Reference UICC 分期 I~II 1.340 1.062~1.691 0.014* III~IV Reference 病理分化程度 高 0.818 0.578~1.157 0.256 中高 0.884 0.677~1.153 0.363 未 1.850 1.013~3.377 0.045* 中低 1.538 1.008~2.346 0.046* 低 2.124 1.169~3.861 0.013* 中 Reference 肿瘤直径(cm) ≥4 1.362 1.079~1.719 0.009* < 4 Reference 神经侵犯 阴性 1.407 1.112~1.787 0.004* 阳性 Reference *P < 0.05。 2.3 461例散发性右半肠癌dMMR与临床病理特征的关系
在461例散发性右半肠癌中,dMMR与临床病理特征的单因素分析结果提示,dMMR与年龄,肿瘤浸润深度相关,见表4;其中本研究的散发性右半肠癌的卡方分析发现,不论肿瘤直径如何,其与dMMR不相关(P = 0.074),但既往文献[17]及本研究中所有肠癌的dMMR与肿瘤直径存在相关性,将其与年龄,肿瘤浸润深度进行多因素分析发现,散发性右半肠癌中dMMR更多见于年龄 < 62岁,pT1~T2,肿瘤直径≥4 cm者,见表5。
表 4 461例散发性右半肠癌MMR与临床病理特征的关系[n(%)]Table 4. Relationship between different MMR status and clinicopathological characteristics of the 461 patients with right-side colon cancer in the cohort [n(%)]临床病理特征 MMR χ2 P pMMR dMMR 性别 282 179 0.244 0.621 男 161(62.16) 98(37.84) 女 121(59.90) 81(40.10) 年龄(岁) < 62 112(53.85) 96(46.15) 8.562 0.003* ≥62 170(67.19) 83(32.81) BMI(kg/m2) < 18.5 29(61.70) 18(38.30) 0.125 0.940 18.5~24 180(61.64) 112(38.36) ≥24 73(59.83) 49(40.17) 民族 汉族 271(60.90) 174(39.10) 0.401 0.527 少数民族 11(68.75) 5(31.25) 血型 A+(Rh+) 104(63.80) 59(36.20) 1.800 0.615 B+(Rh+) 74(60.16) 49(39.84) O+(Rh+) 83(61.48) 52(38.52) AB+(Rh+) 21(52.50) 19(47.50) CEA(ng/mL) < 5 153(57.74) 112(42.26) 3.097 0.078 ≥5 129(65.82) 67(34.18) 病理学类型 普通腺癌 242(63.02) 142(36.98) 4.509 0.105 粘液腺癌 5(38.46) 8(61.54) 混合腺癌 35(54.69) 29(45.31) 病理分化程度 高 37(61.67) 23(38.33) 8.505 0.130 中高 93(64.58) 51(35.42) 未 5(38.46) 8(61.54) 中低 22(51.16) 21(48.84) 低 11(45.83) 13(54.17) 中 114(64.41) 63(35.59) 肿瘤直径(cm) < 4 79(67.52) 38(32.48) 2.662 0.103 ≥4 203(59.01) 141(40.99) pT 分期 T1 8(61.54) 5(38.46) 21.877 < 0.001* T2 13(31.71) 28(68.29) T3 165(60.22) 109(39.78) T4 96(72.18) 37(27.82) pT 分期 T1~T2 21(38.89) 33(61.11) 12.786 < 0.001* T3~T4 261(64.13) 146(35.87) pN 分期 N0 162(57.45) 120(42.55) 6.438 0.092 N1 79(64.75) 43(35.25) N2a 18(64.29) 10(35.71) N2b 23(79.31) 6(20.69) 清扫淋巴结数目 < 12 28(63.64) 16(36.36) 0.124 0.724 ≥12 254(60.91) 163(39.09) 远处转移 阴性 265(61.34) 167(38.66) 0.085 0.771 阳性 17(58.62) 12(41.38) UICC 分期 Ⅰ 17(36.96) 29(63.04) 13.943 0.003* Ⅱ 140(62.50) 84(37.50) Ⅲ 109(66.87) 54(33.13) Ⅳ 16(57.14) 12(42.86) UICC 分期 Ⅰ-Ⅱ 157(58.15) 113(41.85) 2.508 0.113 Ⅲ-Ⅳ 125(65.45) 66(34.55) 脉管侵犯 阴性 209(61.65) 130(38.35) 0.125 0.724 阳性 73(59.84) 49(40.16) 神经侵犯 阴性 160(58.19) 115(41.81) 2.565 0.109 阳性 122(65.59) 64(34.41) *P < 0.05。 表 5 461例散发性右半肠癌dMMR与临床病理特征的多因素分析Table 5. Multivariate results of the relationship between dMMR status and clinicopathological features of the 461 patients with right-side colon cancer临床病理特征 dMMR OR 95% CI P 年龄(岁) < 62 1.888 1.276~2.793 0.001* ≥62 Reference pT 分期 T1~T2 3.778 2.020~7.064 < 0.001* T3~T4 Reference 肿瘤直径(cm) ≥4 1.856 1.144~3.009 0.012* < 4 Reference *P < 0.05。 2.4 1461例散发性左半肠癌dMMR与临床病理特征的关系
在1461例散发性左半肠癌中,dMMR与临床病理特征的单因素分析结果提示,dMMR与年龄,肿瘤分化程度,肿瘤直径,检出淋巴结数目,有无神经侵犯有关,见表6;多因素结果分析提示,散发性左半肠癌中dMMR更多见于年龄 < 62岁,肿瘤直径≥4 cm及无神经侵犯者,见表7。
表 6 1461例散发性左半肠癌MMR与临床病理特征的关系 [n(%)]Table 6. Relationship between different MMR status and clinicopathological characteristics of the 1461 patients with left-side colon cancers in the cohort [n(%)]临床病理特征 MMR χ2 P pMMR dMMR 性别 1189 272 0.087 0.768 男 711(81.63) 160(18.37) 女 478(81.02) 112(18.98) 年龄(岁) < 62 563(78.41) 155(21.59) 8.222 0.004* ≥62 626(84.25) 117(15.75) BMI(kg/m2) < 18.5 107(83.59) 21(16.41) 0.454 0.797 18.5~24 674(81.20) 156(18.80) ≥24 408(81.11) 95(18.89) 民族 汉族 1138(81.40) 260(18.60) 0.008 0.929 少数民族 51(80.95) 12(19.05) 血型 A+(Rh+) 403(80.92) 95(19.08) 2.805 0.423 B+(Rh+) 307(79.53) 79(20.47) O+(Rh+) 370(82.22) 80(17.78) AB+(Rh+) 109(85.83) 18(14.17) CEA(ng/mL) < 5 735(80.42) 179(19.58) 1.506 0.220 ≥5 454(83.00) 93(17.00) 病理学类型 普通腺癌 1089(82.00) 239(18.00) 4.278 0.118 粘液腺癌 30(71.43) 12(28.57) 混合腺癌 70(76.92) 21(23.08) 病理分化程度 高 187(84.62) 34(15.38) 12.764 0.026* 中高 378(83.63) 74(16.37) 未 28(70.00) 12(30.00) 中低 65(75.58) 21(24.42) 低 20(66.67) 10(33.33) 中 511(80.85) 121(19.15) 肿瘤直径(cm) < 4 636(83.68) 124(16.32) 5.538 0.019* ≥4 553(78.89) 148(21.11) pT 分期 T1 61(87.14) 9(12.86) 1.815 0.612 T2 273(80.29) 67(19.71) T3 585(81.25) 135(18.75) T4 270(81.57) 61(18.43) pT 分期 T1~T2 334(81.46) 76(18.54) 0.002 0.960 T3~T4 855(81.35) 196(18.65) pN 分期 N0 691(80.16) 171(19.84) 2.581 0.461 N1 330(82.91) 68(17.09) N2a 93(85.32) 16(14.68) N2b 75(81.52) 17(18.48) 清扫淋巴结数目 < 12 431(84.18) 81(15.82) 4.070 0.044* ≥12 758(79.87) 191(20.13) 远处转移 阴性 1123(81.44) 256(18.56) 0.046 0.830 阳性 66(80.49) 16(19.51) UICC 分期 Ⅰ 262(80.37) 64(19.63) 3.456 0.327 Ⅱ 407(79.80) 103(20.20) Ⅲ 460(83.79) 89(16.21) Ⅳ 60(78.95) 16(21.05) UICC 分期 Ⅰ-Ⅱ 669(80.02) 167(19.98) 2.381 0.123 Ⅲ-Ⅳ 520(83.20) 105(16.80) 脉管侵犯 阴性 954(81.89) 211(18.11) 0.971 0.324 阳性 235(79.39) 61(20.61) 神经侵犯 阴性 710(79.69) 181(20.31) 4.340 0.037* 阳性 479(84.04) 91(15.96) *P < 0.05。 表 7 1461例散发性左半肠癌dMMR与临床病理特征的多因素分析Table 7. Multivariate results of the relationship between dMMR status and clinicopathological features of the 1461 patients with left-side colon cancer临床病理特征 dMMR OR 95% CI P 年龄(岁) < 62 1.525 1.166~1.995 0.002* ≥62 Reference 肿瘤直径(cm) ≥4 1.391 1.064~1.819 0.016* < 4 Reference 神经侵犯 阴性 1.454 1.096~1.928 0.009* 阳性 Reference *P < 0.05。 3. 讨论
结直肠癌中,dMMR与年轻、右半结肠、肿瘤直径更大、检出淋巴数目更多以及病理分期等临床病理因素有关[10]。由于左、右半肠癌在流行病学、病理、细胞遗传及分子特征等方面存在明显的差异,1990年,Bufill[18]提出近端和远端结直肠癌即左右半结肠癌是两种截然不同的肿瘤,然而,在散发性左、右半肠癌中,dMMR与上述结论是否一致目前未知;本研究以横结肠脾曲为界,在散发性左、右半肠癌中分别分析dMMR与不同临床病理特征的相关性。
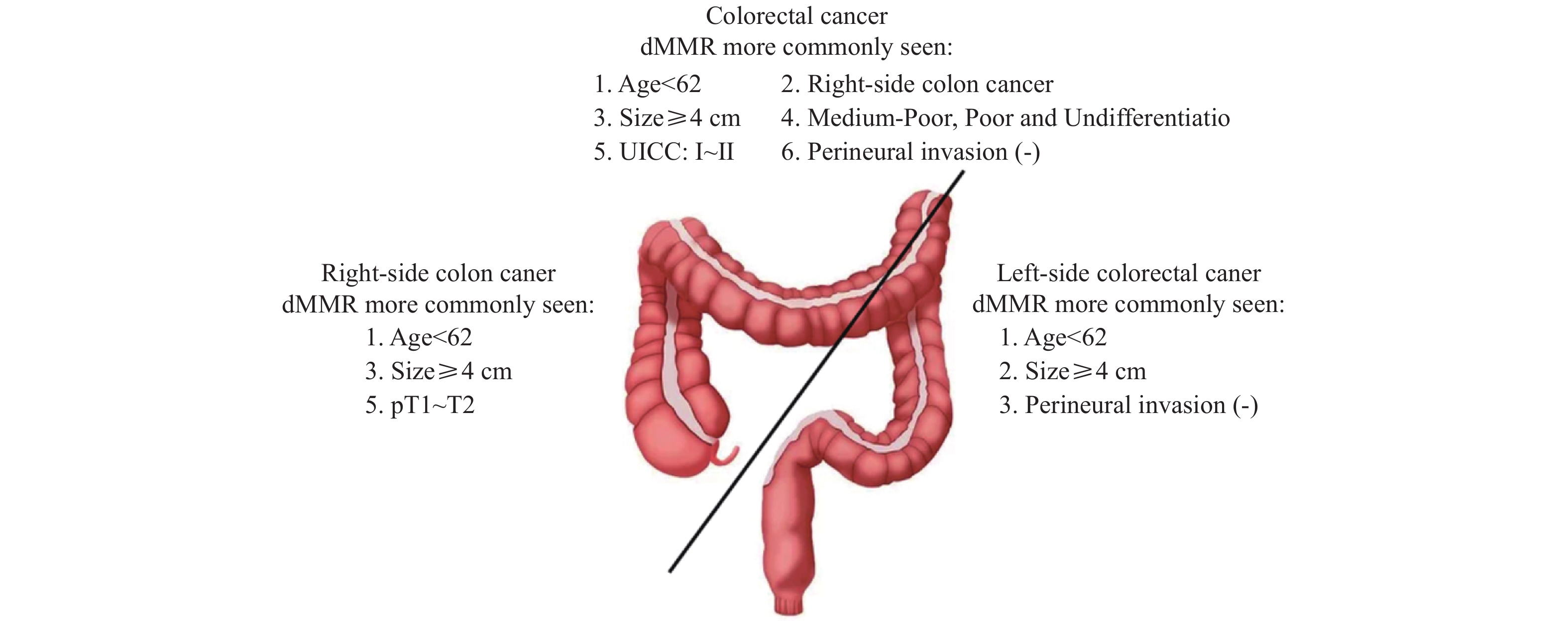
在本研究中,所有散发性肠癌患者dMMR更多见于年龄 < 62岁,右半肠癌、肿瘤直径≥4 cm、中低分化、低分化及未分化、UICC分期为Ⅰ~Ⅱ期、无神经侵犯者,这与既往报道基本一致[5, 19]。在散发性右半肠癌中,dMMR与年龄,pT以及肿瘤直径相关;在散发性左半肠癌中,dMMR与年龄,肿瘤直径以及无神经侵犯者相关,见图3。
在本研究中,1922例散发性肠癌的dMMR率为23.46%。国外dMMR率相对较低为8.4%[20],但高者可达34%[21],而国内的不同地区dMMR率(7.8%~17.9%)也不尽相同[13, 14, 22, 23]。上述结果提示,在不同人种以及不同地区的dMMR率存在差异,本研究的dMMR率相对较高可能与以下因素相关:(1)人种的不同导致错配修复蛋白的表达不尽相同;(2)地域环境的差异导致错配修复蛋白的表达存在差异;(3)虽然错配修复蛋白缺失的判断标准统一,但解释结果存在一定主观性,可能存在偏倚[24]。
在本研究的散发性右半肠癌中,右半肠癌的dMMR率为38.83%。通过多因素回归分析发现,在散发性右半肠癌中,dMMR多见于年龄 < 62岁,肿瘤直径≥4 cm者以及pT1~T2者。除了年龄及肿瘤直径这两个因素以外,本研究首次发现,在散发性右半肠癌中的pT1~T2者(P = 0.000,OR = 3.778)较高频率出现dMMR。与左半肠癌不同的是,散发性右半肠癌患者大体类型多为肿块型,局部浸润层次较浅,从本研究数据来看,散发性右半肠癌中T1~T2的患者共54例,其中dMMR者33例,占比61.11%相对较高,此外散发性右半肠癌多数由绒毛状腺瘤发展而来,这也提示对于腺瘤癌变者,其dMMR率相对较高。
在散发性左半肠癌中,左半肠癌dMMR率18.62%。本研究首次发现,在左半肠癌中,dMMR更多见于无神经侵犯者(OR = 1.454,P = 0.009)。在本研究中,散发性左半肠癌无神经侵犯者共891例,其中dMMR表型者181例,占比20.31%,对于本研究中首次发现的dMMR更多见于无神经侵犯者,需扩大样本进行验证,相关机制需后续试验进一步探讨。
综上所述,在散发性肠癌中,不论肿瘤部位如何,dMMR均与年龄 < 62岁,肿瘤直径≥4 cm存在相关关系;然而,本研究发现,散发性左、右半肠癌dMMR表型分别与神经侵犯(-)及pT1~T2分期相关。
本研究为单中心回顾性研究;由于潜在的局限性,不可避免的产生偏倚;缺少预后数据;本研究样本量较小,需更大样本量、多中心、前瞻性研究进一步佐证。
-
表 1 1922例散发性肠癌MMR表达与临床病理特征的关系[n(%)]
Table 1. Relationship between different MMR status and clinicopathological characteristics of all patients with sporadic colorectal cancer in the cohort [n(%)]
临床病理特征 MMR χ2 P pMMR(n = 1471) dMMR(n = 451) 性别 0.612 0.434 男 872(77.17) 258(22.83) 女 599(75.63) 193(24.37) 年龄(岁) 13.188 < 0.001* < 62 675(72.89) 251(27.11) ≥62 796(79.92) 200(20.08) BMI(kg/m2) 0.309 0.857 < 18.5 136(77.71) 39(22.29) 18.5~24 854(76.11) 268(23.89) ≥24 481(76.96) 144(23.04) 民族 0.174 0.677 汉族 1409(76.45) 434(23.55) 少数民族 62(78.48) 17(21.52) 血型 1.236 0.744 A+(Rh+) 507(76.70) 154(23.30) B+(Rh+) 381(74.85) 128(25.15) O+(Rh+) 453(77.44) 132(22.56) AB+(Rh+) 130(77.84) 37(22.16) CEA(ng/mL) 2.514 0.113 < 5 888(75.32) 291(24.68) ≥5 583(78.47) 160(21.53) 肿瘤部位 79.708 < 0.001* 右半肠癌 282(61.17) 179(38.83) 左半肠癌 1189(81.38) 272(18.62) 病理学类型 13.165 0.001* 普通腺癌 1331(77.75) 381(22.25) 粘液腺癌 35(63.64) 20(36.36) 混合腺癌 105(67.74) 50(32.26) 病理分化程度 26.828 < 0.001* 高 224(79.72) 57(20.28) 中高 471(79.03) 125(20.97) 未 33(62.26) 20(37.74) 中低 87(67.44) 42(32.56) 低 31(57.41) 23(42.59) 中 625(77.26) 184(22.74) 肿瘤直径(cm) 22.392 < 0.001* < 4 715(81.53) 162(18.47) ≥4 756(72.34) 289(27.66) pT 分期 4.538 0.209 T1 69(83.13) 14(16.87) T2 286(75.07) 95(24.93) T3 750(75.45) 244(24.55) T4 366(78.88) 98(21.12) pT 分期 0.000 0.988 T1~T2 355(76.51) 109(23.49) T3~T4 1116(76.54) 342(23.46) pN 分期 6.651 0.084 N0 853(74.56) 291(25.44) N1 409(78.65) 111(21.35) N2a 111(81.02) 26(18.98) N2b 98(80.99) 23(19.91) 清扫淋巴结数目 15.782 < 0.001* < 12 459(82.55) 97(17.45) ≥12 1012(74.08) 354(25.92) 远处转移 0.203 0.652 阴性 1388(76.64) 423(23.36) 阳性 83(74.77) 28(25.23) UICC 分期 7.366 0.061 Ⅰ 279(75.00) 93(25.00) Ⅱ 547(74.52) 187(25.48) Ⅲ 569(79.92) 143(20.08) Ⅳ 76(73.08) 28(26.92) UICC 分期 4.972 0.026* Ⅰ-Ⅱ 826(74.68) 280(25.32) Ⅲ-Ⅳ 645(79.04) 171(20.96) 脉管侵犯 2.417 0.120 阴性 1163(77.33) 341(22.67) 阳性 308(73.68) 110(26.32) 神经侵犯 6.090 0.014* 阴性 870(74.61) 296(23.59) 阳性 601(79.50) 155(20.50) *P < 0.05。 表 2 1922例散发性肠癌dMMR表型情况[n(%)]
Table 2. Different dMMR phenotype of all patients with sporadic colorectal cancer in the cohort [n(%)]
dMMR 总数 比率(%) 右半肠癌 左半肠癌 MLH1 46 2.39(46/1922) 10(0.52) 36(1.87) MSH2 18 0.94(18/1922) 5(0.26) 13(0.68) MSH6 14 0.73(14/1922) 4(0.21) 10(0.52) PMS2 146 7.60(146/1922) 49(2.55) 97(5.05) MLH1 + PMS2 131 6.82(131/1922) 71(3.69) 60(3.12) MSH2 + MSH6 23 1.20(23/1922) 15(0.78) 8(0.42) MLH1 + MSH2 + MSH6 + PMS2 11 0.57(11/1922) 3(0.16) 8(0.41) Other* 62 3.23(62/1922) 22(1.14) 40(2.08) Other*:MLH1 + MSH2(14例);MLH1 + MSH6(4例);MSH2 + PMS2(10例);MSH6 + PMS2(11例);MLH1 + MSH2 + MSH6(5例);MLH1 + MSH2+PMS2(10例);MLH1 + MSH6 + PMS2(4例);MSH2 + MSH6 + PMS2(4例)。 表 3 1922例散发性肠癌dMMR与临床病理特征的多因素分析
Table 3. Multivariate results of the relationship between dMMR status and clinicopathological features of all patients with sporadic colorectal cancer in the cohort
临床病理特征 dMMR OR 95% CI P 年龄(岁) < 62 1.551 1.243~1.936 < 0.001* ≥62 Reference 肿瘤部位 右半肠癌 2.603 2.044~3.314 < 0.001* 左半肠癌 Reference UICC 分期 I~II 1.340 1.062~1.691 0.014* III~IV Reference 病理分化程度 高 0.818 0.578~1.157 0.256 中高 0.884 0.677~1.153 0.363 未 1.850 1.013~3.377 0.045* 中低 1.538 1.008~2.346 0.046* 低 2.124 1.169~3.861 0.013* 中 Reference 肿瘤直径(cm) ≥4 1.362 1.079~1.719 0.009* < 4 Reference 神经侵犯 阴性 1.407 1.112~1.787 0.004* 阳性 Reference *P < 0.05。 表 4 461例散发性右半肠癌MMR与临床病理特征的关系[n(%)]
Table 4. Relationship between different MMR status and clinicopathological characteristics of the 461 patients with right-side colon cancer in the cohort [n(%)]
临床病理特征 MMR χ2 P pMMR dMMR 性别 282 179 0.244 0.621 男 161(62.16) 98(37.84) 女 121(59.90) 81(40.10) 年龄(岁) < 62 112(53.85) 96(46.15) 8.562 0.003* ≥62 170(67.19) 83(32.81) BMI(kg/m2) < 18.5 29(61.70) 18(38.30) 0.125 0.940 18.5~24 180(61.64) 112(38.36) ≥24 73(59.83) 49(40.17) 民族 汉族 271(60.90) 174(39.10) 0.401 0.527 少数民族 11(68.75) 5(31.25) 血型 A+(Rh+) 104(63.80) 59(36.20) 1.800 0.615 B+(Rh+) 74(60.16) 49(39.84) O+(Rh+) 83(61.48) 52(38.52) AB+(Rh+) 21(52.50) 19(47.50) CEA(ng/mL) < 5 153(57.74) 112(42.26) 3.097 0.078 ≥5 129(65.82) 67(34.18) 病理学类型 普通腺癌 242(63.02) 142(36.98) 4.509 0.105 粘液腺癌 5(38.46) 8(61.54) 混合腺癌 35(54.69) 29(45.31) 病理分化程度 高 37(61.67) 23(38.33) 8.505 0.130 中高 93(64.58) 51(35.42) 未 5(38.46) 8(61.54) 中低 22(51.16) 21(48.84) 低 11(45.83) 13(54.17) 中 114(64.41) 63(35.59) 肿瘤直径(cm) < 4 79(67.52) 38(32.48) 2.662 0.103 ≥4 203(59.01) 141(40.99) pT 分期 T1 8(61.54) 5(38.46) 21.877 < 0.001* T2 13(31.71) 28(68.29) T3 165(60.22) 109(39.78) T4 96(72.18) 37(27.82) pT 分期 T1~T2 21(38.89) 33(61.11) 12.786 < 0.001* T3~T4 261(64.13) 146(35.87) pN 分期 N0 162(57.45) 120(42.55) 6.438 0.092 N1 79(64.75) 43(35.25) N2a 18(64.29) 10(35.71) N2b 23(79.31) 6(20.69) 清扫淋巴结数目 < 12 28(63.64) 16(36.36) 0.124 0.724 ≥12 254(60.91) 163(39.09) 远处转移 阴性 265(61.34) 167(38.66) 0.085 0.771 阳性 17(58.62) 12(41.38) UICC 分期 Ⅰ 17(36.96) 29(63.04) 13.943 0.003* Ⅱ 140(62.50) 84(37.50) Ⅲ 109(66.87) 54(33.13) Ⅳ 16(57.14) 12(42.86) UICC 分期 Ⅰ-Ⅱ 157(58.15) 113(41.85) 2.508 0.113 Ⅲ-Ⅳ 125(65.45) 66(34.55) 脉管侵犯 阴性 209(61.65) 130(38.35) 0.125 0.724 阳性 73(59.84) 49(40.16) 神经侵犯 阴性 160(58.19) 115(41.81) 2.565 0.109 阳性 122(65.59) 64(34.41) *P < 0.05。 表 5 461例散发性右半肠癌dMMR与临床病理特征的多因素分析
Table 5. Multivariate results of the relationship between dMMR status and clinicopathological features of the 461 patients with right-side colon cancer
临床病理特征 dMMR OR 95% CI P 年龄(岁) < 62 1.888 1.276~2.793 0.001* ≥62 Reference pT 分期 T1~T2 3.778 2.020~7.064 < 0.001* T3~T4 Reference 肿瘤直径(cm) ≥4 1.856 1.144~3.009 0.012* < 4 Reference *P < 0.05。 表 6 1461例散发性左半肠癌MMR与临床病理特征的关系 [n(%)]
Table 6. Relationship between different MMR status and clinicopathological characteristics of the 1461 patients with left-side colon cancers in the cohort [n(%)]
临床病理特征 MMR χ2 P pMMR dMMR 性别 1189 272 0.087 0.768 男 711(81.63) 160(18.37) 女 478(81.02) 112(18.98) 年龄(岁) < 62 563(78.41) 155(21.59) 8.222 0.004* ≥62 626(84.25) 117(15.75) BMI(kg/m2) < 18.5 107(83.59) 21(16.41) 0.454 0.797 18.5~24 674(81.20) 156(18.80) ≥24 408(81.11) 95(18.89) 民族 汉族 1138(81.40) 260(18.60) 0.008 0.929 少数民族 51(80.95) 12(19.05) 血型 A+(Rh+) 403(80.92) 95(19.08) 2.805 0.423 B+(Rh+) 307(79.53) 79(20.47) O+(Rh+) 370(82.22) 80(17.78) AB+(Rh+) 109(85.83) 18(14.17) CEA(ng/mL) < 5 735(80.42) 179(19.58) 1.506 0.220 ≥5 454(83.00) 93(17.00) 病理学类型 普通腺癌 1089(82.00) 239(18.00) 4.278 0.118 粘液腺癌 30(71.43) 12(28.57) 混合腺癌 70(76.92) 21(23.08) 病理分化程度 高 187(84.62) 34(15.38) 12.764 0.026* 中高 378(83.63) 74(16.37) 未 28(70.00) 12(30.00) 中低 65(75.58) 21(24.42) 低 20(66.67) 10(33.33) 中 511(80.85) 121(19.15) 肿瘤直径(cm) < 4 636(83.68) 124(16.32) 5.538 0.019* ≥4 553(78.89) 148(21.11) pT 分期 T1 61(87.14) 9(12.86) 1.815 0.612 T2 273(80.29) 67(19.71) T3 585(81.25) 135(18.75) T4 270(81.57) 61(18.43) pT 分期 T1~T2 334(81.46) 76(18.54) 0.002 0.960 T3~T4 855(81.35) 196(18.65) pN 分期 N0 691(80.16) 171(19.84) 2.581 0.461 N1 330(82.91) 68(17.09) N2a 93(85.32) 16(14.68) N2b 75(81.52) 17(18.48) 清扫淋巴结数目 < 12 431(84.18) 81(15.82) 4.070 0.044* ≥12 758(79.87) 191(20.13) 远处转移 阴性 1123(81.44) 256(18.56) 0.046 0.830 阳性 66(80.49) 16(19.51) UICC 分期 Ⅰ 262(80.37) 64(19.63) 3.456 0.327 Ⅱ 407(79.80) 103(20.20) Ⅲ 460(83.79) 89(16.21) Ⅳ 60(78.95) 16(21.05) UICC 分期 Ⅰ-Ⅱ 669(80.02) 167(19.98) 2.381 0.123 Ⅲ-Ⅳ 520(83.20) 105(16.80) 脉管侵犯 阴性 954(81.89) 211(18.11) 0.971 0.324 阳性 235(79.39) 61(20.61) 神经侵犯 阴性 710(79.69) 181(20.31) 4.340 0.037* 阳性 479(84.04) 91(15.96) *P < 0.05。 表 7 1461例散发性左半肠癌dMMR与临床病理特征的多因素分析
Table 7. Multivariate results of the relationship between dMMR status and clinicopathological features of the 1461 patients with left-side colon cancer
临床病理特征 dMMR OR 95% CI P 年龄(岁) < 62 1.525 1.166~1.995 0.002* ≥62 Reference 肿瘤直径(cm) ≥4 1.391 1.064~1.819 0.016* < 4 Reference 神经侵犯 阴性 1.454 1.096~1.928 0.009* 阳性 Reference *P < 0.05。 -
[1] Siegel R L,Miller K D,Jemal A. Cancer statistics,2020[J]. CA:A Cancer Journal For Clinicians,2020,70(1):7-30. doi: 10.3322/caac.21590 [2] Nguyen L H,Goel A,Chung D C. Pathways of colorectal carcinogenesis[J]. Gastroenterology,2020,158(2):291-302. doi: 10.1053/j.gastro.2019.08.059 [3] Harada S,Morlote D. Molecular pathology of colorectal cancer[J]. Advances In Anatomic Pathology,2020,27(1):20-6. doi: 10.1097/PAP.0000000000000247 [4] Deng Z,Qin Y,Wang J,et al. Prognostic and predictive role of DNA mismatch repair status in stage II-III colorectal cancer:A systematic review and meta-analysis[J]. Clinical Genetics,2020,97(1):25-38. doi: 10.1111/cge.13628 [5] Chikatani K,Chika N,Suzuki O,et al. A model for predicting DNA mismatch repair-deficient colorectal cancer[J]. Anticancer Research,2020,40(8):4379-4385. doi: 10.21873/anticanres.14441 [6] Sargent D J,Marsoni S,Monges G,et al. Defective mismatch repair as a predictive marker for lack of efficacy of fluorouracil-based adjuvant therapy in colon cancer[J]. Journal Of Clinical Oncology:Official Journal Of The American Society Of Clinical Oncology,2010,28(20):3219-3226. doi: 10.1200/JCO.2009.27.1825 [7] Popat S,Hubner R,Houlston R S. Systematic review of microsatellite instability and colorectal cancer prognosis[J]. Journal Of Clinical Oncology:Official Journal Of The American Society Of Clinical Oncology,2005,23(3):609-618. doi: 10.1200/JCO.2005.01.086 [8] Zhu L,Huang Y,Fang X,et al. A novel and reliable method to detect microsatellite instability in colorectal cancer by next-generation sequencing[J]. The Journal Of Molecular Diagnostics:JMD,2018,20(2):225-231. doi: 10.1016/j.jmoldx.2017.11.007 [9] Cheah P L,Li J,Looi L M,et al. Screening for microsatellite instability in colorectal carcinoma:Practical utility of immunohistochemistry and PCR with fragment analysis in a diagnostic histopathology setting[J]. The Malaysian Journal Of Pathology,2019,41(2):91-100. [10] 张园园,邹霜梅,王振宁,等. 26280例结直肠癌患者MLH1和PMS2基因表达情况及临床病理特征的多中心回顾性研究[J]. 中华结直肠疾病电子杂志,2019,8(1):16-22. doi: 10.3877/cma.j.issn.2095-3224.2019.01.004 [11] Yoon Y S,Yu C S,Kim T W,et al. Mismatch repair status in sporadic colorectal cancer:immunohistochemistry and microsatellite instability analyses[J]. J Gastroenterol Hepato,2011,26(12):1733-1739. doi: 10.1111/j.1440-1746.2011.06784.x [12] 王超,高志冬,姜可伟,等. 结肠癌组织中错配修复蛋白表达及其对患者预后的影响[J]. 中华普通外科杂志,2019,34(4):349-352. doi: 10.3760/cma.j.issn.1007-631X.2019.04.017 [13] 吴畅,张继君,赵夫娟,等. 湖南地区结直肠癌中错配修复蛋白MSH2、MSH6、MLH1及PMS2的表达与临床病理特征的关系[J]. 中国医学创新,2019,16(13):112-115. doi: 10.3969/j.issn.1674-4985.2019.13.028 [14] Cao Y,Peng T,Li H,et al. Development and validation of MMR prediction model based on simplified clinicopathological features and serum tumour markers[J]. E Bio Medicine,2020,61:103060. doi: 10.1016/j.ebiom.2020.103060 [15] 袁瑛. 结直肠癌及其他相关实体瘤微卫星不稳定性检测中国专家共识[J]. 实用肿瘤杂志,2019,34(5):381-389. [16] 吴焕文,邵建永. 结直肠癌分子生物标志物检测专家共识[J]. 中华病理学杂志,2018,47(4):237-240. [17] Guo T A,Wu Y C,Tan C,et al. Clinicopathologic features and prognostic value of KRAS,NRAS and BRAF mutations and DNA mismatch repair status:A single-center retrospective study of 1,834 Chinese patients with Stage I-IV colorectal cancer[J]. International Journal Of Cancer,2019,145(6):1625-1634. doi: 10.1002/ijc.32489 [18] Bufill J A. Colorectal cancer:evidence for distinct genetic categories based on proximal or distal tumor location[J]. Annals Of Internal Medicine,1990,113(10):779-788. doi: 10.7326/0003-4819-113-10-779 [19] X Z T,Z R X,Z Y,et al. Relationship between the expression of mismatch repair protein and clinicopathological characteristics in patients with sporadic colorectal cancer[J]. Chinese Medical Journal,2017,97(16):1248-1251. [20] Suzuki O,Eguchi H,Chika N,et al. Prevalence and clinicopathologic/molecular characteristics of mismatch repair-deficient colorectal cancer in the under-50-year-old Japanese population[J]. Surg Today,2017,47(9):1135-1146. doi: 10.1007/s00595-017-1486-x [21] Hashmi A A,Ali R,Hussain Z F,et al. Mismatch repair deficiency screening in colorectal carcinoma by a four-antibody immunohistochemical panel in Pakistani population and its correlation with histopathological parameters[J]. World J Surg Oncol,2017,15(1):116. doi: 10.1186/s12957-017-1158-8 [22] 谢仲鹏,李海荣,吴余,等. 海南地区结直肠癌中错配修复蛋白及多药耐药蛋白的表达及意义[J]. 临床与实验病理学杂志,2020,36(10):1205-1208. [23] 朱凤伟,吕亚莉,宋欣,等. 左右半结肠癌分子生物学表达与临床病理特征关系[J]. 诊断病理学杂志,2020,27(3):145-149+53. doi: 10.3969/j.issn.1007-8096.2020.03.001 [24] 姜武,凌逸虹,吴晓丹,等. 结直肠癌错配修复蛋白免疫组化结果误判与对策[J]. 中国全科医学,2019,22(24):2967-2970. doi: 10.12114/j.issn.1007-9572.2019.00.105 期刊类型引用(1)
1. 李东松,陈娉珊,蔡泰楠,蔡泽华,丁玉芝,童昊. 错配修复蛋白表达缺失与结直肠癌病理特征及预后的关系. 医学信息. 2024(08): 99-103 .  百度学术
百度学术其他类型引用(1)
-






 下载:
下载:
 下载:
下载:

