Novel Conservative Treatment Mechanisms and Clinical Translation for Female Stress Urinary Incontinence
-
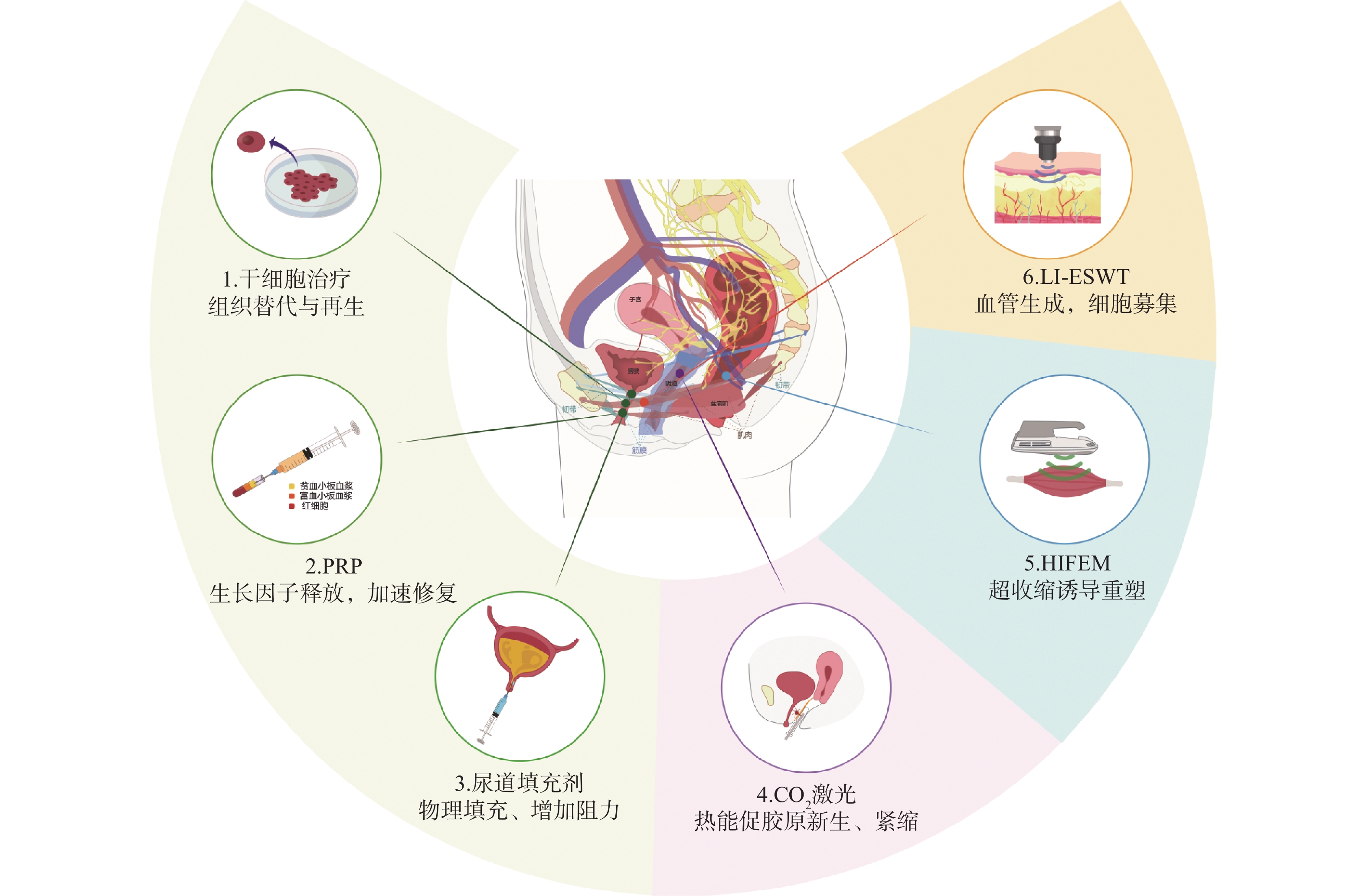
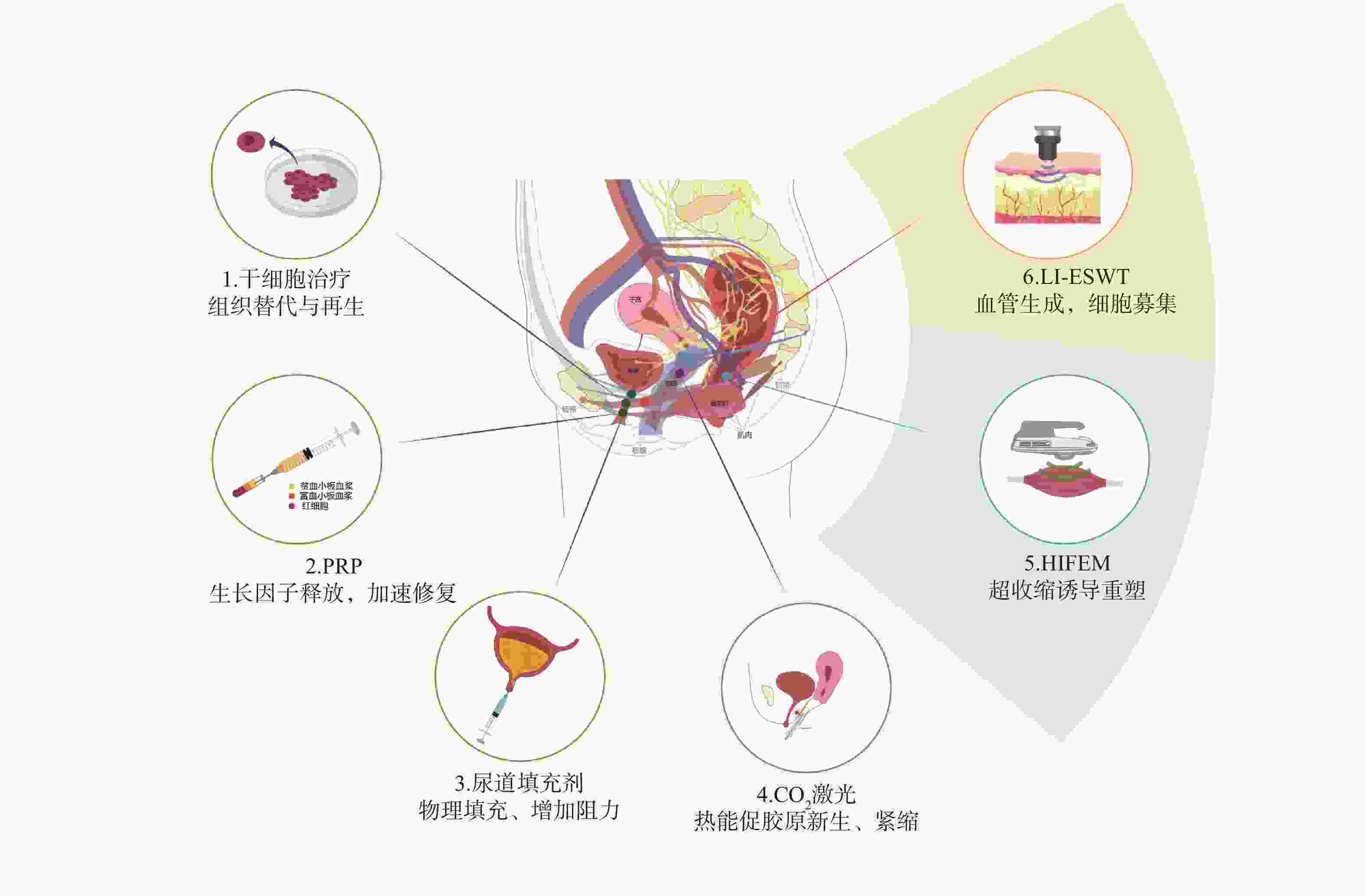
摘要: 压力性尿失禁(stress urinary incontinence,SUI)是影响全球数百万女性的最常见盆底功能障碍之一。目前,临床实践中广泛采用的保守治疗方法疗效相对有限,亟需探索超越传统方法的创新治疗方案。近年来,物理治疗技术(如高强度聚焦电磁刺激)、再生医学与生物材料以及远程康复模式等新型保守治疗手段逐渐崭露头角,成为治疗SUI的潜在干预手段。这些疗法可能有效改善尿失禁症状并提升患者生活质量。对上述几种疗法在SUI中的作用机制及临床转化进展进行了综述,旨在为SUI的临床实践提供创新且实用的参考方案。Abstract: Stress urinary incontinence is one of the most common pelvic floor dysfunctions affecting millions of women worldwide. Currently, conservative treatment methods widely adopted in clinical practice have relatively limited efficacy, necessitating the exploration of innovative treatment approaches beyond traditional methods. In recent years, new treatment methods such as physical therapy techniques (e.g., high-intensity focused electromagnetic stimulation), regenerative medicine and biomaterials, and telerehabilitation models have gradually become prominent as potential interventions for SUI. These therapies may effectively alleviate urinary incontinence symptoms and improve the quality of life for patients. This review discusses the mechanisms of action and clinical translation progress of several aforementioned therapies in SUI, aiming to provide innovative and practical reference solutions for clinical practice in SUI management.
-
表 1 SUI新型保守治疗的疗效与特性对比
Table 1. Comparison of efficacy and characteristics of new conservative treatment for SUI
治疗方式 主要作用机制 疗程 疗效维持
(月)优势 局限 参考文献 HIFEM 非侵入性诱发深层肌肉收缩,增强肌力与耐力 8~12次/4~6周 约6~18 无创、操作简单,尤其适用盆底肌力弱者 无法直接改善结缔组织松弛,对重度患者效果有限 [10,12−14] CO2激光 促进新胶原纤维的形成 3~5次/3~4月 约12-~24 微创、安全,
对与尿道及阴道结缔组织松弛患者疗效较好不能直接改善肌肉力量,对重度盆底组织脱垂/萎缩者效果欠佳 [16−20] Li-ESWT 促进血管生成和肌肉
再生6次/8周 约12~24 无创、副作用小,促进整体修复,协同改善多个机制 个体差异大,需多次治疗,长期效果待观察 [25−26] 干细胞注射 促进组织修复和再生 单次(可重复) * 再生潜力大,综合修复组织 临床数据有限,安全性需进一步验证 [30−32] PRP 促进组织再生、增强胶原蛋白生成、减轻炎症 2次注射,间隔4~6周 约3~6 取材自体,微创,安全性高 作用时间有限,需多次注射 [35−38] 尿道填充剂 提升尿道体积,增加闭合压力 单次,中位手术时间为9min 约24~36 即刻改善症状,操作简便,微创,耗时短 需重复注射,存在诸如尿路感染和尿潴留等多种并发症 [41−43] mHealth APP+PFMT 实时监测患者训练情况,可视化反馈 长期坚持训练 依赖训练持续性 无创,经济,可及性高 需患者主动参与 [48−49] *目前临床研究随访时间有限,远期疗效尚待观察。 -
[1] Jefferson F A, Linder B J. Evaluation and management of female stress urinary incontinence[J]. Mayo Clin Proc, 2024, 99(11): 1802-1814. doi: 10.1016/j.mayocp.2024.07.003 [2] Li L, Li G, Dai S, et al. Prevalence and spatial distribution characteristics of female stress urinary incontinence in mainland China[J]. Eur Urol Open Sci, 2024, 68: 48-60. doi: 10.1016/j.euros.2024.08.007 [3] Alexandridis V, Lundmark Drca A, Ek M, et al. Retropubic slings are more efficient than transobturator at 10-year follow-up: A Swedish register-based study[J]. Int Urogynecol J, 2023, 34(6): 1307-1315. doi: 10.1007/s00192-023-05506-4 [4] Lin Y H, Lee C K, Chang S D, et al. Focusing on long-term complications of mid-urethral slings among women with stress urinary incontinence as a patient safety improvement measure: A protocol for systematic review and meta-analysis[J]. Medicine, 2021, 100(24): e26257. doi: 10.1097/MD.0000000000026257 [5] Li M, Qiu K, Guo H, et al. Conservative treatments for women with stress urinary incontinence: A systematic review and network meta-analysis[J]. Front Med, 2024, 11: 1517962. doi: 10.3389/fmed.2024.1517962 [6] Yang X, Wang X, Gao Z, et al. The anatomical pathogenesis of stress urinary incontinence in women[J]. Medicina, 2022, 59(1): 5. doi: 10.3390/medicina59010005 [7] Zachariah R R, Lange S, Keller N, et al. Female urinary incontinence - diagnostics and therapies[J]. Praxis, 2024, 113(10): 261-266. [8] Moawad G N, Wu C, Klebanoff J S, et al. Pelvic neuroanatomy: An overview of commonly encountered pelvic nerves in gynecologic surgery[J]. J Minim Invasive Gynecol, 2021, 28(2): 178. doi: 10.1016/j.jmig.2020.06.005 [9] Leonardo K, Rahardjo H E, Afriansyah A. Noninvasive high-intensity focused electromagnetic therapy in women with urinary incontinence: A systematic review and meta-analysis[J]. Neurourol Urodyn, 2025, 44(2): 424-433. doi: 10.1002/nau.25658 [10] Samuels J B, Pezzella A, Berenholz J, et al. Safety and efficacy of a non-invasive high-intensity focused electromagnetic field (HIFEM) device for treatment of urinary incontinence and enhancement of quality of life[J]. Lasers Surg Med, 2019, 51(9): 760-766. doi: 10.1002/lsm.23106 [11] Pavčnik M, Antić A, Lukanović A, et al. Evaluation of possible side effects in the treatment of urinary incontinence with magnetic stimulation[J]. Medicina, 2023, 59(7): 1286. doi: 10.3390/medicina59071286 [12] Tosun H, Akınsal E C, Sönmez G, et al. Is the high-intensity focused electromagnetic energy an effective treatment for urinary incontinence in women?[J]. Ther Clin Risk Manag, 2024, 20: 811-816. doi: 10.2147/TCRM.S478919 [13] Long C Y, Lin K L, Yeh J L, et al. Effect of high-intensity focused electromagnetic technology in the treatment of female stress urinary incontinence[J]. Biomedicines, 2024, 12(12): 2883. doi: 10.3390/biomedicines12122883 [14] Silantyeva E, Zarkovic D, Astafeva E, et al. A comparative study on the effects of high-intensity focused electromagnetic technology and electrostimulation for the treatment of pelvic floor muscles and urinary incontinence in parous women: Analysis of posttreatment data[J]. Female Pelvic Med Reconstr Surg, 2021, 27(4): 269-273. doi: 10.1097/SPV.0000000000000807 [15] Li P C, Ding D C. Exploring the role of laser therapy for stress urinary incontinence: A literature review[J]. Lasers Med Sci, 2025, 40(1): 125. doi: 10.1007/s10103-025-04385-z [16] Alcalay M, Ben Ami M, Greenshpun A, et al. Fractional-pixel CO2 laser treatment in patients with urodynamic stress urinary incontinence: 1-year follow-up[J]. Lasers Surg Med, 2021, 53(7): 960-967. doi: 10.1002/lsm.23329 [17] Kuszka A, Gamper M, Walser C, et al. Erbium: YAG laser treatment of female stress urinary incontinence: Midterm data[J]. Int Urogynecol J, 2020, 31(9): 1859-1866. doi: 10.1007/s00192-019-04148-9 [18] Gao L, Wang Y, Wen W, et al. Fractional carbon dioxide vaginal laser treatment of stress urinary incontinence: Remodeling of vaginal tissues and improving pelvic floor structures[J]. Lasers Surg Med, 2023, 55(3): 268-277. doi: 10.1002/lsm.23641 [19] Ruffolo A F, Braga A, Torella M, et al. Vaginal laser therapy for female stress urinary incontinence: New solutions for a well-known issue-a concise review[J]. Medicina, 2022, 58(4): 512. doi: 10.3390/medicina58040512 [20] Rocha-Rangel S C, Pereira G M V, Juliato C R T, et al. Laser and pelvic floor muscle training for urinary incontinence: A randomized clinical trial[J]. Urogynecology, 2025, 31(6): 627-635. doi: 10.1097/SPV.0000000000001516 [21] De Marchi T, Ferlito J V, Turra A C, et al. Pilates method and/or photobiomodulation therapy combined to static magnetic field in women with stress urinary incontinence: A randomized, double-blind, placebo-controlled clinical trial[J]. J Clin Med, 2023, 12(3): 1104. doi: 10.3390/jcm12031104 [22] Lin G, Lue T F. Microenergy shockwave therapies for female stress urinary incontinence[J]. Transl Androl Urol, 2024, 13(8): 1687-1694. doi: 10.21037/tau-23-9 [23] Chen P Y, Cheng J H, Wu Z S, et al. New frontiers of extracorporeal shock wave medicine in urology from bench to clinical studies[J]. Biomedicines, 2022, 10(3): 675. doi: 10.3390/biomedicines10030675 [24] Zhang X, Ruan Y, Wu A K, et al. Delayed treatment with low-intensity extracorporeal shock wave therapy in an irreversible rat model of stress urinary incontinence[J]. Urology, 2020, 141: 187. e1-187. e7. [25] Lin K L, Chueh K S, Lu J H, et al. Low intensity extracorporeal shock wave therapy as a novel treatment for stress urinary incontinence: A randomized-controlled clinical study[J]. Medicina, 2021, 57(9): 947. doi: 10.3390/medicina57090947 [26] Long C Y, Lin K L, Lee Y C, et al. Therapeutic effects of Low intensity extracorporeal low energy shock wave therapy (LiESWT) on stress urinary incontinence[J]. Sci Rep, 2020, 10(1): 5818. doi: 10.1038/s41598-020-62471-4 [27] Li P C, Ding D C. Stem-cell therapy in stress urinary incontinence: A review[J]. Tzu Chi Med J, 2022, 35(2): 111-119. [28] Andersson K E, Williams K. Cellular regenerative therapy in stress urinary incontinence: New frontiers? -a narrative review[J]. Transl Androl Urol, 2024, 13(8): 1709-1716. doi: 10.21037/tau-22-682 [29] Seval M M, Koyuncu K. Current status of stem cell treatments and innovative approaches for stress urinary incontinence[J]. Front Med, 2022, 9: 1073758. doi: 10.3389/fmed.2022.1073758 [30] Blaganje M, Lukanović A. The effect of skeletal muscle-derived cells implantation on stress urinary incontinence and functional urethral properties in female patients[J]. Int J Gynaecol Obstet, 2022, 157(2): 444-451. doi: 10.1002/ijgo.13853 [31] Rose A, Rübben H. Implantation of autologous skeletal muscle-derived cells combined with electrical stimulation in patients with stress urinary incontinence[J]. Int Urogynecol J, 2025, 36(3): 703-713. doi: 10.1007/s00192-025-06079-0 [32] Mariotti G, Salciccia S, Viscuso P, et al. Regenerative medicine-based treatment of stress urinary incontinence with mesenchymal stem cells: A systematic review and meta-analysis[J]. Curr Stem Cell Res Ther, 2023, 18(3): 429-437. doi: 10.2174/1574888X17666220616100621 [33] Pourebrahimi A, Khalili A, Behzadi S, et al. Platelet-rich plasma for treatment of female stress urinary incontinence[J]. Int Urol Nephrol, 2025, 57(2): 313-321. [34] Lee P J, Jiang Y H, Kuo H C. A novel management for postprostatectomy urinary incontinence: Platelet-rich plasma urethral sphincter injection[J]. Sci Rep, 2021, 11(1): 5371. doi: 10.1038/s41598-021-84923-1 [35] Chiang C H, Kuo H C. The efficacy and mid-term durability of urethral sphincter injections of platelet-rich plasma in treatment of female stress urinary incontinence[J]. Front Pharmacol, 2022, 13: 847520. doi: 10.3389/fphar.2022.847520 [36] Grigoriadis T, Kalantzis C, Zacharakis D, et al. Platelet-rich plasma for the treatment of stress urinary incontinence-a randomized trial[J]. Urogynecology, 2024, 30(1): 42-49. doi: 10.1097/SPV.0000000000001378 [37] Saraluck A, Chinthakanan O, Kijmanawat A, et al. Autologous platelet rich plasma (A-PRP) combined with pelvic floor muscle training for the treatment of female stress urinary incontinence (SUI): A randomized control clinical trial[J]. Neurourol Urodyn, 2024, 43(2): 342-353. doi: 10.1002/nau.25365 [38] Behnia-Willison F, Nguyen T T T, Norbury A J, et al. Promising impact of platelet rich plasma and carbon dioxide laser for stress urinary incontinence[J]. Eur J Obstet Gynecol Reprod Biol X, 2019, 5: 100099. [39] Fleischmann N, Chughtai B, Plair A, et al. Urethral bulking[J]. Urogynecology, 2024, 30(8): 667-682. doi: 10.1097/SPV.0000000000001548 [40] Hoe V, Haller B, Yao H H, et al. Urethral bulking agents for the treatment of stress urinary incontinence in women: A systematic review[J]. Neurourol Urodyn, 2021, 40(6): 1349-1388. doi: 10.1002/nau.24696 [41] Pai A, Al-Singary W. Durability, safety and efficacy of polyacrylamide hydrogel (Bulkamid(®)) in the management of stress and mixed urinary incontinence: Three year follow up outcomes[J]. Cent European J Urol, 2015, 68(4): 428-433. [42] Serati M, Giammò A, Carone R, et al. Bulking agents for the treatment of recurrent stress urinary incontinence: A suitable option?[J]. Minerva Urol Nephrol, 2022, 74(6): 747-754. [43] Sikora M, Gamper M, Zivanovic I, et al. Current treatment of stress urinary incontinence by bulking agents and laser therapy-an update[J]. J Clin Med, 2024, 13(5): 1377. doi: 10.3390/jcm13051377 [44] Mantilla Toloza S C, Villareal Cogollo A F, Peña García K M. Pelvic floor training to prevent stress urinary incontinence: A systematic review[J]. Actas Urol Esp, 2024, 48(4): 319-327. doi: 10.1016/j.acuro.2024.01.007 [45] Todhunter-Brown A, Hazelton C, Campbell P, et al. Conservative interventions for treating urinary incontinence in women: An overview of cochrane systematic reviews[J]. Cochrane Database Syst Rev, 2022, 9(9): CD012337. [46] Smith S M, Wallace E, Clyne B, et al. Interventions for improving outcomes in patients with multimorbidity in primary care and community setting: A systematic review[J]. Syst Rev, 2021, 10(1): 271. doi: 10.1186/s13643-021-01817-z [47] Hou Y, Feng S, Tong B, et al. Effect of pelvic floor muscle training using mobile health applications for stress urinary incontinence in women: A systematic review[J]. BMC Womens Health, 2022, 22(1): 400. doi: 10.1186/s12905-022-01985-7 [48] Hao J, Yao Z, Remis A, et al. Pelvic floor muscle training in telerehabilitation: A systematic review and meta-analysis[J]. Arch Gynecol Obstet, 2024, 309(5): 1753-1764. doi: 10.1007/s00404-024-07380-x [49] Hamine S, Gerth-Guyette E, Faulx D, et al. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: A systematic review[J]. J Med Internet Res, 2015, 17(2): e52. doi: 10.2196/jmir.3951 -





 下载:
下载: