Analysis of Clinical Characteristics and Death Risk Factors in Patients with Community-acquired Pneumonia Complicated with Diabetes
-
摘要:
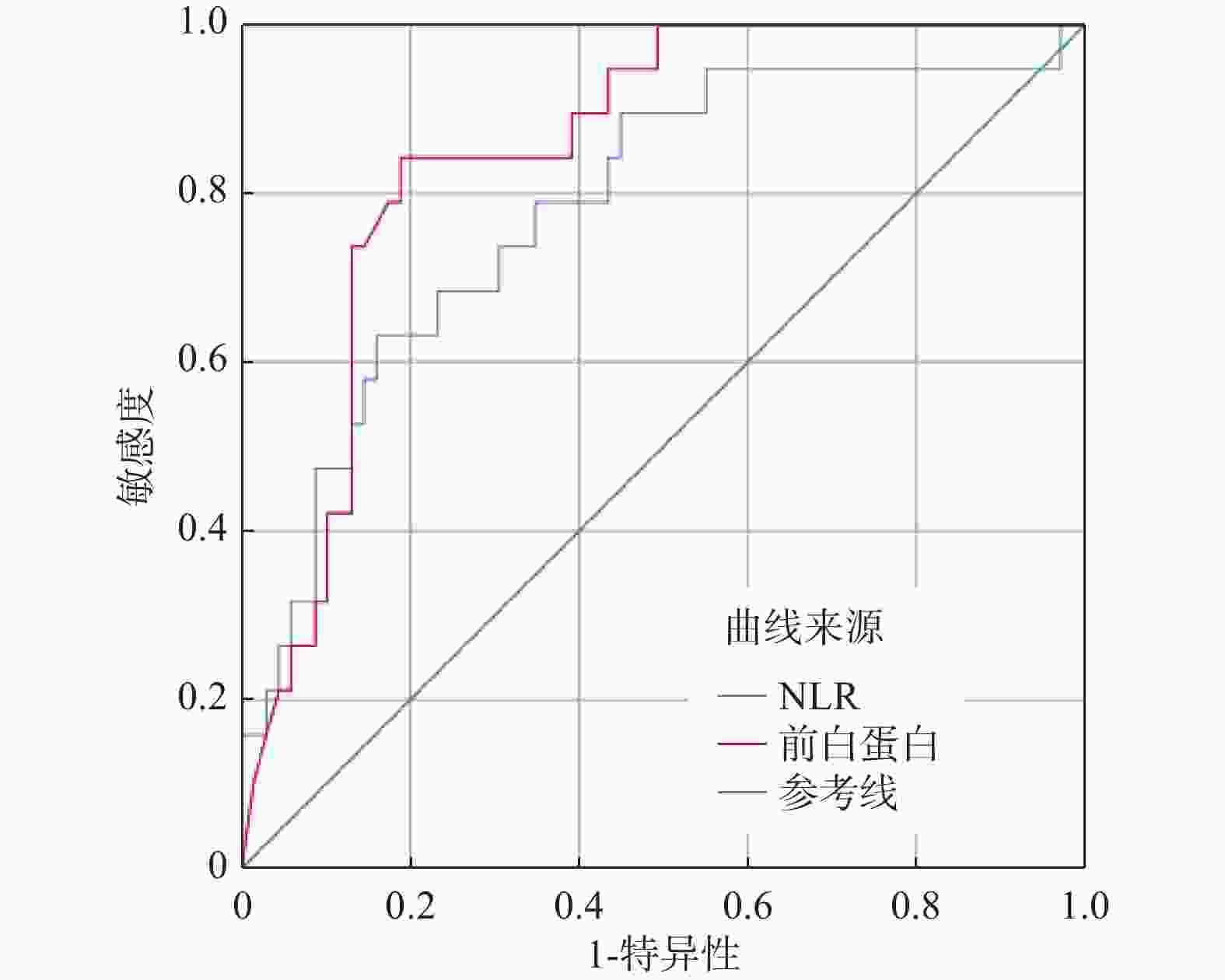
目的 探讨社区获得性肺炎(community-acquired pneumonia,CAP)合并糖尿病(diabetes mellitus,DM)患者的临床特征和住院期间死亡的危险因素。 方法 回顾性收集昆明医科大学第二附属医院2018年1月至2022年1月住院治疗的566例CAP患者资料,根据患者是否合并糖尿病分为单纯CAP组(n=478),CAP合并糖尿病(CAP+DM)组(n=88),再根据患者住院期间是否死亡将CAP+DM组(n=88)分为存活组(n=69)和死亡组(n=19)。分别比较不同分组患者的临床资料和入院时的实验室化验指标,采用Cox回归分析筛选CAP+DM组患者住院期间死亡的危险因素,绘制受试者工作特征(receiver operating characteristic,ROC)曲线评估危险因素对住院期间死亡的预测价值。 结果 与单纯CAP组比较,CAP+DM组患者在年龄、合并高血压、冠心病、CURB-65评分、中性粒细胞与淋巴细胞比值(neutrophil to lymphocyte ratio,NLR)、C反应蛋白(C-reactive protein,CRP)、降钙素原(procalcitonin,PCT)、白蛋白(albumin,ALB)、前白蛋白(prealbumin,PA)、葡萄糖(glucose,GLU)、血清钾(potassium,K)、钙(calcium,Ca)、磷(phosphorus,P)、镁(magnesium,Mg)、乳酸(lactic acid,Lac),无创通气时间、入住ICU率及病死率比较上,差异有统计学意义(P < 0.05);与存活组比较,死亡组患者在CURB-65评分、NLR、CRP、PCT、GIU、ALB、PA、血清铁(iron,Fe)、Ca、无创通气时间、入住ICU率比较上,差异有统计学意义(P < 0.05)。Cox回归分析显示,NLR水平升高、PA水平下降是CAP合并糖尿病患者住院期间死亡的危险因素(P < 0.05)。PA截断值为91 mg/L时,预测合并糖尿病的CAP患者住院期间死亡的曲线下面积(area under curve,AUC)、灵敏度和特异度分别为0.849,84.2%、81.2%。 结论 CAP合并糖尿病的患者较单纯的CAP患者病情更严重,预后更差,PA对这类患者的预后具有良好的预测价值,应早期检测并积极干预,以降低患者的住院病死率。 Abstract:Objective To explore the clinical characteristics and risk factors of death during hospitalization in patients with community-acquired pneumonia(CAP) complicated with diabetes mellitus(DM). Methods A retrospective analysis was performed on 566 patients with CAP hospitalized in the Second Affiliated Hospital of Kunming Medical University from January 2018 to January 2022. The patients were divided into simple CAP group(n=478) and CAP combined with diabetes(CAP+DM) group(n=88) according to whether they had diabetes, and then CAP+DM group(n=88) was divided into survival group(n=69) and death group(n =19) according to whether the patients died during hospitalization. The clinical data and laboratory test indicators of patients in different groups were compared. Cox regression analysis was used to screen the risk factors of death during hospitalization in the CAP+DM group. Receiver operating characteristic(ROC) curve was plotted to evaluate the predictive value of independent risk factors on hospitalization death. Results Compared with the simple CAP group, the CAP+DM group had significant differences in age, concomitant hypertension, coronary heart disease, CURB-65 score, neutrophil to lymphocyte ratio(NLR), C-reactive protein(CRP), procalcitonin(PCT), albumin(ALB), prealbumin(PA), glucose(GLU), serum potassium(K), calcium(Ca), phosphorus(P), magnesium(Mg), lactic acid(Lac), non-invasive ventilation time, ICU occupancy rate and mortality rate(P < 0.05); Compared with the survival group, there were statistically significant differences in CURB-65 score, NLR, CRP, PCT, GIU, ALB, PA, serum iron(Fe), Ca, non-invasive ventilation time, and ICU admission rate among the death group patients(P < 0.05). Cox regression analysis showed that the increase of NLR level and the decrease in PA level were the risk factors for in-hospital death in patients with CAP complicated with diabetes(P < 0.05). When the PA cutoff value was 91 mg/L, the AUC, sensitivity, and specificity for predicting in-hospital death of CAP patients with diabetes were 0.849, 84.2% and 81.2%, respectively. Conclusion Patients with CAP combined with diabetes are more serious and have worse prognosis than those with CAP alone. PA has a good predictive value for the prognosis of these patients. Early detection and active intervention should be carried out to reduce the in-hospital mortality of patients. -
Key words:
- Community-acquired pneumonia /
- Diabetes mellitus /
- Clinical features /
- Mortality rate /
- Prealbumin
-
表 1 单纯CAP组、CAP+DM组临床资料及化验指标比较[M(P25,P75)/n(%),d]
Table 1. Comparison of clinical data and laboratory indicators between CAP group and CAP+DM group[M(P25,P75)/n(%),d]
项目 单纯CAP(n=478) CAP+DM(n=88) χ2 P 年龄(岁) 57(40,73) 70(62,82) −6.296 <0.001* 男性 247(51.7) 53(60.2) 2.183 0.140 吸烟史 161(33.7) 23(26.1) 1.929 0.165 高血压 125(26.2) 64(72.7) 72.487 <0.001* 冠心病 33(6.9) 19(21.6) 19.215 <0.001* 抗生素使用天数 7.00(5.00,9.00) 7.00(5.25,9.00) −1.047 0.295 无创通气天数 0(0,0) 0(0,5) −2.842 0.004* 入住ICU 23(4.8) 14(15.9) 14.980 <0.001* 住院期间死亡 26(5.4) 19(21.6) 26.492 <0.001* CURB-65评分 0(0,1) 1(1,2) −5.467 <0.001* NLR 3.98(2.20,8.97) 6.03(3.40,12.46) −3.183 0.001* CRP(mg/L) 26.65(3.83,92.64) 56.05(10.00,135.07) −2.837 0.005* PCT(ng/L) 0.08(0.04,0.31) 0.18(0.07,1.11) −3.900 <0.001* ALB(g/L) 36.15(31.60,40.40) 31.85(27.00,36.00) −5.114 <0.001* PA(mg/L) 162.50(116.00,227.25) 118.50(78.00,180.25) −4.522 <0.001* Na(mmol/L) 139.75(138.00,141.50) 140.00(136.73,142.98) −0.646 0.518 K(mmol/L) 3.88(3.61,4,14) 3.76(3.36,4.09) −2.095 0.036* Ca(mmol/L) 2.14(2.01,2.26) 2.05(1.98,2.18) −3.266 0.001* P(mmol/L) 1.10(0.94,1.23) 1.03(0.78,1.18) −2.403 0.016* Mg(mmol/L) 0.86(0.80,0.91) 0.82(0.75,0.90) −2.276 0.023* Fe(μmol/L) 9.70(5.48,15.10) 8.90(5.48,13.15) −1.073 0.283 GIU(mmol/L) 5.14(4.65,5.94) 8.35(6.24,12.48) −9.811 <0.001* PH 7.44(7.42,7.47) 7.45(7.41,7.47) −0.065 0.949 PaO2(mmHg) 68.00(59.98,75.03) 67.95(57.55,75.68) −0.553 0.581 PaCO2(mmHg) 33.25(30.18,37.00) 32.55(29.00,35.68) −1.576 0.115 Lac(mmol/L) 1.40(1.00,1.90) 1.70(1.20,2.40) −3.661 <0.001* *P < 0.05。 表 2 CAP+DM患者存活组和死亡组临床资料及化验指标比较[$ \bar x \pm s $/M(P25,P75)/n(%),d]
Table 2. Comparison of clinical data and laboratory indicators between the survival and death groups of CAP+DM patients[M(P25,P75)/n(%),d]
项目 存活组(n =69) 死亡组(n =19) χ2/Z/t P 年龄(岁) 68(62,77) 79(64,85) −1.410 0.158 男性 39(56.5) 14(73.7) 1.832 0.176 吸烟史 19(27.5) 4(21.1) 0.075 0.784 高血压 50(72.5) 14(73.7) 0.011 0.916 冠心病 12(17.4) 7(36.8) 2.280 0.131 抗生素使用天数 7(6,9) 6(4,7) −1.852 0.064 无创通气天数 0(0,0) 6(3,7) −4.076 <0.001* 入住ICU 5(7.2) 9(47.4) 15.053 <0.001* CURB-65评分 1(0,2) 2(2,3) −4.858 <0.001* NLR 4.48(2.67,9.71) 13.82(7.33,22.42) −3.767 <0.001* CRP(mg/L) 45.36(5.15,118.66) 117.31(51.52,179.39) −2.896 0.004* PCT(ng/L) 0.12(0.06,0.41) 1.14(0.38,3.19) −4.042 <0.001* ALB(g/L) 33.00(30.40,38.40) 26.60(24.40,29.50) −3.808 <0.001* PA(mg/L) 148.74±69.31 72.79±29.72 7.048 <0.001* Na(mmol/L) 140.00(136.80,142.35) 142.10(134.80,150.40) −1.156 0.248 K(mmol/L) 3.79±0.58 3.62±0.63 1.134 0.260 Ca(mmol/L) 2.08(2.00,2.21) 1.89(1.83,2.01) −3.526 <0.001* P(mmol/L) 1.07(0.84,1.20) 0.87(0.69,1.14) −1.369 0.171 Mg(mmol/L) 0.82(0.77,0.90) 0.81(0.68,0.95) −0.441 0.659 Fe(μmol/L) 9.80(6.60,13.70) 5.70(3.00,8.00) −3.230 0.001* GIU(mmol/L) 7.78(6.15,10.44) 12.76(6.81,16.17) −2.586 0.010* PH 7.45(7.41,7.47) 7.43(7.40,7.48) −0.350 0.726 PaO2(mmHg) 68.00(60.35,74.40) 61.10(46.00,76.40) −1.065 0.287 PaCO2(mmHg) 32.60(29.30,35.80) 32.20(27.00,35.70) −0.675 0.500 Lac(mmol/L) 1.60(1.15,2.30) 2.10(1.46,3.10) −1.812 0.070 *P < 0.05。 表 3 CAP+DM患者住院期间死亡危险因素的 Cox回归分析(Forward LR法)
Table 3. Cox regression analysis of risk factors for mortality during hospitalization in CAP+DM patients (Forward LR method)
危险因素 β SE Wald P HR (95%CI) NLR 0.041 0.014 8.517 0.004* 1.042(1.014~1.072) PA −0.016 0.007 6.173 0.013* 0.984(0.971~0.997) *P < 0.05。 表 4 NLR、PA对CAP+DM患者住院期间死亡的预测价值
Table 4. Predictive value of PA on hospitalization death in patients with CAP+DM
变量 AUC(95%CI) 截断值 约登指数 灵敏度 特异度 P NLR 0.783(0.662~0.904) 11.89 0.473 0.632 0.841 <0.001* PA 0.849(0.764~0.934) 91.00 0.654 0.842 0.812 <0.001* *P < 0.05。 -
[1] Sun Y,Li H,Pei Z,et al. Incidence of community-acquired pneumonia in urban China: A national population-based study[J]. Vaccine,2020,38(52):8362-8370. doi: 10.1016/j.vaccine.2020.11.004 [2] Aliberti S,Dela C S,Amati F,et al. Community-acquired pneumonia[J]. Lancet,2021,398(10303):906-919. doi: 10.1016/S0140-6736(21)00630-9 [3] Baker E H,Baines D L. Airway glucose homeostasis[J]. Chest,2018,153(2):507-514. doi: 10.1016/j.chest.2017.05.031 [4] Zeng W,Huang X,Luo W,et al. Association of admission blood glucose level and clinical outcomes in elderly community‐acquired pneumonia patients with or without diabetes[J]. The Clinical Respiratory Journal,2022,16(8):562-571. doi: 10.1111/crj.13526 [5] Klein O L,Krishnan J A,Glick S,et al. Systematic review of the association between lung function and Type 2 diabetes mellitus[J]. Diabetic Medicine,2010,27(9):977-987. doi: 10.1111/j.1464-5491.2010.03073.x [6] 中华医学会呼吸病学分会. 中国成人社区获得性肺炎诊断和治疗指南(2016年版)[J]. 中华结核和呼吸杂志,2016,39(4):253-279. doi: 10.3760/cma.j.issn.1001-0939.2016.04.005 [7] 陈亮,韩秀迪,李艳丽,等. 糖尿病合并社区获得性肺炎住院患者临床特征和死亡危险因素分析[J]. 中国糖尿病杂志,2021,29(1):14-19. doi: 10.3969/j.issn.1006-6187.2021.01.004 [8] 邓伟吾. 糖尿病的肺功能损害和肺部并发症[J]. 临床肺科杂志,2010,15(7):903-905. doi: 10.3969/j.issn.1009-6663.2010.07.001 [9] Di Y S,Garcia-Vidal C,Viasus D,et al. Clinical features,etiology,and outcomes of community-acquired pneumonia in patients with diabetes mellitus[J]. Medicine,2013,92(1):42-50. doi: 10.1097/MD.0b013e31827f602a [10] Huang D,He D,Gong L,et al. Clinical characteristics and risk factors associated with mortality in patients with severe community-acquired pneumonia and type 2 diabetes mellitus[J]. Critical Care,2021,25(1):419. doi: 10.1186/s13054-021-03841-w [11] Arias F L,Pardo S J,Cebey-López M,et al. Differences between diabetic and non-diabetic patients with community-acquired pneumonia in primary care in Spain[J]. BMC Infect Dis,2019,19(1):973. doi: 10.1186/s12879-019-4534-x [12] Cheng S,Hou G,Liu Z,et al. Risk prediction of in-hospital mortality among patients with type 2 diabetes mellitus and concomitant community-acquired pneumonia[J]. Annals of Palliative Medicine,2020,9(5):3313-3325. doi: 10.21037/apm-20-1489 [13] Khan R N,Saba F,Kausar S F,et al. Pattern of electrolyte imbalance in type 2 diabetes patients: Experience from a tertiary care hospital[J]. Pakistan Journal of Medical Sciences,2019,35(3):797-801. [14] Wang S Q,Lu D X,Zhang J D,et al. The association between abnormal serum magnesium levels and prognosis of elderly patients with community-acquired pneumonia[J]. Magnesium Research,2021,34(4):159-165. doi: 10.1684/mrh.2022.0493 [15] Liu X L,Wang S Q,Ji M J,et al. Hypomagnesemia is associated with increased mortality in the short-term but not the long-term in community-acquired pneumonia patients with type 2 diabetes[J]. Magnesium Research,2022,35(2):33-38. doi: 10.1684/mrh.2022.0499 [16] Smith S H. Using albumin and prealbumin to assess nutritional status[J]. Nursing,2017,47(4):65-66. doi: 10.1097/01.NURSE.0000511805.83334.df [17] Li T,Guo Y,Zhuang X,et al. Abnormal liver-related biomarkers in COVID-19 patients and the role of prealbumin[J]. Saudi Journal of Gastroenterology,2020,26(5):272-278. doi: 10.4103/sjg.SJG_239_20 [18] Gamarra-Morales Y,Molina-López J,Machado-Casas J F,et al. Influence of Nutritional Parameters on the Evolution,Severity and Prognosis of Critically Ill Patients with COVID-19[J]. Nutrients,2022,14(24):5363. doi: 10.3390/nu14245363 [19] Zhang H F,Li L Q,Ge Y L,et al. Serum prealbumin improves the sensitivity of pneumonia severity index in predicting 30-day mortality of CAP patients[J]. Clinical Laboratory,2020,66(5):811-818. [20] Parthasarathi A,Padashetti V C,Padukudru S,et al. Association of serum albumin and copeptin with early clinical deterioration and instability in community-acquired pneumonia[J]. Advances in Respiratory Medicine,2022,90(4):323-337. doi: 10.3390/arm90040042 [21] Miyazaki H,Nagata N,Akagi T,et al. Comprehensive analysis of prognostic factors in hospitalized patients with pneumonia occurring outside hospital: Serum albumin is not less important than pneumonia severity assessment scale[J]. Journal of Infection and Chemotherapy,2018,24(8):602-609. doi: 10.1016/j.jiac.2018.03.006 [22] Akbar M R,Pranata R,Wibowo A,et al. The association between serum prealbumin and poor outcome in COVID-19-Systematic review and meta-analysis[J]. European Review for Medical and Pharmacological Sciences,2021,25(10):3879-3885. [23] Jensen A V,Faurholt-Jepsen D,Egelund G B,et al. Undiagnosed diabetes mellitus in community-acquired pneumonia: a prospective cohort study[J]. Clinical Infectious Diseases,2017,65(12):2091-2098. doi: 10.1093/cid/cix703 [24] Al-Khlaiwi T,Alsabih A O,Khan A,et al. Reduced pulmonary functions and respiratory muscle strength in Type 2 diabetes mellitus and its association with glycemic control[J]. European Review for Medical and Pharmacological Sciences,2021,25(23):7363-7368. -





 下载:
下载:


