The Relationship between Arterial and Venous Blood Lactic Acid in Early Stage of Septic Shock and Prognostic Value of Lactate and Lactate Clearance Rate
-
摘要:
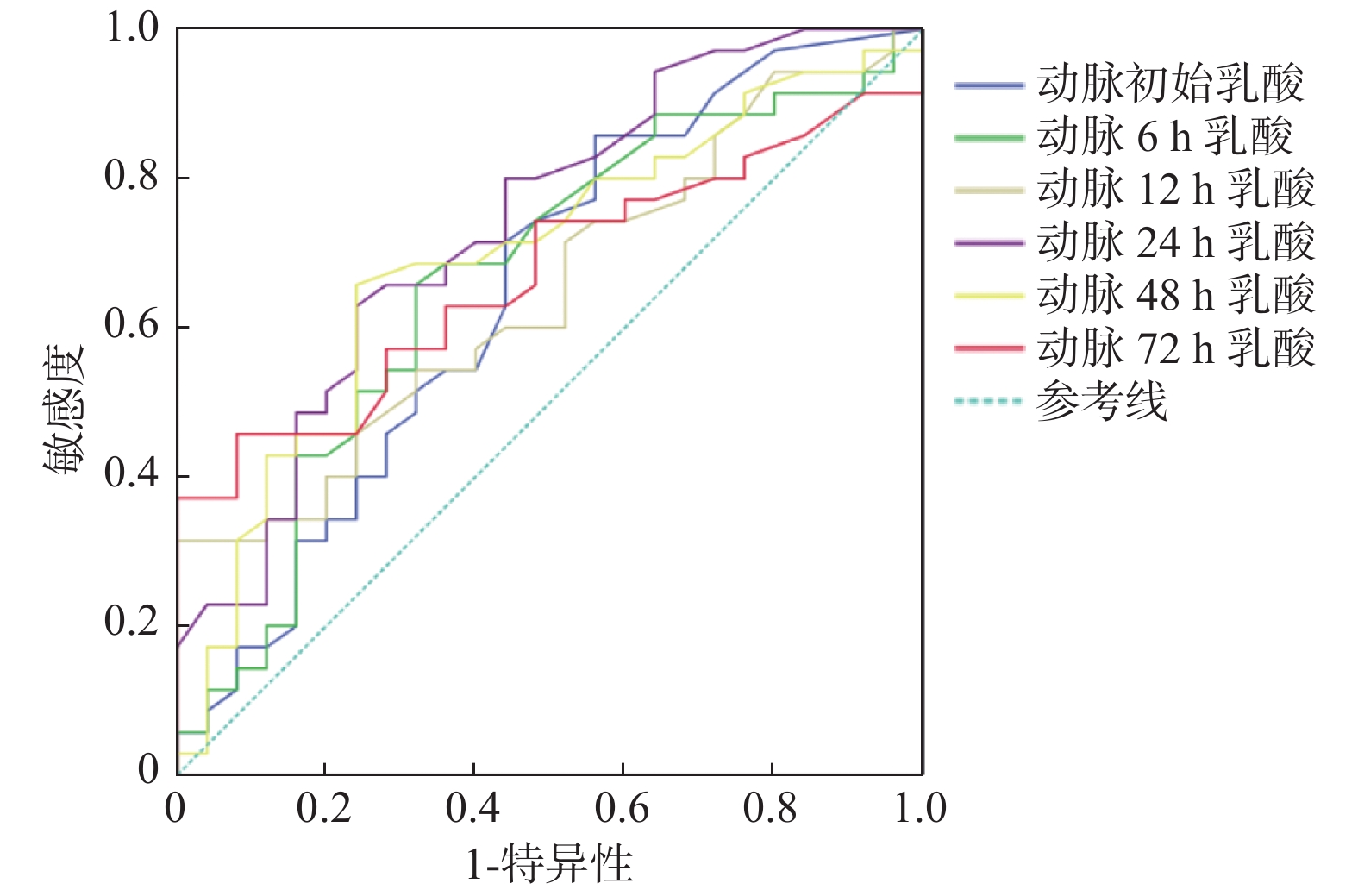
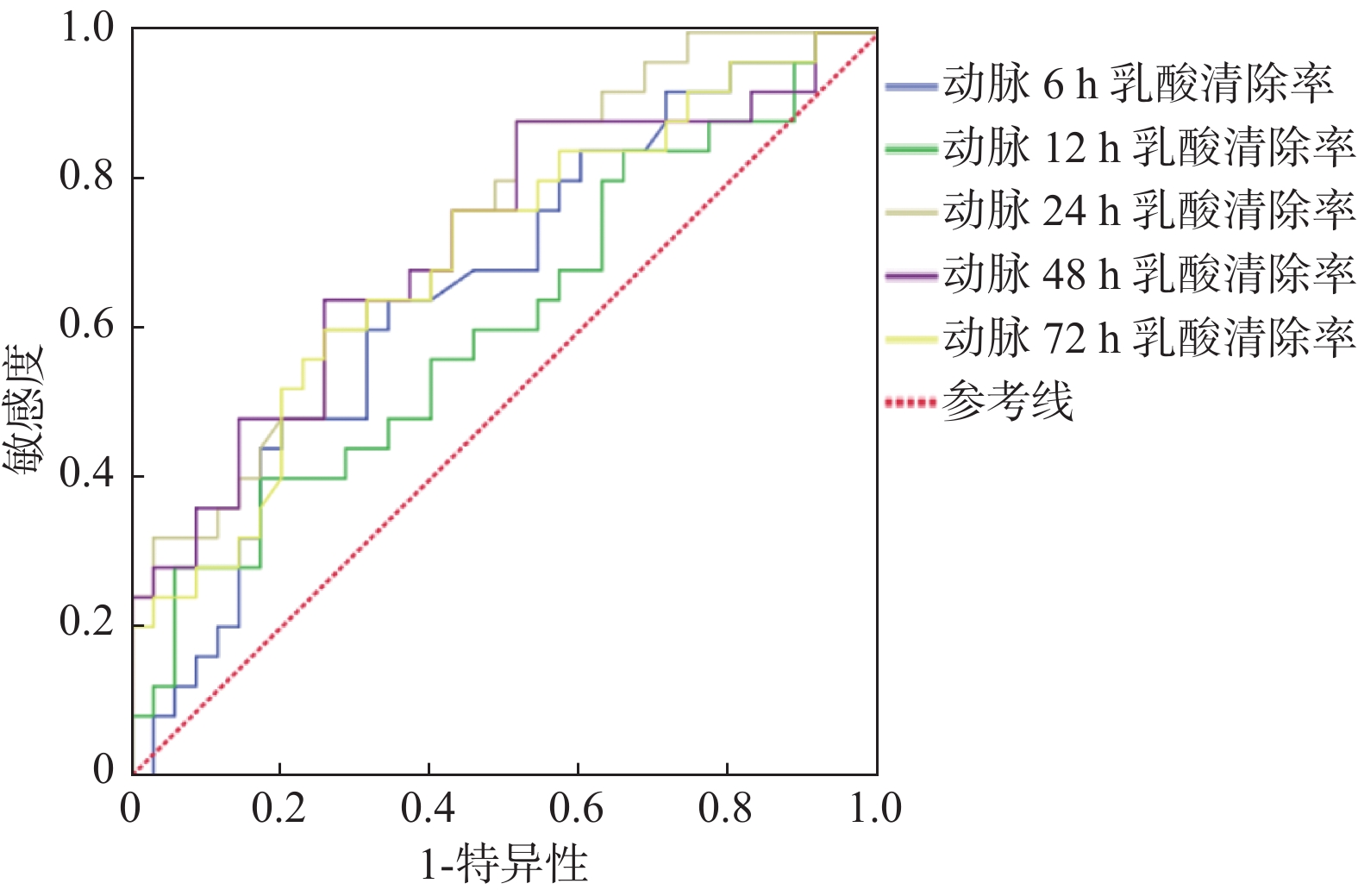
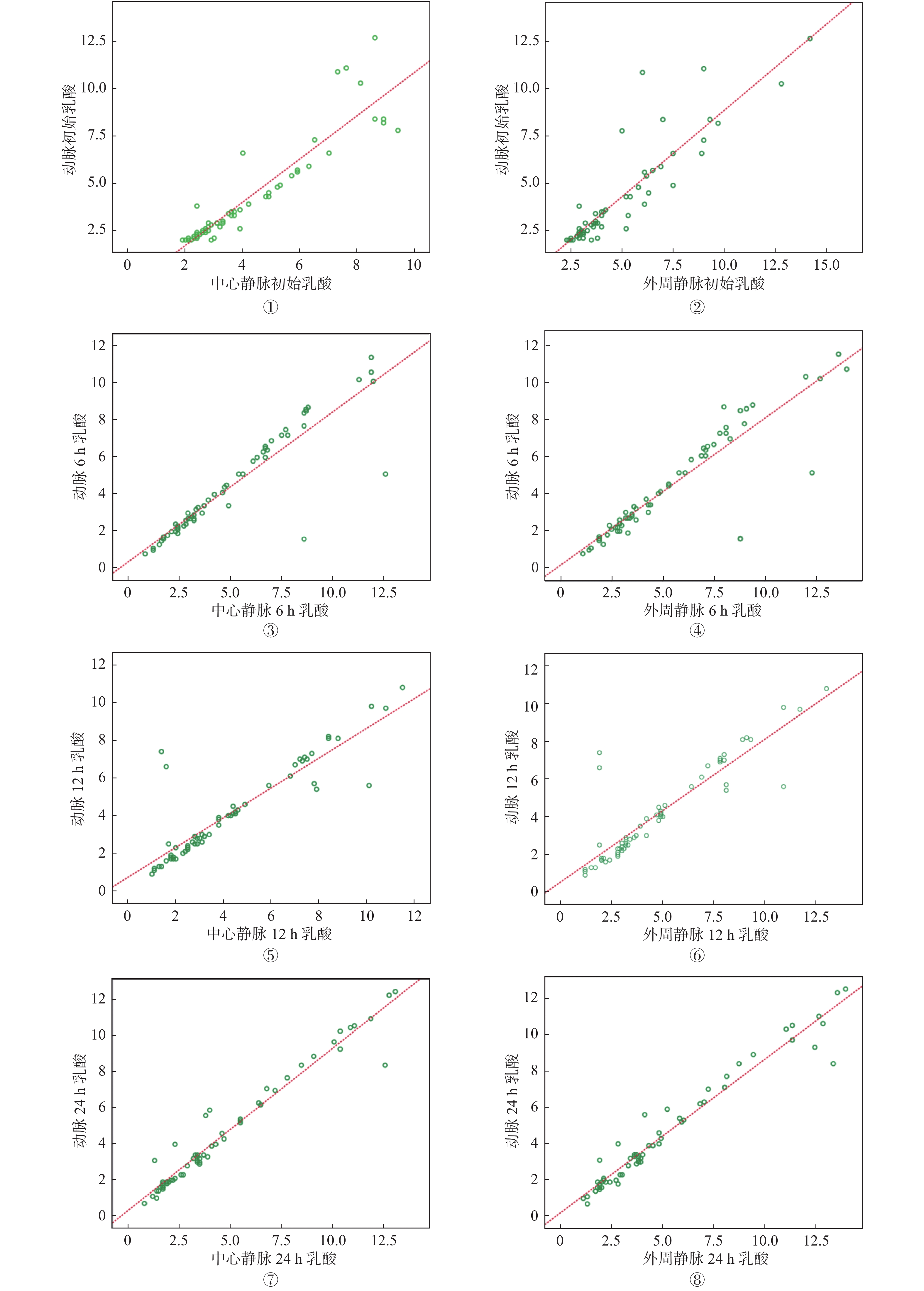
目的 分析脓毒性休克患者的动脉、中心静脉及外周静脉血乳酸浓度的相关性,探讨不同时间段血乳酸、乳酸清除率对脓毒性休克患者预后的评估价值。 方法 选择昆明医科大学第一附属医院3号楼ICU 2020年6月至2021年2月期间收治的60例脓毒性休克患者为研究对象,收集入组患者一般资料,监测入住ICU时及治疗后6 h、12 h、24 h动脉、外周静脉、中心静脉血血气参数,以及48 h、72 h动脉血血气参数。首先根据血样本的来源分为动脉、中心静脉、外周静脉组,分析3组之间血乳酸浓度的相关性,然后根据患者28 d存活情况分为死亡组和存活组,探讨早期不同时间段血乳酸、乳酸清除率对病情预后的评估价值。 结果 (1)经Pearson相关性分析,入住ICU时及治疗后6 h、12 h、24 h动脉与中心静脉乳酸值具有相关性,各时间段r值在0.89~0.90之间,P < 0.05;入住ICU时及治疗后6 h、12 h、24 h动脉与外周静脉乳酸值具有相关性,各时间段r值在0.83~0.87之间,P < 0.05;(2)经绘制ROC曲线,初始及治疗后6 h、12 h、24 h、48 h、72 h动脉乳酸AUC分别为0.64,0.62,0.64,0.72,0.66,0.63,P < 0.05,动脉24 h乳酸AUC最大,其最佳截断值 = 2.42 mmol/L,灵敏度 = 0.64,特异度 = 0.66;(3)经绘制ROC曲线,6 h、12 h、24 h、48 h、72 h动脉乳酸清除率AUC分别为0.66,0.61,0.74,0.72,0.70,P < 0.05,24 h乳酸清除率AUC最大,其最佳截断值 = 19.57%,灵敏度 = 0.64,特异度 = 0.68。 结论 (1)脓毒性休克患者早期动脉与中心静脉、外周静脉血乳酸水平具有相关性;(2)治疗后24 h的动脉血乳酸及乳酸清除率对脓毒性休克患者预后具有较好的评估价值。 Abstract:Objectives To analyze the correlation of blood lactate concentration in artery, central vein and peripheral vein of patients with septic shock, and to explore the value of blood lactate and lactate clearance rate in different periods of time in evaluating the prognosis of patients with septic shock. Methods A total of 60 patients with septic shock in ICU of building 3 of the First Affiliated Hospital of Kunming Medical University from June 2020 to February 2021 were selected as the research objects. The general data of the patients were collected, and the blood gas parameters of artery, peripheral vein and central vein at admission and 6 h, 12 h and 24 h after treatment, as well as arterial blood gas parameters at 48 h and 72 h after the treatment were monitored. First, according to the source of blood samples, they were divided into the artery group, the central vein group and the peripheral vein group. The correlation of blood lactic acid concentration in artery, central vein and peripheral vein was analyzed. Then, according to the 28 day survival of patients, they were divided into the death group and the survival group. The evaluation value of blood lactic acid and lactic acid clearance rate in different periods of early stage on the prognosis of patients was discussed. Results (1) According to Pearson correlation analysis, there was a correlation between arterial lactic acid and central venous lactic acid at ICU admission and 6 h, 12 h, 24 h after the treatment, with r value between 0.89-0.90 at each time period, P < 0.05; there was a correlation between arterial lactic acid and peripheral venous lactic acid at ICU admission and 6 h, 12 h, 24 h after treatment, with r value between 0.83-0.87 at each time period, P < 0.05. (2) By drawing ROC curve, the AUC of arterial lactic acid at the initial and 6 h, 12 h, 24 h, 48 h and 72 h after the treatment were 0.64, 0.62, 0.64, 0.72, 0.66, 0.63, respectively, P < 0.05. The AUC of arterial lactate was the highest at 24 h, with the best cutoff value of 2.42 mmol/L, sensitivity of 0.64 and specificity of 0.66. (3) By drawing the ROC curve, the AUC of arterial lactic acid clearance at 6 h, 12 h, 24 h, 48 h and 72 h were 0.66, 0.61, 0.74, 0.72 and 0.70, respectively, P < 0.05. The AUC of 24 h lactate clearance was the highest, with the best cutoff value of 19.57%, sensitivity of 0.64 and specificity of 0.68. Conclusions (1) There is a correlation between arterial and central venous blood lactic acid levels and between arterial and peripheral venous blood lactic acid levels in patients with septic shock. (2) The arterial lactate and lactate clearance rate 24 hours after the treatment have a good evaluation value for the prognosis of patients with septic shock. -
Key words:
- Septic shock /
- Blood lactate /
- Lactate clearance rate /
- Prognosis evaluation
-
全球近视和高度近视患者近十余年来呈现快速增长的趋势,Holden等[1]纳入了145个研究数据,涉及210万参与者。该研究显示2000年全球有14. 06亿近视患者(22.9%)和1.63亿高度近视患者(2.7%);到2050年,近视人群将上升到47.58亿(49.8%),高度近视人群达到9.38亿(9.8%)。我国是近视发病率较高的国家,儿童及青少年近视呈现发病早、进展快、高度近视比例增高的特点,预防近视和控制近视度数增高已成为国家疾病预防和眼保健的重要内容。过去在近视的诊断中,屈光度为唯一的金标准,近年来眼轴对于近视评价也显示出了肯定的作用[2]。本研究调查学龄儿童眼屈光发育参数的年龄特点,在不同屈光状态中的变化和相关性,寻求更多有价值的近视评价指标。
1. 资料与方法
1.1 研究对象
横断面研究,收集2023年9月至11月在云南省楚雄市北浦小学7~12岁小学生中开展视力筛查的资料。检查内容有屈光度(SE/DS/DC)和屈光发育参数,包括:眼轴(axis length,AL)、角膜曲率(K)、中央前房深度(anterior chamber depth,ACD)、中央角膜厚度(central corneal thickness,CCT)、晶状体厚度(lens thickness,LT)、玻璃体深度(vitreous chamber depth,VD)。最终纳入检查记录完整的资料有
1463 名,其中男生735名,女生728名,右眼数据纳入分析。参与本次研究的学生及监护人均知情同意。1.2 研究方法
(1)基本信息:记录学生姓名、年龄和性别等;(2)视力检查:使用统一的标准对数视力表,检查距离为5 m,检查裸眼远视力(uncorrected distance visual acuity,UCVA);(3)屈光检查:非睫状肌麻痹验光,自动电脑验光仪每眼验光3次,取平均值,获取球镜度数(spherical degree,DS)、柱镜度数(cylenderical degree,DC)、等效球镜度(spherical equivalent degree,SE)。根据SE度数将屈光状态分为近视(SE ≤-0.50D),远视(SE≥+0.50D),正视(-0.50D < SE < +0.50D),散光定义为DC≥0.75D;(4)屈光参数测量:采用眼科光学生物测量仪( SW9000) 测量受检者AL、角膜屈率(K1,K2)、ACD、CCT、LT、VD。角膜曲率平均值K = (K1+K2)/2,计算角膜曲率半径CR =
1000 (n2-n1)/K(n1为空气屈光指数1.00,n2为角膜曲率屈光指数1.3375 ),然后计算AL/CR比值。晶状体度数(lens power,LP)使用Bennett公式进行计算[3],LP = -1000n(Scv+Km)]/[1000n-(ACD+C1LT)x(Scv+Km)]+1000n/(C2LT+VD),Scv = SE/(1-0.014XSE),C1 = 0.596,C2 = 0.358,n =1.3375 。1.3 统计学分析
采用SPSS 25.0软件进行统计分析,计数资料使用$ {\chi }^{2} $检验,计量资料不符合正态分布,用中位数及四分位数的方式来表示,即P50(P25,P75),组间比较采用秩和检验,单个因素与SE的关系分析采用Spearman线性相关分析,P < 0.05为差异有统计学意义。
2. 结果
2.1 一般情况
1 463名中年龄中位数为9岁,其中男孩735名(50.24%),女孩728名(49.76%)。近视647名(44.22%);正视532名(36.36%);远视284名(19.42%);散光293名(20.04%)。不同性别之间:DC、AL/CR比较,差异无统计学意义(P > 0.05),其余参数均有统计学意义(P < 0.05)。其中,女孩的DS较男孩偏负(P < 0.05);女孩的AL、CCT、ACD、VD、CR大于男孩(P < 0.05);而K、LT、LP小于男孩(P < 0.05)。计算7~8岁、9~10岁、11~12岁各年龄段近视的患病率,3组之间差异有统计学意义(P < 0.05),不同年龄组两两比较,差异均有统计学意义(P < 0.05),见表1。
表 1 各年龄段近视的患病率比较 [n(%)]Table 1. Comparison of myopia prevalence by age group [n(%)]年龄段(岁) 总人数 近视人数 患病率(%) $ {\chi }^{2} $ P 7~8 518 139 26.8 114.13 < 0.001* 9~10 547 268 49.0 11~12 398 243 61.1 *P < 0.05。 2.2 不同年龄组屈光参数比较
将年龄段分为7~8岁,9~10岁,11~12岁3组,各组之间的DS、DC、SE、AL、AL/CR、LP、LT、ACD、VD比较,差异有统计学意义(P < 0.05)。DS、SE、AL、AL/CR、LP、LT、ACD、VD两两比较,差异均有统计学意义(P < 0.05)。DC仅7~8岁与11~12岁比较差异有统计学意义(P < 0.05),即随着年龄增加,DS、SE表现为近视度数增加,AL、AL/CR、ACD、VD数值逐渐增加,而LT、LP逐渐下降。各组之间K、CR、CCT比较,差异均无统计学意义(P > 0.05),见表2。
表 2 不同年龄组屈光度和眼屈光参数的分布[P50(P25,P75)]Table 2. Distribution of diopter and ocular biological parameters by age group at different ages[P50(P25,P75)]参数 7~8岁(n = 518) 9~10岁(n = 547) 11~12岁(n = 398) H P DS(D) 0.25(−0.25,0.50) −0.25(−1.25,0.25) −0.75(−2.00,0.25) 148.82 < 0.001* DC(D) 0(−0.50,0) 0(−0.50,0) 0(−0.50,0) 6.874 0.032* SE(D) 0(−0.50,0.50) −0.375(−1.375,0.25) −1.00(−2.25,0.00) 143.105 < 0.001* K(D) 43.25(42.25,44.26) 43.23(42.37,44.23) 43.28(42.28,44.27) 0.163 0.922 AL(mm) 23.01(22.45,23.52) 23.43(22.87,24.05) 23.75(23.08,24.60) 169.651 < 0.001* CR(mm) 7.80(7.63,7.99) 7.81(7.63,7.97) 7.80(7.62,7.98) 0.163 0.922 AL/CR 2.94(2.90,2.99) 3.00(2.94,3.07) 3.04(2.97,3.14) 252.016 < 0.001* LT(mm) 3.60(3.47,3.77) 3.48(3.36,3.62) 3.44(3.32,3.56) 143.49 < 0.001* ACD(mm) 2.87(2.70,3.05) 3.02(2.83,3.18) 3.08(2.89,3.24) 121.416 < 0.001* VD(mm) 15.95(15.44,16.52) 16.43(15.87,16.96) 16.78(16.08,17.51) 174.915 < 0.001* CCT(mm) 537.00(517,560.3) 542(522,562) 543(520,564) 3.186 0.203 LP(D) 25.89(24.61,27.14) 24.51(23.47,25.87) 24.00(22.86,25.13) 208.466 < 0.001* *P < 0.05。 2.3 不同屈光状态组中眼屈光参数的比较
按屈光状态分为近视、正视、远视3组,各组之间的AL、AL/CR、LT、LP、ACD、VD差异有统计学意义(P < 0.05),其中,AL、AL/CR、LP、ACD两两比较,差异均有统计学意义(P < 0.05)。正视组和远视组比较,LT和VD差异无统计学意义(P > 0.05)。随着屈光状态从远视、正视向近视转变,AL、AL/CR、ACD逐渐增大,而LP逐渐减小。K、CR、CCT在不同屈光状态之间差异无统计学意义(P > 0.05),见表3。
表 3 不同屈光状态组眼屈光参数的比较[P50(P25,P75)]Table 3. Comparison of ocular biological parameters in different refractive state groups[P50(P25,P75)]指标 近视(n = 647) 正视(n = 532) 远视(n = 284) H P SE(D) −1.50(−2.50,−0.75) 0.00(−0.25,0.25) 0.63(0.50,0.75) 1260.078 < 0.001* K(D) 43.31(42.34,44.35) 43.25(42.33,44.18) 43.12(42.13,44.05) 3.214 0.200 AL(mm) 23.88(23.20,24.61) 23.12(22.60,23.60) 22.98(22.45,23.40) 298.07 < 0.001* CR(mm)
AL/CR
LT(mm)
ACD(mm)
VD(mm)
CCT(mm)
LP(D)7.79(7.61,7.97)
3.06(2.98,3.14)
3.44(3.31,3.61)
3.09(2.89,3.25)
16.83(16.17,17.51)
541(519,563)
24.37(23.14,26.09)7.80(7.64,7.97)
2.96(2.92,3.01)
3.54(3.43,3.71)
2.92(2.76,3.09)
16.05(15.59,16.56)
539(521,560)
25.29(24.09,26.64)7.83(7.66,8.01)
2.93(2.89,2.98)
3.57(3.43.3.72)
2.87(2.71,3.02)
15.98(15.42,16.43)
541(514,565)
24.83(23.87,26.04)3.214
444.08
99.428
149.686
269.512
0.383
54.4920.200
< 0.001*
< 0.001*
< 0.001*
< 0.001*
0.826
< 0.001**P < 0.05。 2.4 屈光发育参数与SE的相关性分析
与屈光发育密切的AL、CR、AL/CR、LP和SE呈现出不同的相关性:近视组中AL、AL/CR与SE呈负相关(rs = -0.617;rs = -0.737,P < 0.05),AL/CR与SE的相关性高于AL。LP与SE呈正相关(rs = 0.412,P < 0.05)。正视组中AL/CR与SE呈负相关(rs = -0.134,P < 0.05),而AL、LP与SE无相关性(P > 0.05)。远视组中,AL、AL/CR与SE呈负相关(rs = -0.318;r = -0.406,均为P < 0.05),AL/CR与SE的相关性高于AL,LP与SE呈正相关(rs = 0.182,P < 0.05)。在3组中CR与SE均无相关性(P > 0.05),见表4。
表 4 不同屈光发育参数与SE的相关性分析Table 4. Correlation analysis between different refractive parameters and SE组别 AL vs SE AL/CR vs SE CR vs SE LP vs SE rs P rs P rs P rs P 近视组 −0.617 < 0.001* −0.737 < 0.001* 0.044 0.259 0.412 < 0.001* 正视组 −0.056 0.198 −0.134 0.002* 0.021 0.624 −0.069 0.112 远视组 −0.318 < 0.001* −0.406 < 0.001* 0.008 0.888 0.182 0.002* *P < 0.05。 3. 讨论
3.1 儿童屈光发育参数变化
在儿童眼球的发育中,屈光度(SE)、眼轴长度(AL)、角膜曲率(K)及晶状体屈光度(LP)之间是一个动态匹配的过程,各个参数会受到遗传因素和环境因素的影响[4]。随着人眼的发育,远视度数逐渐降低而向正视转变,这个过程叫正视化进程。这个进程的快慢与屈光发育参数相关,对于近视防控意义重大。婴儿出生后不久,AL相对较短,角膜弯曲度较大,晶状体厚度较厚,角膜对应的曲率K和晶状体对应的LP较大,SE表现为远视;随年龄增长眼轴变长,角膜变平坦,晶状体厚度变薄,K值和LP逐渐下降,远视减少。AL、K、LP在3岁前变化明显,3~6岁以后变化减缓直至青少年时期[5]。
本研究显示,7~12岁儿童随年龄增加SE、DS、LT、LP逐渐变小(P < 0.05),而AL、AL/CR、ACD、VD逐渐增大(P < 0.05)。这些改变符合儿童眼球正视化中随年龄增加眼球不断发育的特征,其中晶状体的纤维和内部结构发生改变,晶状体厚度变薄带来晶状体屈光度的下降,这能够抵消一部分眼轴增长带来的近视进展[6−7]。本研究还发现,这个年龄段眼球的角膜形态趋于稳定,对应的CR、K、CCT随年龄增长无变化(P > 0.05),女孩的屈光度(SE、DS)比男孩更偏负值,眼轴更长。上述结论同以往较多研究的结果相似[8−9]。
3.2 儿童屈光度变化的评价指标
目前,近视临床评估主要指标是屈光度和眼轴长度。本研究中7~8岁近视患病率为7.8%,SE为0.25D(-0.25,0.50);9~10岁近视患病率为49%,SE为-0.25D(-1.25,0.25);11~12岁近视患病率为61%,SE为-0.75D(-2.00,0.25),表现出随年龄增加近视屈光度增高,近视患病率增加。
眼轴的增长代表着眼球的发育,新生儿AL长度约为16.5 mm,3岁之内增长较快,随后增长变缓,3~6岁AL平均值为(22.39±0.68)mm,6岁后每年平均以0.09 mm 的速度增长,15岁时约为23.39 mm [参考区间(22.10~24.68) mm][5,10−11]。本研究中AL随年龄增加,从7~8岁的23.01 mm增长到9~10岁的23.43 mm,11~12岁的23.75 mm。正视者眼轴为23.12 mm(22.60,23.60),近视者眼轴为23.88 mm(23.20,24.61),远视者眼轴为22.98 mm(22.45,23.40),在3组中差异均有统计学意义(P < 0.05),说明眼轴对于决定屈光状态有重要意义。
本研究还发现,除SE、AL以外,AL/CR、LP、ACD在3个不同屈光状态组、不同年龄组之间均有差异性,原因可能为眼球发育和眼轴增长带来的相应变化。其中AL、AL/CR、LP与SE呈现出不同的相关性,与既往研究相似[12]。AL、AL/CR、ACD值增大,LP减小可以作为儿童屈光变化的预测及评估参考指标。
3.3 AL/CR在屈光不正中的评价作用
在近视人群中,有些眼轴已经超过了24 mm,但角膜曲率较低,结果并没有近视或仅呈现低度近视;而有些眼轴正常甚至偏短,但角膜曲率偏高,结果表现为近视。故对于屈光状态的评价,需综合眼轴和角膜曲率的变化。有研究发现在调整了年龄和性别后的多元线性回归模型中,随年龄增加SE和AL、AL/CR呈线性负相关,而对于近视的评价,AL/CR较AL更有参考意义[5]。李童等[13]的研究也发现AL / CR相对于AL和小瞳孔下电脑验光来说,可以更好地评估屈光状态。
本研究中AL和近视、远视均有相关性,但和正视无关;而AL/CR和近视、远视、正视均有相关性,因此对于评价屈光状态是连续性的。在近视组中,AL、AL/CR与SE呈负相关(rs = -0.617;rs = -0.737,P < 0.05),从相关系数来看AL/CR与近视的相关性比AL更高。远视亦是如此。而在正视组中AL/CR与SE相关性较低(rs = -0.134,P < 0.05)。类似的研究如He等[14]发现在6~12岁儿童中,AL/CR与SE相关性在中度远视和近视中较高,而在正视儿童中较低。廖梦霏等[15]也发现SE与AL/CR的相关性在近视儿童中相关性最高,且高于单独的AL。Grosvenor等[16]发现正视眼的AL/CR值接近3/1,Blanco等[17]也认为AL/CR > 3可作为诊断近视的高危指标。本研究中AL/CR在近视、正视、远视组中分别为3.06、2.96和2.93,3组之间差异有统计学意义(P < 0.05)。因此,AL/CR值等于3可以作为一个近视眼与非近视眼之间的初步评估界限值。
AL/CR随年龄增高有逐渐增高的趋势,例如一项14年的纵向队列研究,平均年龄为9.3岁,AL/CR为3.15;14年后AL/CR增至3.31 D[18]。本研究中7~8岁AL/CR为2.94,9~10岁为3,11~12岁为3.04,考虑和不同年龄的近视率有关,9岁以下近视患病率低,AL/CR < 3,而9岁后近视患病率增高,AL/CR > 3。笔者认为在儿童屈光筛查中,由于睫状肌麻痹验光的局限性,包括耗时、儿童不配合、家长不接受等因素,利用生物测量仪检查并计算出AL/CR值来预测和判断近视也是一种可靠的方法和重要补充。
综上所述,本研究发现7~12岁儿童的屈光发育中,AL、AL/CR、ACD、VD随年龄增长而增大,SE、DS、LT、LP随年龄增长而变小,而K、CR、CCT基本稳定;AL/CR和AL可作为近视的重要监测指标,AL/CR较AL与SE的相关性更高。K、CR、LT、LP等生物学参数,有待进一步明确其作为评价儿童屈光状态指标的可能性。
-
表 1 基本情况比较[
$ \bar x \pm s $ /n(%)]Table 1. The comparison of basic data [
$ \bar x \pm s $ /n(%)]指标 存活组(n = 25) 死亡组(n = 35) χ2/t P 性别 0.019 0.891 男 16 23 女 9 12 年龄(岁) 63.20 ± 11.98 74.11 ± 14.95 −3.021 0.004* 感染部位(n) 4.402 0.221 腹腔 10 6 肺部 11 22 皮肤软组织 2 5 其他 2 2 APACHE Ⅱ评分 21.08 ± 6.54 25.54 ± 6.54 −2.606 0.012* SOFA评分 10.24 ± 2.49 12.06 ± 2.92 −2.524 0.014* *P < 0.05。 表 2 动脉与中心静脉、外周静脉乳酸相关性分析[(
$ \bar x \pm s $ ),mmol/L]Table 2. Correlation analysis between arterial,central vein and peripheral vein lactic acid [(
$ \bar x \pm s $ ),mmol/L]指标 $ \bar x \pm s $ r P 初始中心静脉乳酸 4.12 ± 2.42 0.90 < 0.001* 初始外周静脉乳酸 4.34 ± 1.87 0.85 < 0.001* 6 h中心静脉乳酸 4.21 ± 1.63 0.89 < 0.001* 6 h外周静脉乳酸 4.42 ± 1.72 0.83 < 0.001* 12 h中心静脉乳酸 3.52 ± 1.92 0.89 < 0.001* 12 h外周静脉乳酸 3.72 ± 1.02 0.86 < 0.001* 24 h中心静脉乳酸 4.03 ± 1.02 0.90 < 0.001* 24 h外周静脉乳酸 4.31 ± 1.63 0.87 < 0.001* *P < 0.05。 表 3 2组患者动脉血乳酸比较[(
$ \bar x \pm s $ ),mmol/L]Table 3. Comparison of arterial blood lactic acid between 2 groups [(
$ \bar x \pm s $ ),mmol/L]分组 治疗开始时 6 h 12 h 24 h 48 h 72 h F P 存活组 3.60 ± 2.33 3.26 ± 2.40 2.92 ± 1.69 2.45 ± 1.68 2.41 ± 1.92 2.41 ± 1.66 17.217 < 0.001* 死亡组 4.53 ± 2.79 5.04 ± 3.01 4.88 ± 2.92 5.97 ± 3.89 6.21 ± 4.02 6.55 ± 4.62 *P < 0.05。 表 4 2组患者乳酸清除率比较(
$ \bar x \pm s $ )Table 4. Comparison of lactic acid clearance rate between 2 groups (
$ \bar x \pm s $ )分组 6 h 12 h 24 h 48 h 72 h F P 存活组 8.28 ± 4.26 7.22 ± 2.18 22.11 ± 4.88 71.26 ± 40.40 82.61 ± 53.56 10.373 0.002* 死亡组 −20.40 ± 8.22 −18.27 ± 8.81 −54.17 ± 9.72 −9.06 ± 6.22 −3.35 ± 1.54 *P < 0.05。 -
[1] Singer M,Deutschman C S,Seymour C W,et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3)[J]. JAMA,2016,315(8):801-810. doi: 10.1001/jama.2016.0287 [2] Stefan Kluge,Geraldine de Heer,Dominik Jarczak,et al. Laktatazidose-update 2018[J]. DMW - Deutsche Medizinische Wochenschrift,2018,143,(15):1082-1085. [3] Bolvardi E,Malmir J,Reihani H,et al. The role of lactate clearance as a predictor of organ dysfunction and mortality in patients with severe sepsis.[J]. Mater Sociomed,2016,28(1):57-60. doi: 10.5455/msm.2016.28.57-60 [4] Chauvin A,Javaud N,Ghazali A,et al. Reducing pain by using venous blood gas instead of arterial blood gas (VEINART):A multicentre randomised controlled trial[J]. Emerg Med J.,2020,37(12):756-761. [5] 曹钰,柴艳芬,邓颖,等. 中国脓毒症/脓毒性休克急诊治疗指南(2018)[J]. 临床急诊杂志,2018,19(09):567-588. [6] 卜会驹,杨秀洁,杭寒皎,等. 中心静脉和动脉血气联合分析在脓毒血症患者诊疗中的预警作用[J]. 中国煤炭工业医学杂志,2009,12(06):861-864. [7] Nascente A P,Assunção M,Guedes C J,et al. Comparison of lactate values obtained from different sites and their clinical significance in patients with severe sepsis[J]. Sao Paulo Med J,2011,129(1):11-16. doi: 10.1590/S1516-31802011000100003 [8] Contenti J,Corraze H,Lemoël F,et al. Effectiveness of arterial,venous,and capillary blood lactate as a sepsis triage tool in ED patients[J]. Am J Emerg Med,2015,33(2):167-172. doi: 10.1016/j.ajem.2014.11.003 [9] Wernly B,Bakker J,Jung C. Venous blood lactate concentrations in patients with shock:Interesting but not really helpful[J]. J Crit Care,2020,58(8):125-126. [10] Coopersmith C M,De Backer D,Deutschman C S,et al. Surviving sepsis campaign:Research priorities for sepsis and septic shock[J]. Intensive Care Med,2018,44(9):1400-1426. doi: 10.1007/s00134-018-5175-z [11] Puskarich M A,Trzeciak S,Shapiro N I,et al. Whole blood lactate kinetics in patients undergoing quantitative resuscitation for severe sepsis and septic shock[J]. Chest,2013,143(6):1548-1553. doi: 10.1378/chest.12-0878 [12] Hernandez G,Luengo C,Bruhn A,et al. When to stop septic shock resuscitation:Clues from a dynamic perfusion monitoring[J]. Ann Intensive Care,2014,4(1):1-9. [13] 伊孙邦,胡雨峰,林素涵,等. 不同时间段血乳酸水平对脓毒症院内死亡的预测价值比较:基于重症监护医学信息数据库[J]. 中华危重症医学杂志(电子版),2020,13(1):39-43. doi: 10.3877/cma.j.issn.1674-6880.2020.01.008 [14] Ryoo S M,Ahn R,Shin T G,et al. Lactate normalization within 6 hours of bundle therapy and 24 hours of delayed achievement were associated with 28-day mortality in septic shock patients[J]. PLoS One,2019,14(6):e0217857. doi: 10.1371/journal.pone.0217857 [15] Taniguchi T,Sato K,Okajima M. 1440:procalcitonin and lactate clearances as markers of improvement of severity in abdominal septic shock[J]. Critical Care Medicine,2018,46(1):704-704. [16] Nguyen H B,Loomba M,Yang J J,et al. Early lactate clearance is associated with biomarkers of inflammation,coagulation,apoptosis,organ dysfunction and mortality in severe sepsis and septic shock[J]. Journal of Inflammation,2010,7(1):6-16. doi: 10.1186/1476-9255-7-6 [17] Marty P,Roquilly A,F Vallée,et al. Lactate clearance for death prediction in severe sepsis or septic shock patients during the first 24 hours in Intensive Care Unit:an observational study[J]. Annals of Intensive Care,2013,3(1):3-9. doi: 10.1186/2110-5820-3-3 [18] Baysan M,Baroni G D,Van Boekel A M,et al. The added value of lactate and lactate clearance in prediction of in-hospital mortality in critically Ⅲ patients with sepsis[J]. Crit Care Explor,2020,2(3):e0087. doi: 10.1097/CCE.0000000000000087 [19] V Herwanto,KC Lie,S Suwarto,CM Rumende. Role of 6-hour,12-hour,and 24-hour lactate clearance in mortality of severe sepsis and septic shock patients[J]. Critical Care,2014,18(2suppl):P2. -






 下载:
下载:
 下载:
下载: