Correlation between Platelet Autophagy Related Factors and Neurological Damage and Prognosis in Patients with Aneurysmal Subarachnoid Hemorrhage
-
摘要:
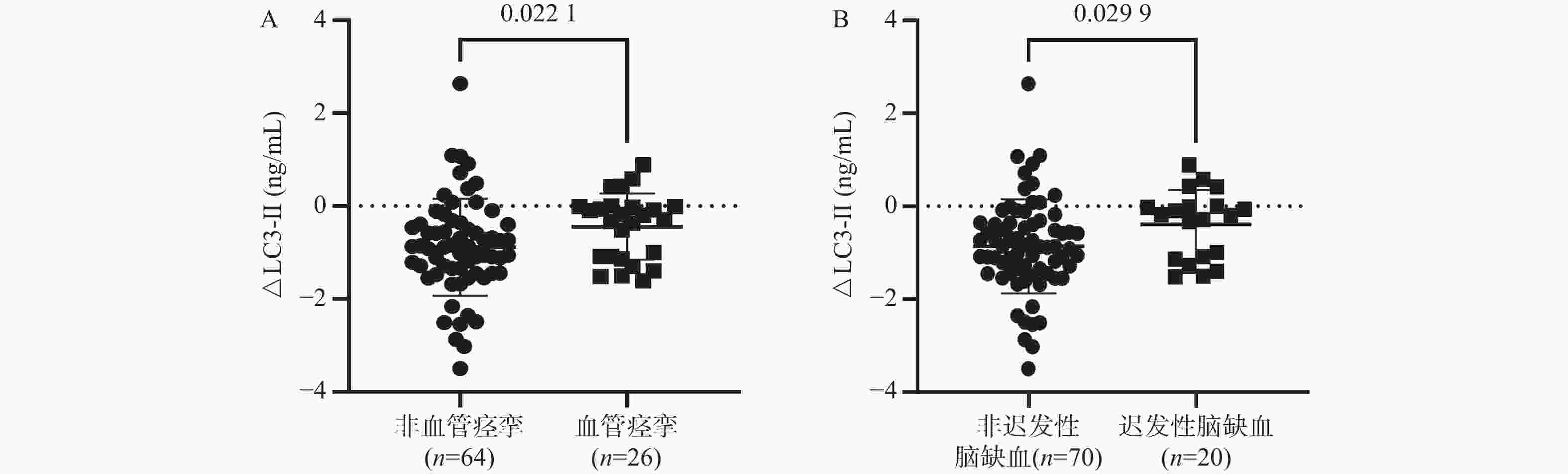
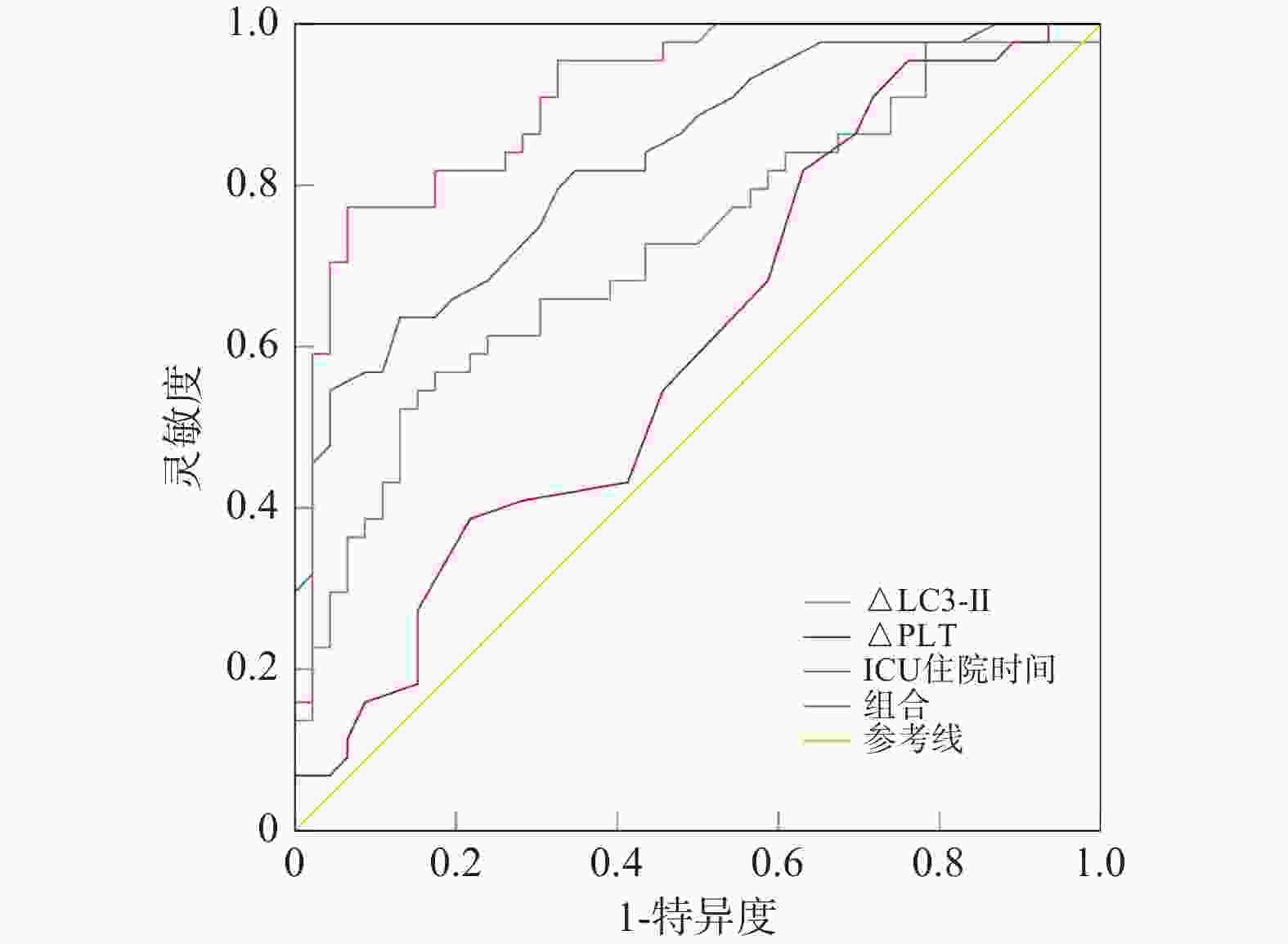
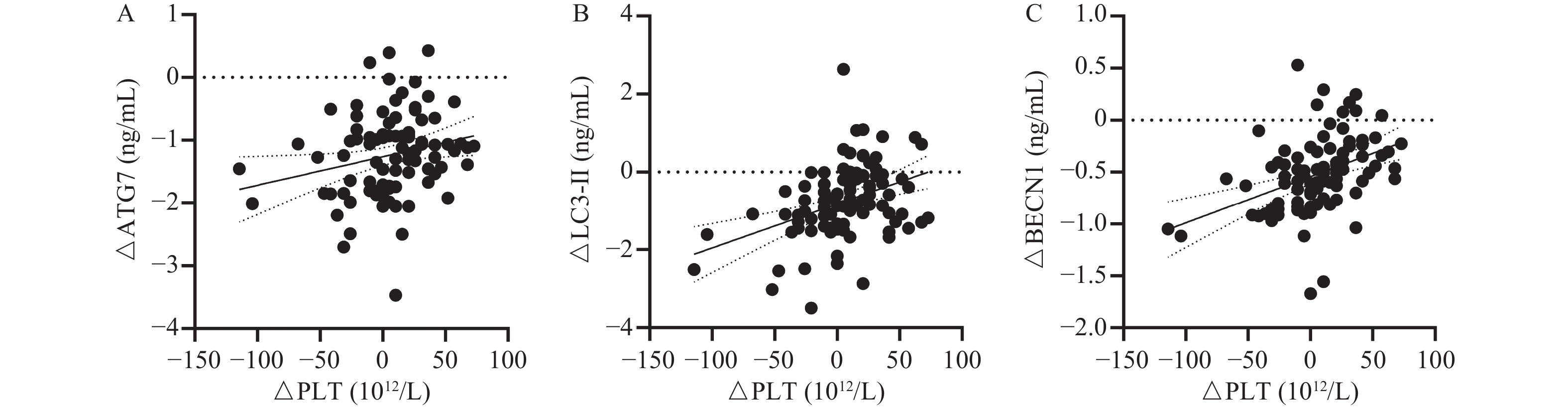
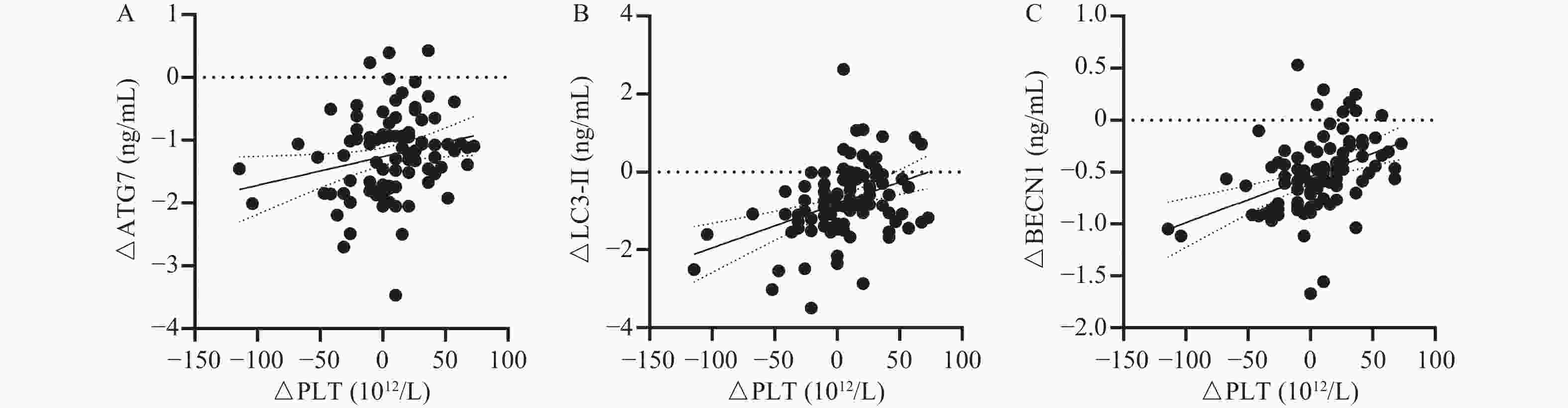
目的 探讨动脉瘤性蛛网膜下腔出血(aSAH)后血小板自噬相关因子表达参与患者神经功能损伤及预后的关系。 方法 对2020年7月至2023年3月入住西安市第三医院神经外科重症监护室的90例aSAH患者进行了回顾性分析。根据出院后3个月mRS评分,46名mRS评分为0~2分的aSAH患者被分为良好预后组,44名mRS评分为3~5分的aSAH患者被分为预后不良组。收集所有受试者的血小板,并通过酶联免疫吸附试验(ELISA)测定自噬相关蛋白7(ATG7)、苄氯素1(BECN1)、微管相关蛋白1轻链3(LC3)和sequestosome 1(p62)水平。 结果 与良好预后组相比,预后不良组机械通气时间、ICU住院时间、早期脑损伤例数、血管痉挛例数、迟发性脑缺血例数显著增加(P < 0.05)。与良好预后组相比,预后不良组ΔPLT显著降低(P < 0.05),ΔLC3-Ⅱ、ΔATG7显著增加(P < 0.05)。Spearman相关性分析显示,ΔPLT与ΔATG7、ΔLC3-Ⅱ、ΔBECN1呈显著正相关性(r=0.239、0.389、0.487,均P < 0.05)。发生血管痉挛、迟发性脑缺血的aSAH患者血小板 ΔLC3-Ⅱ高于未发生血管痉挛、迟发性脑缺血的aSAH患者(P < 0.05)。ICU住院时间(OR = 1.187,95%CI 1.045~1.349,P = 0.008),ΔPLT(OR = 0.972,95%CI 0.947~0.998,P = 0.034)和ΔLC3-Ⅱ(OR = 2.840,95%CI 1.049~7.694,P = 0.040)是aSAH患者预后不良的独立影响因素。ICU住院时间、ΔPLT和ΔLC3-Ⅱ组合预测aSAH患者预后不良的能力最大,AUC为0.921,灵敏度为86.4%,特异度为84.8%。 结论 aSAH患者治疗早期血小板计数和LC3-Ⅱ改善程度减弱可作为患者不良结局的独立影响因素。 -
关键词:
- 动脉瘤性蛛网膜下腔出血 /
- 血小板 /
- 自噬 /
- 神经功能损伤 /
- 预后
Abstract:Objective To investigate the correlation between the level of platelet autophagy related factors and the neurological impairment and prognosis of the patients with aneurysmal subarachnoid hemorrhage (aSAH). Methods From July 2020 to March 2023, 90 aSAH patients admitted to the intensive care unit of neurosurgery department of our hospital were analyzed retrospectively. Based on mRS score 3 months after discharge, patients with aSAH (n = 46, mRS 0-2) were divided into the good prognosis group, while those with mRS 3-5 (n = 44) as the poor prognosis group. Platelets of all the participants were collected, and the levels of autophagy-associated protein 7(ATG7), benzalkonium chloride 1(BECN1), microtubule-associated protein 1 light chain 3(LC3) and sequestosome 1(p62) were determined by enzyme-linked immunosorbent assay (ELISA). Results Compared with the good prognosis group, the mechanical ventilation time, ICU stay, cases of early brain injury, vasospasm and delayed cerebral ischemia in the poor prognosis group increased significantly (P < 0.05). Compared with the good prognosis group, the ΔPLT in the poor prognosis group decreased significantly (P < 0.05), and ΔLC3-Ⅱ and ΔATG7 increased significantly (P < 0.05). Spearman correlation analysis showed that ΔPLT was positively correlated with ΔATG7, ΔLC3-Ⅱ and ΔBECN1 (r = 0.239, 0.389 and 0.487, all P < 0.05). Platelet ΔLC3-Ⅱ in patients with vasospasm and delayed cerebral ischemia was higher than that in patients without vasospasm and delayed cerebral ischemia (P < 0.05). ICU stay (OR = 1.187, 95%CI = 1.045~1.349, P = 0.008), ΔPLT(OR = 0.972, 95%CI = 0.947~0.998, P = 0.034) and ΔLC3-Ⅱ (OR = 2.840, 95%CI = 1.049~7.694, P = 0.040) were independent influencing factors for the poor prognosis of aSAH patients. The combination of ICU stay, ΔPLT and ΔLC3-Ⅱ had the greatest ability to predict the poor prognosis of aSAH patients, with AUC of 0.921, sensitivity of 86.4% and specificity of 84.8%. Conclusion The decrease of platelet count and LC3-Ⅱ improvement in early treatment of aSAH patients can be regarded as the independent influencing factors of adverse outcomes. -
Key words:
- Aneurysmal subarachnoid hemorrhage /
- Platelets /
- Autophagy /
- Nerve function damage /
- Prognosis
-
表 1 患者临床基线数据的比较[n(%)/($\bar x \pm s $)]
Table 1. Comparison of Clinical Baseline Data of Patients [n(%)/($\bar x \pm s $)]
特征 预后良好组(n=46) 预后不良组(n=44) t/χ2 P 男性 14(30.4) 17(38.6) 0.670 0.413 年龄(岁) 51.48 ± 14.33 53.39 ± 10.87 0.709 0.480 机械通气时间(d) 10.43 ± 7.09 31.16 ± 17.38 7.275 <0.001* ICU住院时间(d) 15.50 ± 8.95 44.41 ± 21.94 8.119 <0.001* 高血压 15(32.6) 14(31.8) 0.006 0.936 糖尿病 0(0) 2(4.5) − 0.236 心血管疾病 6(13.0) 5(11.4) 0.059 0.808 吸烟 16(34.8) 17(38.6) 0.144 0.705 饮酒 3(6.5) 4(9.1) 0.207 0.649 动脉瘤部位 1.010 0.315 前循环 36(78.3) 38(86.4) 后循环 10(21.7) 6(13.6) 疾病评分 GCS评分 7.41 ± 3.34 6.84 ± 2.92 0.863 0.390 SAPSⅡ 38.98 ± 10.61 41.23 ± 10.55 1.008 0.316 WFNS分级 1.265 0.531 3 5(10.9) 2(4.5) 4 21(45.7) 22(50.0) 5 20(43.5) 20(45.5) 改良Fisher分级 2.215 0.330 2 2(4.3) 0(0) 3 9(19.6) 11(25.0) 4 35(76.1) 33(75.0) 治疗方法 2.700 0.259 弹簧圈栓塞 33(71.7) 27(61.4) 开颅夹闭 13(28.3) 15(34.1) 二者均有 0 2(4.5) 并发症 早期脑损伤 23(50.0) 32(72.7) 4.888 0.027* 动脉瘤再出血 1(2.2) 5(11.4) − 0.107 血管痉挛 6(13.0) 20(45.5) 11.500 0.001* 迟发性脑缺血 4(8.7) 16(36.4) 9.960 0.002* 实验数据 总胆固醇(mmol/L) 4.34 ± 0.81 4.06 ± 1.06 1.450 0.151 甘油三酯(mmol/L) 1.05 ± 0.53 1.16 ± 0.45 1.064 0.290 LDL-C(mmol/L) 2.45 ± 0.62 2.46 ± 0.85 0.033 0.974 HDL-C(mmol/L) 1.21 ± 0.38 1.09 ± 0.43 1.487 0.141 WBC(109/L) 7.10 ± 1.52 7.51 ± 1.79 0.342 0.733 PLT(1012/L) 222.70 ± 52.41 229.15 ± 53.18 0.580 0.563 *P < 0.05。 表 2 血小板计数和血小板自噬相关因子表达[($\bar x \pm s $)/M(IQR)]
Table 2. Platelet Count and Expression of Platelet Autophagy Related Factors [($\bar x \pm s $)/M(IQR)]
指标 时间点 预后良好组(n=46) 预后不良组(n=44) Z/t/χ2 P PLT(1012/L) 基线 222.70 ± 52.41 229.15 ± 53.18 1.951 0.056 治疗第5 d 235.70 ± 52.30 227.62 ± 51.11 1.461 0.150 Δ,M(IQR) 10.40(42.90) 5.20(41.60) 2.097 0.039* LC3-Ⅱ(ng/mL) 基线 8.94 ± 2.46 8.89 ± 2.57 0.064 0.949 治疗第5 d 7.66 ± 3.00 7.37 ± 2.18 0.433 0.667 Δ,M(IQR) −0.88(0.88) −0.38(1.35) 2.123 0.034* ATG7(ng/mL) 基线 3.39 ± 0.72 3.21 ± 0.61 1.261 0.211 治疗第5 d 2.01 ± 0.55 2.13 ± 0.64 0.953 0.343 Δ,M(IQR) −1.33(0.80) −1.02(1.06) 2.317 0.021* p62(ng/mL) 基线 3.26 ± 2.44 3.17 ± 1.99 0.181 0.857 治疗第5 d 3.71 ± 2.36 3.44 ± 2.09 0.574 0.567 Δ,M(IQR) 0.59(2.42) −0.01(2.44) 0.557 0.578 BECN1(ng/mL) 基线 2.27 ± 0.46 2.18 ± 0.28 1.227 0.224 治疗第5 d 1.70 ± 0.34 1.72 ± 0.35 0.360 0.719 Δ,M(IQR) −0.59(0.43) −0.45(0.38) 1.857 0.063 注:Δ=治疗第5天水平−基线水平,*P < 0.05。 表 3 aSAH后血小板计数的早期变化和ΔATG7、ΔLC3-Ⅱ、ΔBECN1、Δp62表达的相关性分析
Table 3. Correlation analysis between early changes of platelet count and expression of ΔATG7, ΔLC3-Ⅱ, ΔBECN1, Δp62 after aSAH
指标 ΔATG7 ΔLC3-Ⅱ ΔBECN1 Δp62 ΔPLT r 0.239 0.389 0.487 0.027 P 0.023* <0.001* <0.001* 0.802 n 90 90 90 90 *P < 0.05。 表 4 多元logistic回归分析aSAH患者预后不良的预测因素
Table 4. Multivariate logistic Regression Analysis of Predictors of Poor Prognosis in asah Patients
指标 B 标准误差 Wald P OR 95%CI 机械通气时间 −0.039 0.073 0.287 0.592 0.962 0.834~1.109 ICU住院时间 0.172 0.065 6.987 0.008* 1.187 1.045~1.349 早期脑损伤 1.691 0.988 2.928 0.087 5.427 0.782~37.664 血管痉挛 −1.281 1.590 0.650 0.420 0.278 0.012~6.261 迟发性脑缺血 3.063 1.959 2.443 0.118 21.381 0.459~995.235 ΔPLT −0.028 0.013 4.475 0.034* 0.972 0.947~0.998 ΔLC3-Ⅱ 1.044 0.508 4.216 0.040* 2.840 1.049~7.694 ΔATG7 0.636 0.637 0.997 0.318 1.890 0.542~6.592 常量 −3.104 1.365 5.173 0.023* 0.045 表 5 ROC曲线分析ICU住院时间、ΔPLT和ΔLC3-Ⅱ及三者组合预测aSAH患者预后不良的能力
Table 5. ROC curve analysis of ICU stay,ΔPLT and ΔLC3-Ⅱ and their combination to predict the poor prognosis of aSAH patients
变量 区域 截止值 灵敏度% 特异度% P 95%CI 下限 上限 ΔLC3-Ⅱ 0.723 −0.431 56.8 82.6 <0.001 0.617 0.828 ΔPLT 0.602 39 95.5 23.9 0.096 0.485 0.719 ICU住院时间 0.831 25.5 63.6 87.0 <0.001 0.749 0.913 组合 0.921 − 86.4 84.8 <0.001 0.911 0.990 -
[1] Robba C,Busl K M,Claassen J,et al. Contemporary management of aneurysmal subarachnoid haemorrhage. An update for the intensivist[J]. Intensive Care Med,2024,50(5):646-664. doi: 10.1007/s00134-024-07387-7 [2] 卢荣加,周绍福,伊鹏. 3 d-Slicer血肿量预测aSAH后sCVS的临床价值研究[J]. 中华神经医学杂志,2022,21(1):41-46. doi: 10.3760/cma.j.cn115354-20211005-00642 [3] Chaudhry S R,Kahlert U D,Kinfe T M,et al. Differential polarization and activation dynamics of systemic T helper cell subsets after aneurysmal subarachnoid hemorrhage (SAH) and during post-SAH complications[J]. Sci Rep,2021,11(1):14226-14236. doi: 10.1038/s41598-021-92873-x [4] Muhammad S,Hänggi D. Inflammation and anti-inflammatory targets after aneurysmal subarachnoid hemorrhage[J]. Int J Mol Sci,2021,22(14):7355-7359. doi: 10.3390/ijms22147355 [5] Lyu X,Xiong Y,Jiang L,et al. The independent predictive role of platelet to white blood cell ratio on all-cause mortality: A 7-year nationwide follow-up study in China[J]. Int J Surg,2024,110(9):5923-5925. doi: 10.1097/JS9.0000000000001688 [6] Valero P,Cornejo M,Fuentes G,et al. Platelets and endothelial dysfunction in gestational diabetes mellitus[J]. Acta Physiol,2023,237(4):e13940. doi: 10.1111/apha.13940 [7] Zhou Y,Wang K,Li R,et al. Dynamic changes of platelets before and after surgery predict the prognosis of patients with aneurysmal subarachnoid hemorrhage[J]. Heliyon,2024,10(18):e37706. doi: 10.1016/j.heliyon.2024.e37706 [8] Chardon N,Nourredine M,Ledochowski S,et al. Trajectory of mean platelet volume changes after aneurysmal subarachnoid hemorrhage in patients with or without delayed cerebral ischemia[J]. Sci Rep,2024,14(1):25122. doi: 10.1038/s41598-024-75587-8 [9] Nguyen A,Nguyen A,Hsu T I,et al. Neutrophil to lymphocyte ratio as a predictor of postoperative outcomes in traumatic brain injury: A systematic review and meta-analysis[J]. Diseases,2023,11(1):51. doi: 10.3390/diseases11010051 [10] Yang H X,Li Y J,He Y L,et al. Hydrogen Sulfide Promotes Platelet Autophagy via PDGFR-α/PI3K/Akt Signaling in Cirrhotic Thrombocytopenia[J]. J Clin Transl Hepatol,2024,12(7):625-633. [11] 中华医学会神经病学分会,中华医学会神经病学分会脑血管病学组,中华医学会神经病学分会神经血管介入协作组. 中国蛛网膜下腔出血诊治指南2019[J]. 中国神经科杂志,2019,52(12):1006-1021. [12] 中华医学会神经病学分会,中华医学会神经病学分会脑血管病学组,中华医学会神经病学分会神经血管介入协作组. 中国蛛网膜下腔出血诊治指南2019[J]. 中华神经科杂志,2019,52(12): 1006-1021.Schmidt T P,Weiss M,Hoellig A,et al. Revisiting the timeline of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage: Toward a temporal risk profile[J]. Neurocrit Care,2022,37(3): 735-743. [13] Sun D,Huo X,Jia B,et al. The safety and efficacy of endovascular treatment in acute ischemic stroke patients caused by large-vessel occlusion with different etiologies of stroke: data from ANGEL-ACT registry[J]. Neurotherapeutics,2022,19(2):501-512. doi: 10.1007/s13311-022-01189-9 [14] Monsour M,Croci D M,Grüter B E,et al. Cerebral aneurysm and interleukin-6: A key player in aneurysm generation and rupture or just one of the multiple factors?[J]. Transl Stroke Res,2023,14(5):631-639. doi: 10.1007/s12975-022-01079-4 [15] Bolton W S,Gharial P K,Akhunbay-Fudge C,et al. Day 2 neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios for prediction of delayed cerebral ischemia in subarachnoid hemorrhage[J]. Neurosurg Focus,2022,52(3):E4. doi: 10.3171/2021.12.FOCUS21642 [16] Liao B,Xu Q,Lu P,et al. The prognostic value of systemic immune-inflammation index in patients with aneurysmal subarachnoid hemorrhage: A systematic review[J]. Neurosurg Rev,2023,46(1):219. doi: 10.1007/s10143-023-02133-x [17] Zhang W,Xiang C,Liu B,et al. The value of systemic immune inflammation index,white blood cell to platelet ratio,and homocysteine in predicting the instability of small saccular intracranial aneurysms[J]. Sci Rep,2024,14(1):24312. doi: 10.1038/s41598-024-74870-y [18] Ludwig N,Hilger A,Zarbock A,et al. Platelets at the crossroads of pro-inflammatory and resolution pathways during inflammation[J]. Cells,2022,11(12):1957. doi: 10.3390/cells11121957 [19] Naraoka M,Matsuda N,Shimamura N,et al. Role of microcirculatory impairment in delayed cerebral ischemia and outcome after aneurysmal subarachnoid hemorrhage[J]. J Cereb Blood Flow Metab,2022,42(1):186-196. doi: 10.1177/0271678X211045446 [20] Dienel A,Kumar T P,Blackburn S L,et al. Role of platelets in the pathogenesis of delayed injury after subarachnoid hemorrhage[J]. J Cereb Blood Flow Metab,2021,41(11):2820-2830. doi: 10.1177/0271678X211020865 [21] Rzepliński R,Kostyra K,Skadorwa T,et al. Acute platelet response to aneurysmal subarachnoid hemorrhage depends on severity and distribution of bleeding: An observational cohort study[J]. Neurosurg Rev,2021,44(5):2647-2658. doi: 10.1007/s10143-020-01444-7 [22] 姜江,丁育红,贾慧,等. 血小板受体C型凝集素样受体2在巨核细胞自噬中的作用[J]. 南京医科大学学报: 自然科学版,2022,42(6):815-820. [23] Lee T Y,Lu W J,Changou C A,et al. Platelet autophagic machinery involved in thrombosis through a novel linkage of AMPK-MTOR to sphingolipid metabolism[J]. Autophagy,2021,17(12):4141-4158. doi: 10.1080/15548627.2021.1904495 [24] Li X,Ma Y,Liu C,et al. Platelet membrane‐derived microparticles may be biomarkers in patients with hepatocellular carcinoma and can promote the invasion and metastasis of hepatoma carcinoma cells[J]. Transfusion,2023,63(10):1821-1831. doi: 10.1111/trf.17499 [25] Zhao X,Zhao Y,Ding Y,et al. Autophagy Ameliorates Reactive Oxygen Species‐Induced Platelet Storage Lesions[J]. Oxid Med Cell Longev,2022(1):1898844. -





 下载:
下载: