Changes in Expression Levels and Clinical Significance of Park7 and P2X7R in the Serum of Patients with Acute Myocardial Infarction
-
摘要:
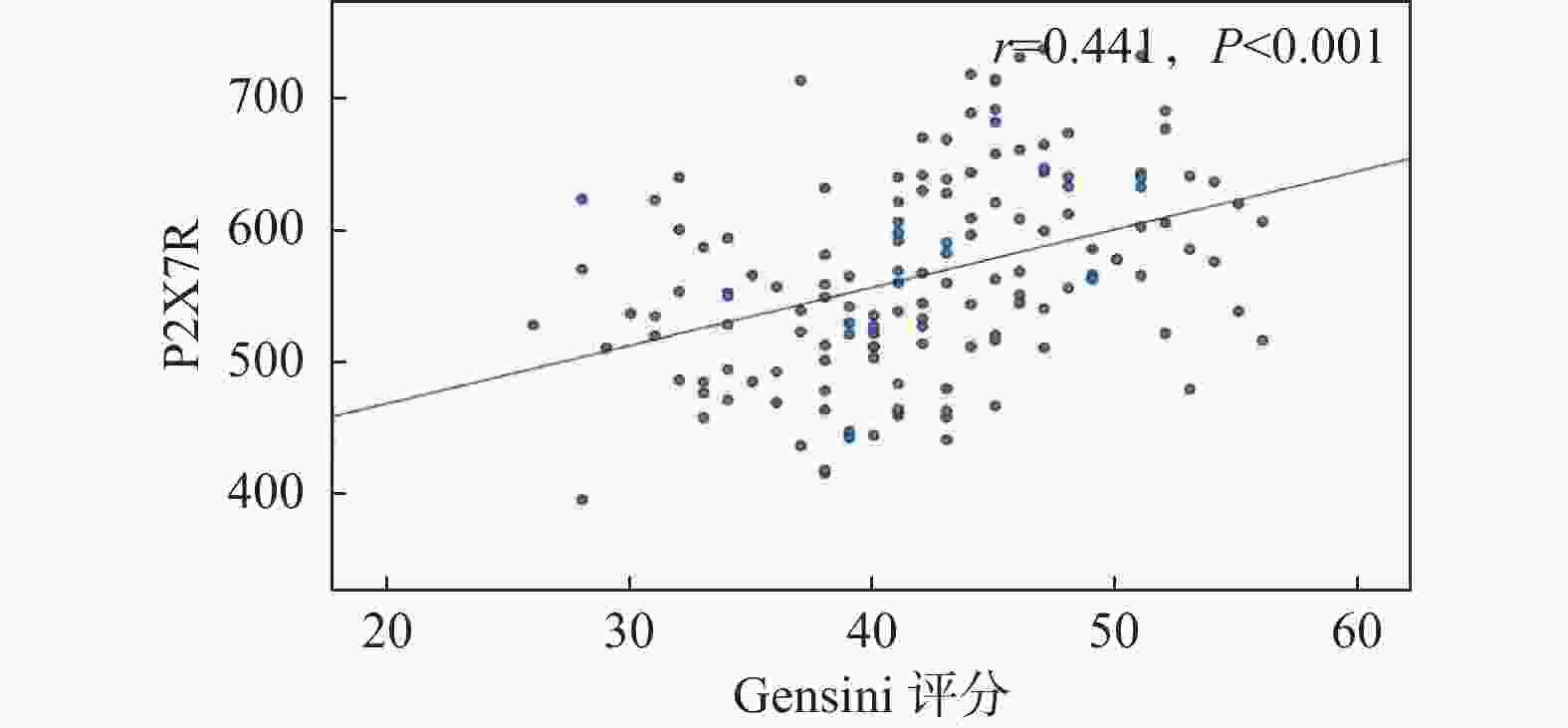
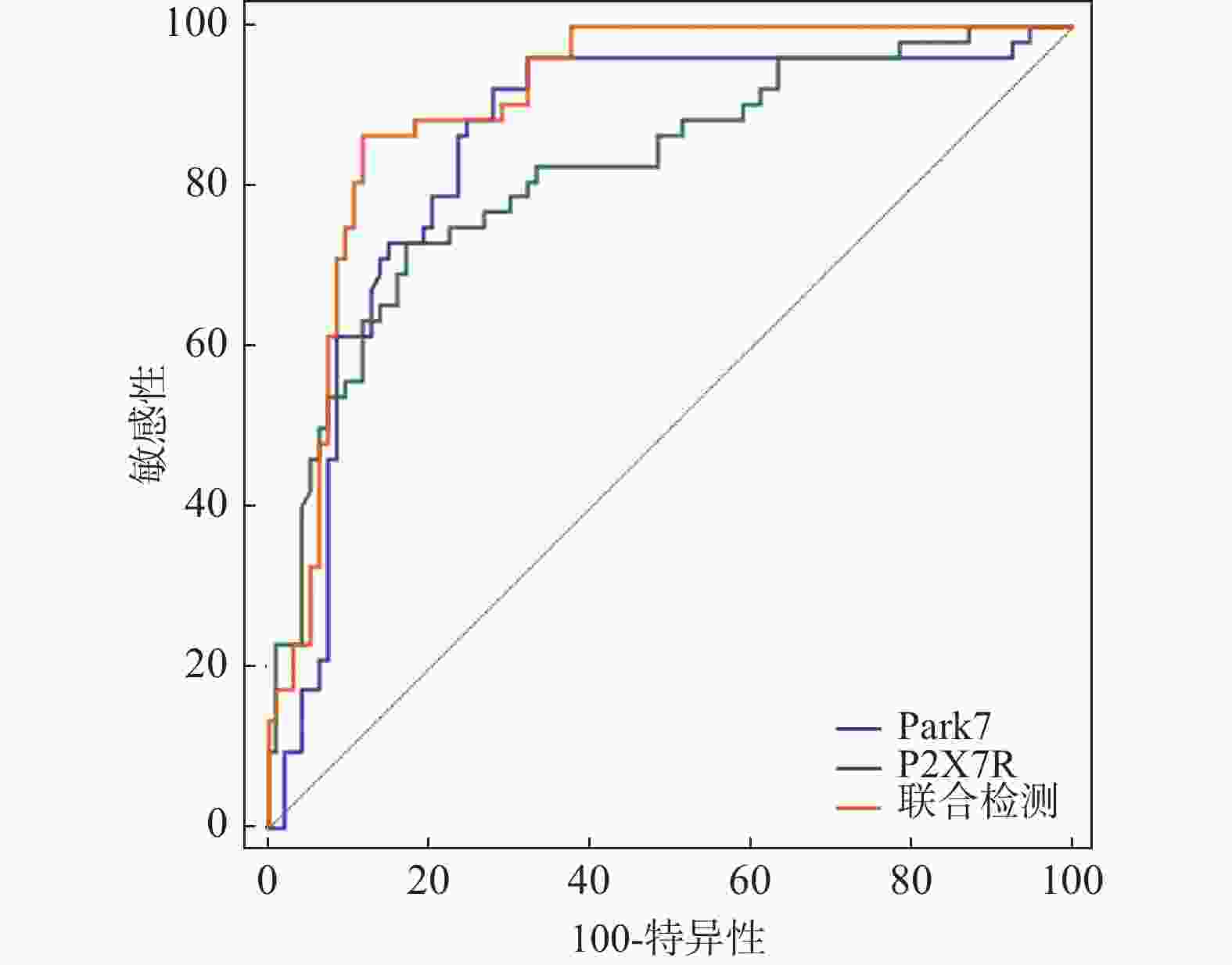
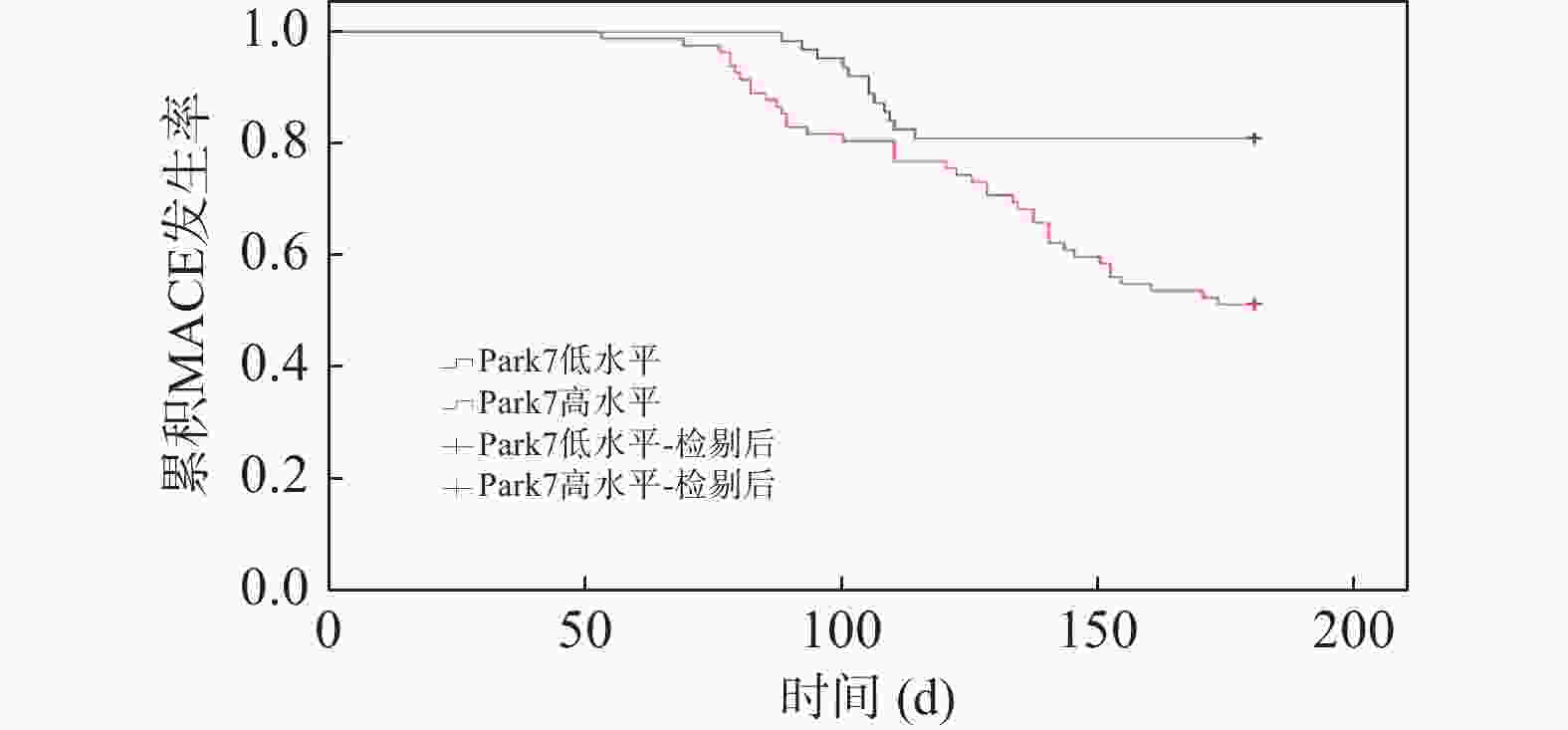
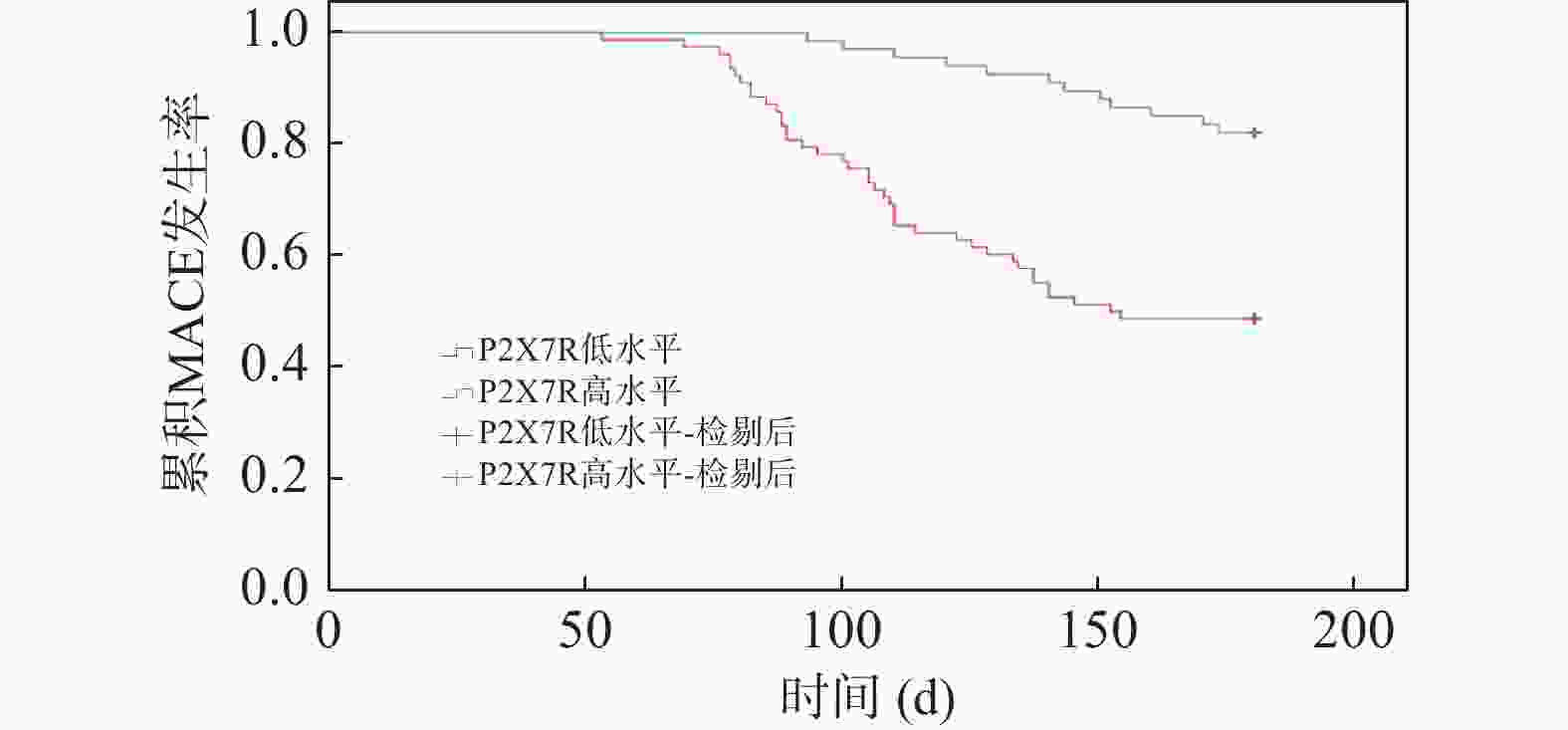
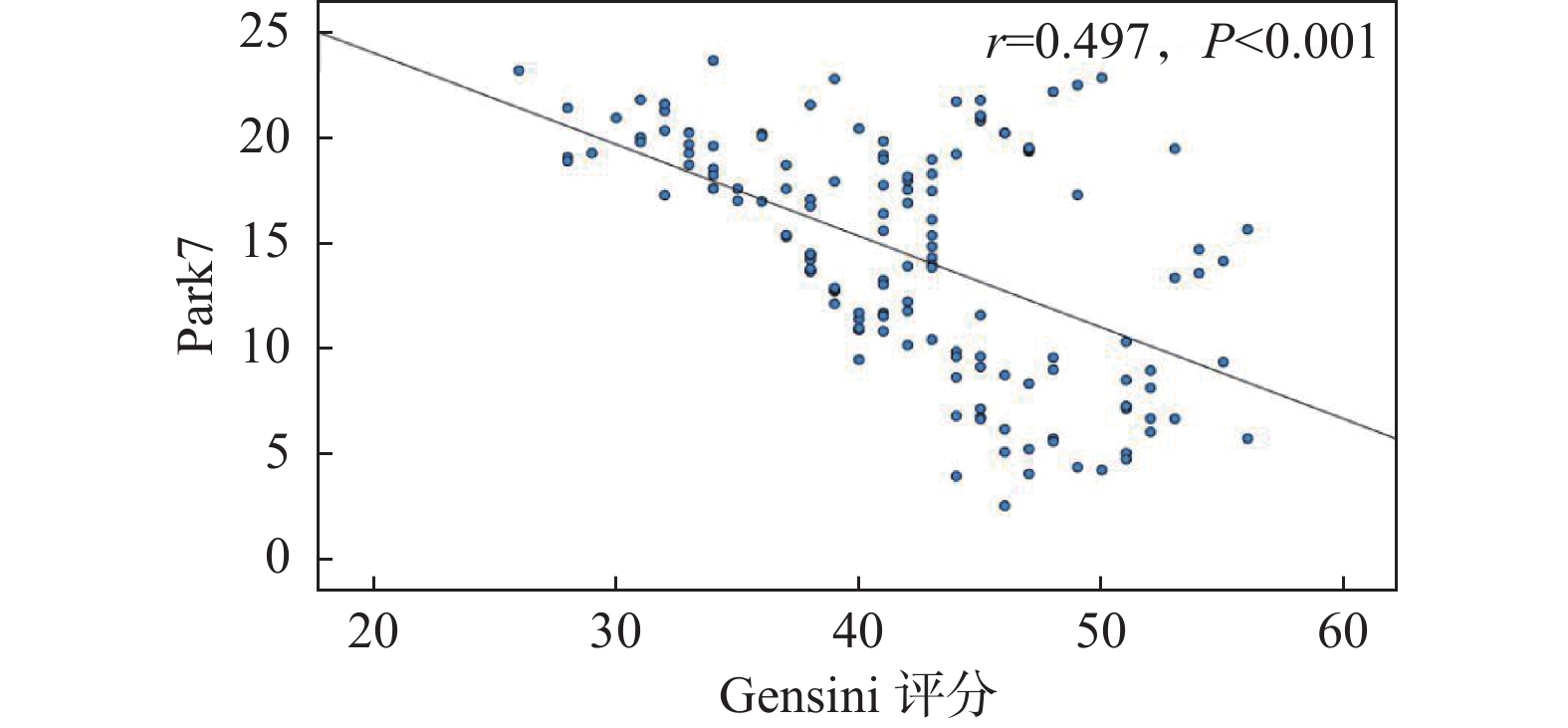
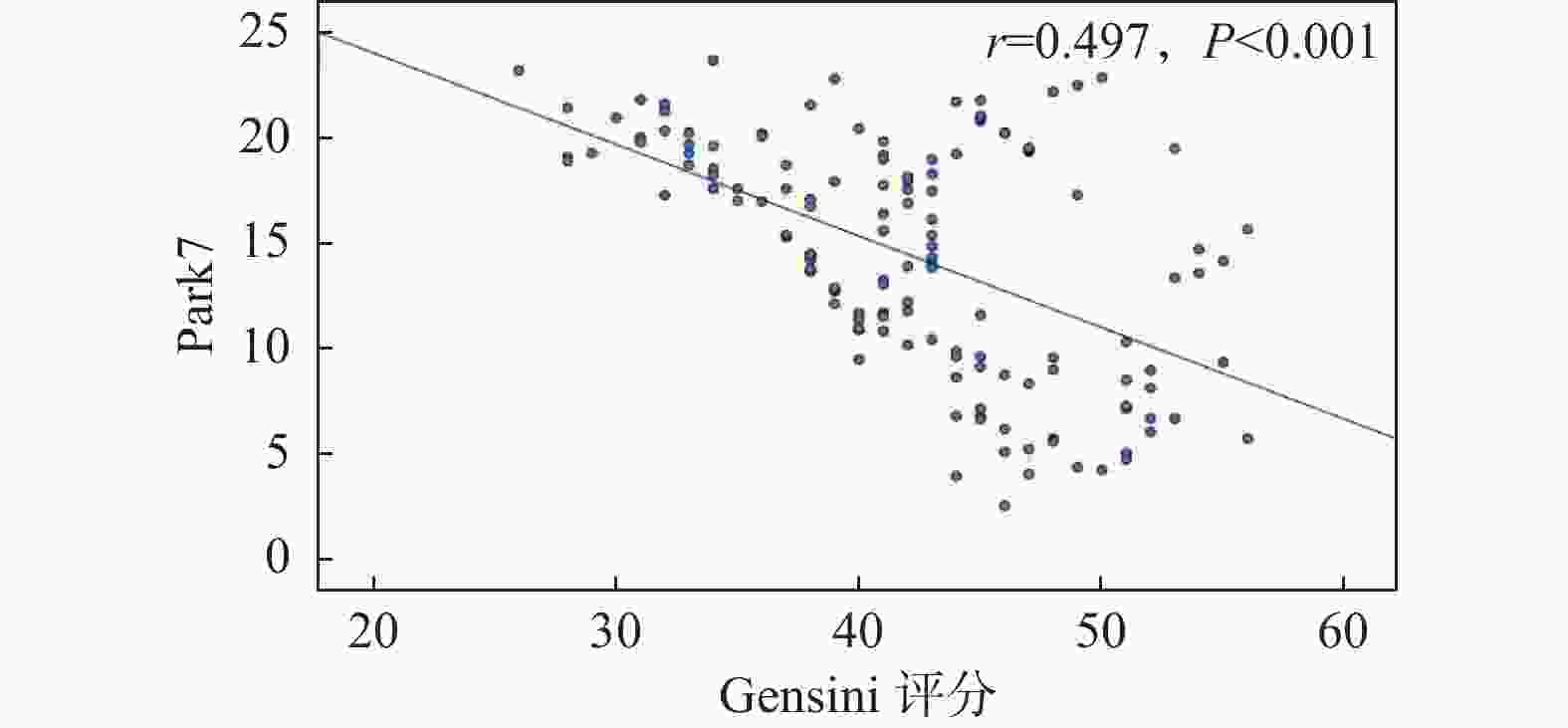
目的 探讨急性心肌梗死(AMI)患者血清中帕金森病蛋白7(Park7)、P2X7嘌呤能受体(P2X7R)的表达水平变化及其临床意义。 方法 招募2021年2月-2023年5月在承德市荣军优抚医院收治的AMI患者145例作为AMI组,根据Gensini评分评估冠脉病变严重程度,分为轻度组(≤30分,68例)、中度组(30~59分,42例)、重度组(≥60分,35例);同期招募在该院体检的健康志愿者120例作为对照组。ELISA法测定血清中Park7、P2X7R表达水平;Spearman法分析AMI患者血清Park7、P2X7R水平与Gensini评分的相关性;ROC曲线评价血清Park7、P2X7R对MACE发生的预测价值;绘制Kaplan-Meier曲线分析不同Park7和P2X7R表达患者的累积MACE发生率;Cox回归分析AMI患者发生MACE的影响因素。 结果 与对照组相比,AMI组TC、TG、LDL-C、IL-6、CTnI、CK-MB、BNP及血清P2X7R水平显著升高(P < 0.05),血清HDL-C、Park7水平显著降低(P < 0.05),且不同严重程度患者血清P2X7R、Park7水平之间差异有统计学意义(P < 0.05)。AMI患者血清Park7与Gensini评分呈负相关(r = -0.497,P < 0.05),P2X7R水平与Gensini评分呈正相关(r = 0.441,P < 0.05)。MACE组患者血清Park7水平显著低于非MACE组,P2X7R水平显著高于非MACE组(P < 0.05)。血清Park7、P2X7R以及联合预测AMI患者发生MACE的AUC分别为0.851、0.820、0.905,联合预测效果更佳(Z二者联合-Park7=2.324、Z二者联合-P2X7R=2.538,P<0.05)。Park7低表达患者6个月累积MACE发生率(51.22%)低于Park7高表达患者(80.95%)(Log Rank χ2=12.178,P < 0.001);P2X7R低表达患者6个月累积MACE发生率(82.09%)高于P2X7R高表达患者(48.72%)(Log Rank χ2=20.233,P < 0.001)。CTnI、CK-MB、BNP、Park7、P2X7R是AMI患者发生MACE的影响因素(P < 0.05)。 结论 AMI患者血清Park7水平下调,P2X7R水平上调,与病情严重程度密切相关,二者联合对AMI患者发生MACE具有较高的预测价值。 Abstract:Objective To investigate the changes in expression levels of Parkinson's disease protein 7 (Park7) and P2X7R purinergic receptor (P2X7R) in the serum of patients with acute myocardial infarction (AMI) and their clinical significance. Methods A total of 145 AMI patients admitted to Chengde Veterans Hospital between February 2021 and May 2023 were recruited as the AMI group. According to the Gensini score for assessing the severity of coronary lesions, they were subdivided into a mild group (≤ 30 points, 68 cases), a moderate group (30-59 points, 42 cases), and a severe group (≥ 60 points, 35 cases). Additionally, 120 healthy volunteers undergoing physical examinations at the same hospital were recruited as the control group. ELISA method was used to measure serum levels of Park7 and P2X7R. Correlation between serum Park7 and P2X7R levels and Gensini score in AMI patients was analysed by Spearman's method. ROC curves were used to evaluate the predictive value of serum Park7 and P2X7R for the occurrence of MACE. Plot Kaplan-Meier curves were plotted to analyze the cumulative MACE incidence rates in patients with different Park7 and P2X7R expression levels. Cox regression analysis was used to identify risk factors for MACE occurrence in AMI patients. Results Compared with the control group, the AMI group showed significantly increased levels of TC, TG, LDL-C, IL-6, CTnI, CK-MB, BNP, and serum P2X7R (P < 0.05), and significantly decreased levels of serum HDL-C and Park7 (P < 0.05). Furthermore, statistically significant differences were observed in serum P2X7R and Park7 levels among patients with different severity levels (P < 0.05). There was a negative correlation between serum Park7 and Gensini score in AMI patients (r = -0.497, P < 0.05), while a positive correlation between P2X7R level and Gensini score (r = 0.441, P < 0.05). Serum Park7 level in the MACE group was significantly lower than that in the non MACE group, while the P2X7Rlevel was significantly higher (P < 0.05). The AUCs for serum Park7, P2X7R, and their combination in predicting MACE in AMI patients was 0.851, 0.820, and 0.905, respectively, with the combined prediction demonstrating superior performance (Zcombination - Park7=2.324, Zcombination - P2X7R=2.538, P < 0.05). The 6-month cumulative MACE incidence was lower in patients with low Park7 expression (51.22%) than in those with high Park7 expression (80.95%) (Log Rank χ2=12.178, P < 0.001); conversely, the 6-month cumulative MACE incidence was higher in patients with low P2X7R expression (82.09%) than in those with high P2X7R expression (48.72%) (Log Rank χ2=20.233, P < 0.001). CTnI, CK-MB, BNP, Park7, and P2X7R were identified as influencing factors for MACE in AMI patients (P < 0.05). Conclusion Serum Park7 level is downregulated while P2X7Rlevel is upregulated in AMI patients, both closely related to the severity of the disease. The combination of the two has high predictive value for the occurrence of MACE in AMI patients. -
表 1 一般临床资料比较[n(%)/($\bar x \pm s $)]
Table 1. Comparison of general clinical data[n(%)/($\bar x \pm s $)]
项目 对照组(n = 120) AMI组(n = 145) t/χ2 P 年龄(岁) 64.12 ± 6.57 65.47 ± 7.35 1.561 0.120 性别(男/女) 64/56 63/82 2.571 0.109 吸烟史 47(39.17) 66(45.52) 1.083 0.298 饮酒史 49(40.83) 75(51.72) 3.128 0.077 糖尿病 20(16.67) 31(21.38) 0.938 0.333 高血压 18(15.00) 33(22.76) 2.543 0.111 冠心病 25(20.83) 38(26.21) 1.046 0.306 心率(次/min) 65.59 ± 7.13 67.18 ± 7.25 1.790 0.075 TC(mmol/L) 4.82 ± 0.75 5.96 ± 0.92 10.902 <0.001* TG(mmol/L) 1.65 ± 0.58 2.31 ± 0.74 7.954 <0.001* HDL-C(mmol/L) 1.20 ± 0.23 0.95 ± 0.18 9.923 <0.001* LDL-C(mmol/L) 2.95 ± 0.61 3.47 ± 0.76 6.053 <0.001* IL-6(pg/mL) 5.23 ± 1.87 8.65 ± 2.32 13.022 <0.001* cTnI(ng/mL) 0.03 ± 0.01 0.51 ± 0.16 32.800 <0.001* CK-MB(U/L) 18.11 ± 4.96 44.98 ± 13.01 21.370 <0.001* BNP(ng/L) 68.76 ± 15.08 135.41 ± 39.89 17.304 <0.001* Park7(μg/L) 32.58 ± 9.44 14.21 ± 4.13 21.123 <0.001* P2X7R(pg/mL) 324.54 ± 53.16 571.68 ± 88.12 26.929 <0.001* *P < 0.05。 表 2 不同严重程度AMI患者血清Park7、P2X7R水平比较($\bar x \pm s $)
Table 2. Comparison of serum Park7 and P2X7R levels in AMI patients with different severity levels ($\bar x \pm s $)
组别 n Park7(μg/L) P2X7R(pg/mL) Gensini评分(分) 轻度组 68 19.11 ± 2.35 526.39 ± 57.47 25.14 ± 6.65 中度组 42 12.35 ± 2.11a 587.45 ± 60.01a 39.89 ± 7.07 重度组 35 6.93 ± 2.07ab 640.75 ± 65.37ab 77.38 ± 7.69 F - 369.417 43.755 640.227 P - <0.001* <0.001* <0.001* *P < 0.05;与轻度组比较,aP < 0.05;与中度组比较,bP < 0.05。 表 3 MACE组和非MACE组血清Park7、P2X7R水平比较($\bar x \pm s $)
Table 3. Comparison of serum Park7 and P2X7R levels between MACE and Non-MACE groups ($\bar x \pm s $)
组别 n Park7(μg/L) P2X7R(pg/mL) 非MACE组 93 18.56 ± 4.14 543.18 ± 54.96 MACE组 52 6.43 ± 2.07 622.65 ± 62.78 t - 19.770 7.931 P - <0.001* <0.001* *P < 0.05。 表 4 血清Park7、P2X7R水平对AMI患者发生MACE的预测价值
Table 4. Predictive value of serum Park7 and P2X7R levels for MACE in patients with AMI
变量 AUC 截断值 95%CI 敏感性(%) 特异性(%) Youden指数 Park7 0.851 14.78 μg/L 0.782~0.904 92.31 72.04 0.644 P2X7R 0.820 587.42 pg/mL 0.748~0.879 73.08 82.80 0.559 联合检测 0.905 - 0.846~0.948 86.54 88.17 0.747 表 5 Cox回归分析AMI患者发生MACE的影响因素
Table 5. Cox regression analysis of factors influencing MACE in AMI patients
自变量 单因素分析 多因素分析 SE OR(95%CI) P SE OR(95%CI) P 年龄 0.157 1.246(0.916~1.695) 0.161 - - - 性别 0.138 1.071(0.817~1.404) 0.619 - - 吸烟史 0.255 1.296(0.786~2.136) 0.309 - - 饮酒史 0.319 1.277(0.683~2.386) 0.443 - - 糖尿病 0.271 1.056(0.621~1.796) 0.841 - - - 高血压 0.152 1.316(0.977~1.773) 0.071 - - - 冠心病 0.133 1.024(0.789~1.329) 0.858 - - - 心率 0.344 1.899(0.968~3.727) 0.062 - - - TC 0.206 1.335(0.892~1.999) 0.161 - - - TG 0.171 1.205(0.862~1.685) 0.275 - - - HDL-C 0.087 0.862(0.727~1.022) 0.088 - - - LDL-C 0.143 1.299(0.981~1.719) 0.067 - - - IL-6 0.240 1.574(0.983~2.519) 0.059 - - - 他汀类药物 0.158 1.211(0.888~1.651) 0.226 - - - P2X7R拮抗剂 0.116 1.215(0.968~1.525) 0.093 - - - 抗血小板药物 0.184 1.341(0.930~1.935) 0.117 - - - ACEI/ARB 0.214 1.450(0.953~2.206) 0.083 - - - CTnI 0.145 1.377(1.036~1.830) 0.027* 0.171 1.469(1.051~2.054) 0.025* CK-MB 0.151 1.499(1.115~2.015) 0.007* 0.106 1.281(1.041~1.577) 0.019* BNP 0.171 1.597(1.142~2.233) 0.006* 0.125 1.514(1.185~1.934) <0.001* Park7 0.059 0.824(0.734~0.925) 0.001* 0.093 0.781(0.651~0.937) 0.008* P2X7R 0.299 2.176(1.211~3.910) 0.009* 1.197 2.085(1.417~3.068) <0.001* *P < 0.05。 -
[1] Krittanawong C, Khawaja M, Tamis-Holland J E, et al. Acute myocardial infarction: Etiologies and mimickers in young patients[J]. J Am Heart Assoc, 2023, 12(18): e029971. doi: 10.1161/JAHA.123.029971 [2] Gallinat A, Mendieta G, Vilahur G, et al. DJ-1 administration exerts cardioprotection in a mouse model of acute myocardial infarction[J]. Front Pharmacol, 2022, 13: 1002755. doi: 10.3389/fphar.2022.1002755 [3] Pan G, Yang S, Han X, et al. Parkinson’s disease protein 7 protected against oxidative stress of myocardial infarction direct through p47phox and nicotinamide adenine dinucleotide phosphate oxidase 4[J]. Hum Exp Toxicol, 2022, 41: 09603271221124099. [4] Bin Dayel A, Alonazi A, Alshammari T, et al. P2X7 purinergic receptor: A potential target in heart diseases (Review)[J]. Mol Med Rep, 2023, 27(3): 74. doi: 10.3892/mmr.2023.12961 [5] Shi X X, Zheng K C, Shan P R, et al. Elevated circulating level of P2X7 receptor is related to severity of coronary artery stenosis and prognosis of acute myocardial infarction[J]. Cardiol J, 2021, 28(3): 453-459. doi: 10.5603/CJ.a2020.0074 [6] 国家心血管病中心. 《中国心血管健康与疾病报告》2020[J]. 心肺血管病杂志, 2021, 40(10): 1005-1009. [7] 孔海英, 杨广龙, 尹琼, 等. 冠状动脉粥样硬化性心脏病病人斑块稳定性及Gensini评分与Lp(a)水平的相关性[J]. 中西医结合心脑血管病杂志, 2022, 20(2): 304-307. [8] 中国医师协会中西医结合医师分会, 中国中西医结合学会心血管病专业委员会, 中国中西医结合学会重症医学专业委员会, 等. 急性心肌梗死中西医结合诊疗指南[J]. 中国中西医结合杂志, 2018, 38(3): 272-284. [9] Saito Y, Oyama K, Tsujita K, et al. Treatment strategies of acute myocardial infarction: Updates on revascularization, pharmacological therapy, and beyond[J]. J Cardiol, 2023, 81(2): 168-178. doi: 10.1016/j.jjcc.2022.07.003 [10] Sun M E, Zheng Q. The tale of DJ-1 (PARK7): A Swiss army knife in biomedical and psychological research[J]. Int J Mol Sci, 2023, 24(8): 7409. doi: 10.3390/ijms24087409 [11] Tsoporis J N, Drosatos I A, Gupta S, et al. Cytoprotective mechanisms of DJ-1: Implications in cardiac pathophysiology[J]. Molecules, 2021, 26(13): 3795. doi: 10.3390/molecules26133795 [12] Pan J, Xiong W, Zhang A, et al. The imbalance of p53-Park7 signaling axis induces iron homeostasis dysfunction in doxorubicin-challenged cardiomyocytes[J]. Adv Sci (Weinh), 2023, 10(15): e2206007. doi: 10.1002/advs.202206007 [13] Zhao X Y, Ren J M, Liu H R, et al. DJ-1 activates the AMPK/mTOR pathway by binding RACK1 to induce autophagy and protect the myocardium from ischemia/hypoxia injury[J]. Biochem Biophys Res Commun, 2022, 637: 276-285. doi: 10.1016/j.bbrc.2022.10.100 [14] Lu Y, Zhang J, Han B, et al. Extracellular vesicles DJ-1 derived from hypoxia-conditioned hMSCs alleviate cardiac hypertrophy by suppressing mitochondria dysfunction and preventing ATRAP degradation[J]. Pharmacol Res, 2023, 187: 106607. doi: 10.1016/j.phrs.2022.106607 [15] Pantner Y, Polavarapu R, Chin L S, et al. DJ-1 attenuates the glycation of mitochondrial complex I and complex III in the post-ischemic heart[J]. Sci Rep, 2021, 11(1): 19408. doi: 10.1038/s41598-021-98722-1 [16] Chen R, Li W, Qiu Z, et al. Ischemic postconditioning-mediated DJ-1 activation mitigate intestinal mucosa injury induced by myocardial ischemia reperfusion in rats through Keap1/Nrf2 pathway[J]. Front Mol Biosci, 2021, 8: 655619. doi: 10.3389/fmolb.2021.655619 [17] Tsirebolos G, Tsoporis J N, Drosatos I A, et al. Emerging markers of inflammation and oxidative stress as potential predictors of coronary artery disease[J]. Int J Cardiol, 2023, 376: 127-133. doi: 10.1016/j.ijcard.2023.02.005 [18] Hirayama Y, Anzai N, Kinouchi H, et al. P2X7 receptors in astrocytes: A switch for ischemic tolerance[J]. Molecules, 2022, 27(12): 3655. doi: 10.3390/molecules27123655 [19] Huang S, Wang W, Li L, et al. P2X7 receptor deficiency ameliorates STZ-induced cardiac damage and remodeling through PKCβ and ERK[J]. Front Cell Dev Biol, 2021, 9: 692028. doi: 10.3389/fcell.2021.692028 [20] Cheng W, Sun Y, Wu Q, et al. Paraventricular nucleus P2X7 receptors aggravate acute myocardial infarction injury via ROS-induced vasopressin-V1b activation in rats[J]. Neurosci Bull, 2021, 37(5): 641-656. doi: 10.1007/s12264-021-00641-8 -





 下载:
下载: