Clinical Efficacy of Short-term Spinal Cord Stimulation and Dorsal Root Ganglion Stimulation in the Treatment of Herpes Zoster-related Neuralgia and Improvement of Sleep Quality
-
摘要:
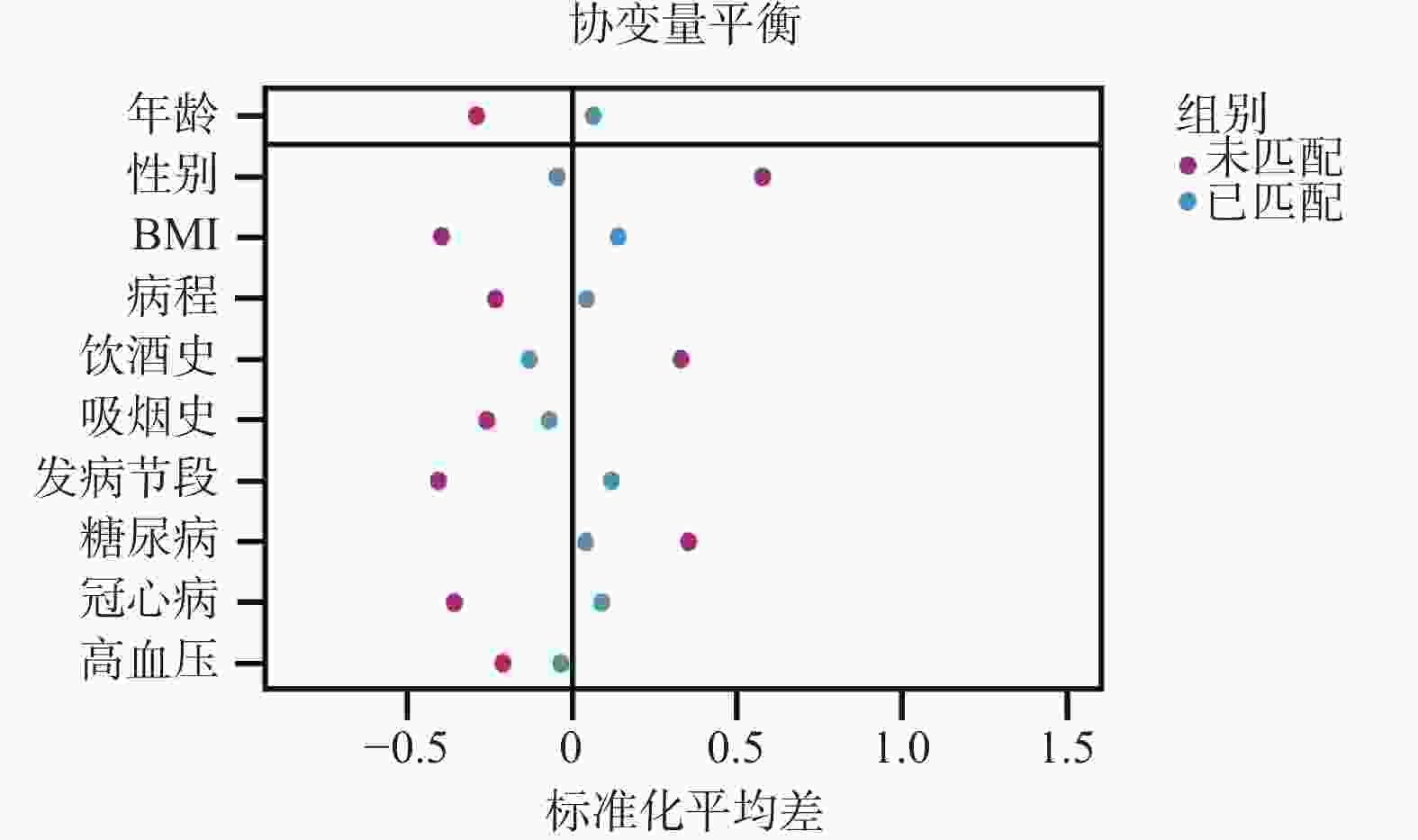
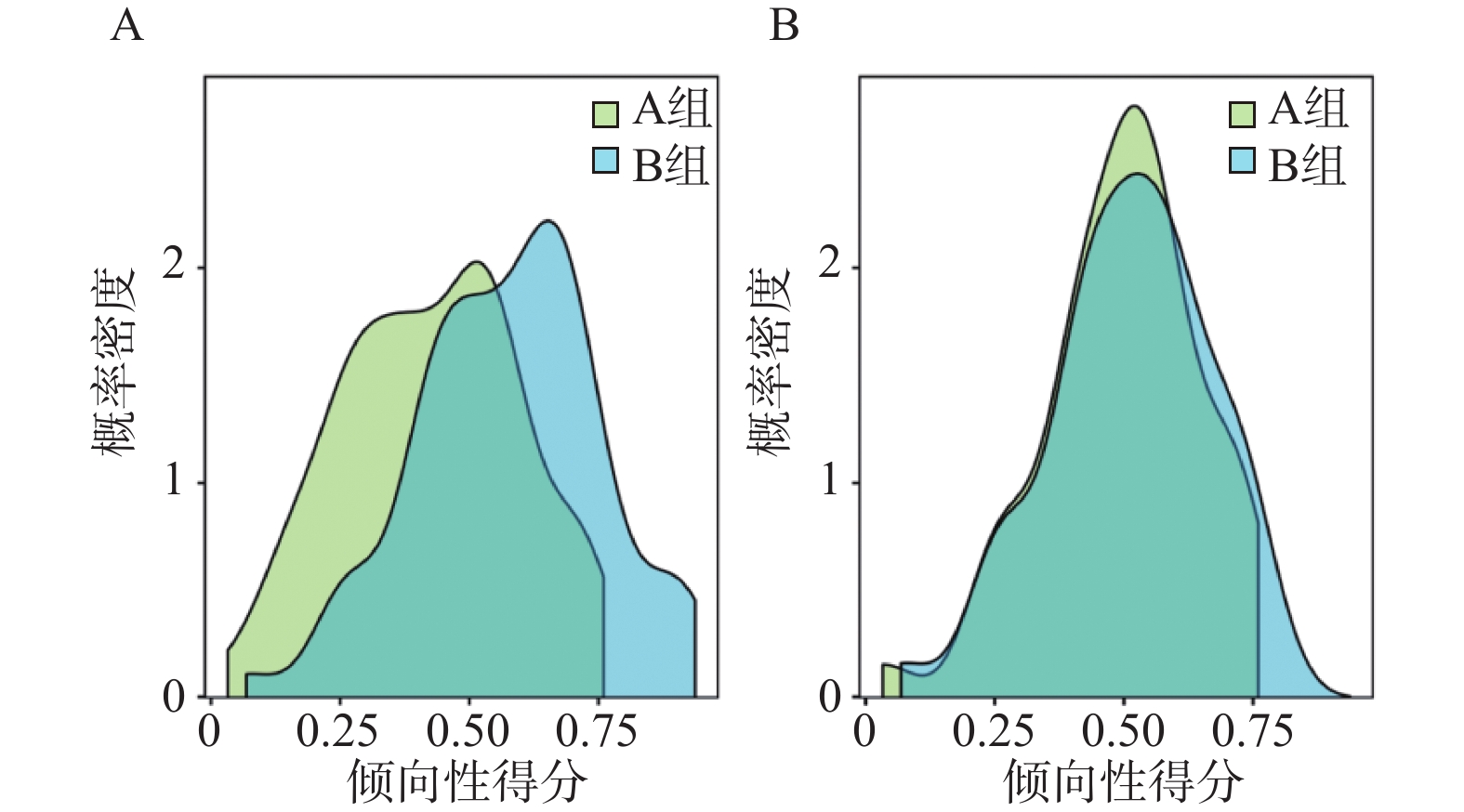
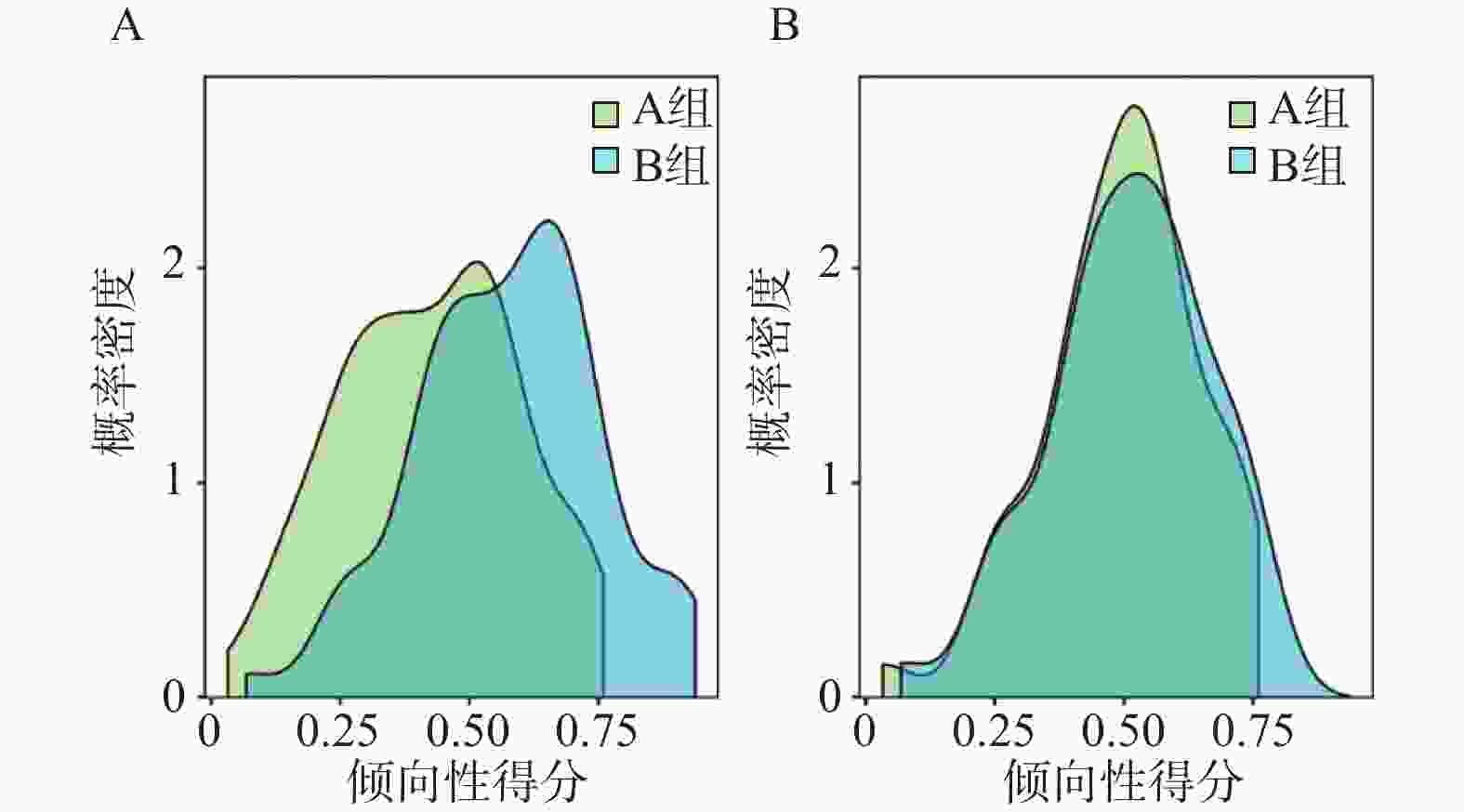
目的 探讨短时程脊髓电刺激(short-term spinal cord stimulation,stSCS)和短时程背根神经节电刺激(short-term dorsal root ganglion stimulation,stDRG)治疗带状疱疹相关神经痛(zoster associated neuralgia,ZAN)的临床疗效及对睡眠质量的影响。 方法 选择2022年9月至2024年5月于河北医科大学第二医院诊治的124例ZAN患者,根据患者治疗方式不同分为A组(stSCS)、B组(stDRG),每组各62例。采用倾向性评分匹配(propensity score matching,PSM)均衡组间协变量后,比较两组患者临床疗效;分析治疗前后视觉模拟量表(visual analogue scale,VAS)、神经病理性疼痛筛选问卷(pain-DETECT questionnaire,PD-Q)、汉密尔顿焦虑量表(hamilton anxiety scale,HAMA)、汉密尔顿抑郁量表(hamilton depresssion scale,HAMD)评分及炎症指标、磷脂酰肌醇-激酶(phosphoinositide3-kinase,PI3K)/蛋白激酶B(protein kinase b,AKT)/哺乳动物雷帕霉素靶蛋白(mammalian target of rapamycin,mTOR)信号通路指标、睡眠图指标的变化,并探讨各指标与PSOI评分的相关性。 结果 两组患者临床疗效、远期复发率及不良反应对比差异无统计学意义(P > 0.05);DID结果显示,两组患者VAS、PD-Q、HAMA、HAMD评分基线水平均无明显差异(P > 0.05);随着时间推移各评分均明显改善,且不同治疗方式对各评分的净效应明显(P < 0.05)。重复测量方差结果表明,两组患者炎症指标、PI3K/AKT/mTOR信号通路指标及睡眠图检测指标均随时间变化明显改变,且组间效应及交互效应明显(P < 0.05)。Pearson分析表明,PSOI、VAS、PD-Q、HAMA及HAMD评分与炎症指标、PI3K/AKT/mTOR信号通路指标、睡眠图指标均存在稳定的相关性(P < 0.05)。 结论 stSCS与stDRG均能有效改善ZAN患者生活质量,其中stSCS对镇痛效果的持续性、对睡眠的稳定作用更具优势。 Abstract:Objective To explore the clinical efficacy and impact on sleep quality of short-term spinal cord stimulation (stSCS) and short-term dorsal root ganglion stimulation (stDRG) in treating zoster associated neuralgia (ZAN). Methods A total of 124 patients with ZAN diagnosed and treated at the Second Hospital of Hebei Medical University between September 2022 and May 2024 were selected and divided into Group A (stSCS) and Group B (stDRG) according to different treatment modalities, with 62 cases in each group. After propensity score matching (PSM) to balance covariates between groups, clinical efficacy was compared. Changes in visual analogue scale (VAS), pain-DETECT questionnaire (PD-Q), Hamilton anxiety scale (HAMA), Hamilton depression scale (HAMD) scores, inflammatory indicators, phosphatidylinositol-3-kinase (PI3K)/protein kinase B (AKT)/mammalian target of rapamycin (mTOR) signaling pathway indicators and polysomnography parameters before and after treatment were analyzed, and the correlation between each indicator and PSOI score was explored. Results There was no statistically significant difference in clinical efficacy, long-term recurrence rate and adverse reactions between the two groups (P > 0.05). Difference-in-differences (DID) analysis showed no significant baseline differences in VAS, PD-Q, HAMA, and HAMD scores between groups (P > 0.05); all scores significantly improved over time, and the net effects of different treatment methods on each score were evident (P < 0.05). Repeated-measures ANOVA showed that the inflammatory indicators, PI3K/AKT/mTOR signaling pathway indicators, and polysomnography parameters in both groups changed significantly over time, with evident between-group and interaction effects (P < 0.05). Pearson correlation analysis demonstrated stable correlations between PSQI, VAS, PD-Q, HAMA, and HAMD scores and inflammatory markers, PI3K/AKT/mTOR signaling pathway indicators, and polysomnography parameters (P < 0.05). Conclusion Both stSCS and stDRG can effectively improve quality of life of ZAN patients, with stSCS demonstrating greater advantages in sustained analgesic efficacy and stable sleep-improving effects. -
表 1 PSM前后两组患者一般资料比较[($\bar x \pm s $)/n(%)]
Table 1. Comparison of general characteristics of patients before and after PSM[($\bar x \pm s $)/n(%)]
指标 PSM前 PSM后 A组(n=62) B组(n=62) χ2/t P A组(n=51) B组(n=51) χ2/t P 年龄(岁) 63.82 ± 11.97 66.27 ± 10.94 1.190 0.236 64.31 ± 12.63 65.78 ± 10.8 0.632 0.529 性别 3.912 0.048* 0.982 0.322 男 27(43.55) 38(61.29) 24(47.06) 29(56.86) 女 35(56.45) 24(38.71) 27(52.94) 22(43.14) BMI(kg/m2) 21.48 ± 1.97 22.19 ± 1.88 2.053 0.042* 21.56 ± 1.95 22.15 ± 1.53 1.700 0.092 病程(月) 2.37 ± 1.06 2.39 ± 1.08 0.104 0.917 2.35 ± 1.05 2.27 ± 1.06 0.422 0.674 饮酒史 32(51.61) 20(32.26) 4.769 0.029* 22(43.14) 19(37.25) 0.367 0.545 吸烟史 26(41.94) 24(38.71) 0.134 0.714 17(33.33) 18(35.29) 0.043 0.835 发病节段 0.570 0.752 1.042 0.594 颈段 13(20.97) 14(22.58) 10(19.61) 12(23.53) 胸段 25(40.32) 28(45.16) 19(37.25) 22(43.14) 腰段 24(38.71) 20(32.26) 22(43.14) 17(33.33) 糖尿病 30(48.39) 37(59.68) 1.591 0.207 25(49.02) 27(52.94) 0.157 0.692 冠心病 26(41.94) 28(45.16) 0.131 0.717 21(41.18) 19(37.25) 0.165 0.685 高血压 36(58.06) 29(46.77) 1.584 0.208 29(56.86) 25(49.02) 0.630 0.427 *P < 0.05。 表 2 两组患者临床疗效比较[n(%)]
Table 2. Comparison of clinical efficacy between the two groups[n(%)]
指标 A组(n=51) B组(n=51) Z/χ2 P 痊愈 26(50.98) 22(43.14) 1.451 0.694 显效 16(31.37) 18(35.29) 有效 8(15.69) 8(15.69) 无效 1(1.96) 3(5.88) 总有效率 50(98.04) 48(94.12) 1.041 0.308 远期复发率 6(11.76) 11(21.57) 1.765 0.184 表 3 两组患者不良反应比较[n(%)]
Table 3. Comparison of adverse reactions between the two groups[n(%)]
指标 A组(n=51) B组(n=51) Fisher/χ2 P 头晕 3(5.88) 1(1.96) − 0.308 恶心呕吐 1(1.96) 0(0.00) − 0.315 穿刺点出血 1(1.96) 1(1.96) − 1.000 穿刺点疼痛 2(3.92) 2(3.92) − 1.000 电极移位 2(3.92) 4(7.84) − 0.400 总计 9(17.65) 8(15.69) 0.071 0.790 表 4 两组患者治疗前后相关评分比较($\bar x \pm s $,分)
Table 4. Comparison of relevant scores before and after treatment between the two groups($\bar x \pm s $,points)
指标 A组(n=51) B组(n=51) t P PSOI评分 T0 15.27 ± 2.41 15.71 ± 1.86 1.013 0.314 T1 5.51 ± 1.10a 6.84 ± 1.33a 5.507 <0.001* T2 4.22 ± 1.33a 4.92 ± 1.31ab 2.700 0.008* T3 1.96 ± 0.66abc 2.25 ± 1.11abc 1.624 0.107 VAS评分 T0 6.96 ± 1.33 6.88 ± 1.32 −0.299 0.765 T1 1.08 ± 0.66a 1.92 ± 0.60a 6.785 <0.001* T2 0.94 ± 0.76a 1.18 ± 0.79a 1.531 0.129 T3 0.53 ± 0.50abc 0.65 ± 0.63abc 1.044 0.299 PD-Q评分 T0 19.51 ± 1.86 19.27 ± 2.19 −0.585 0.560 T1 10.96 ± 0.94a 14.24 ± 2.06a 10.353 <0.001* T2 10.59 ± 0.85a 11.53 ± 3.30a 1.975 0.051 T3 10.22 ± 1.06ab 10.35 ± 2.28ab 0.390 0.698 HAMA评分 T0 23.04 ± 3.22 22.80 ± 3.24 −0.368 0.714 T1 17.20 ± 2.28a 18.82 ± 2.15a 3.707 <0.001* T2 11.69 ± 1.83ab 12.37 ± 2.40ab 1.625 0.107 T3 8.55 ± 1.57abc 9.29 ± 2.26abc 1.932 0.056 HAMD评分 T0 20.59 ± 2.64 23.57 ± 3.62 4.748 <0.001* T1 14.84 ± 2.59a 18.63 ± 2.90a 6.956 <0.001* T2 11.06 ± 1.98ab 11.90 ± 2.31ab 1.978 0.051 T3 6.75 ± 1.82abc 6.86 ± 2.68abc 0.259 0.796 与同组T0相比,aP < 0.05;与同组T1相比,bP < 0.05;与同组T2相比,cP < 0.05;*P < 0.05。 表 5 DID模型评估不同治疗方式对相关评分的影响
Table 5. Evaluation of the impact of different treatment methods on relevant scores using DID model
DID模型 β SE t P PSOI评分 组别 0.431 0.327 1.318 0.189 时间 −13.314 0.327 −40.677 <0.001* 组别×时间 −0.437 0.163 −3.297 0.001* VAS评分 组别 −0.078 0.202 −0.389 0.698 时间 −6.431 0.202 −31.879 <0.001* 组别×时间 −0.896 0.285 −3.687 0.003* PD-Q评分 组别 −0.235 0.378 −0.622 0.534 时间 −9.294 0.378 −24.580 <0.001* 组别×时间 −0.673 0.035 −5.697 0.007* HAMA评分 组别 −0.235 0.528 −0.446 0.656 时间 −14.49 0.528 −27.45 <0.001* 组别×时间 −0.980 0.147 −4.313 0.011* HAMD评分 组别 0.820 0.533 0.440 0.725 时间 −13.843 0.548 −25.269 <0.001* 组别×时间 −2.863 0.775 −3.695 <0.001* *P < 0.05。 表 6 两组患者治疗前后炎症指标比较
Table 6. Comparison of inflammatory indicators before and after treatment in the two groups
指标 A组(n=51) B组(n=51) t P TNF-α(pg/mL) T0 19.76 ± 5.15 20.16 ± 3.99 0.435 0.665 T1 8.72 ± 2.78 5.94 ± 1.32 −6.439 <0.001* T2 5.35 ± 2.13 5.03 ± 0.96 −0.989 0.325 T3 3.10 ± 0.84 3.29 ± 1.04 1.019 0.311 F组间=6.198,P组间=0.014* F时间=756.499,P时间<0.001* F交互=7.093,P交互=0.002* CRP(mg/L) T0 12.43 ± 2.13 12.32 ± 2.06 −0.283 0.777 T1 4.16 ± 0.88 5.06 ± 1.01 4.803 <0.001* T2 3.90 ± 1.08 4.39 ± 0.89 2.498 0.014* T3 3.76 ± 0.93 4.02 ± 1.07 1.321 0.190 F组间=7.829,P组间=0.006* F时间=958.314,P时间<0.001* F交互=2.586,P交互=0.045* IL-6(pg/mL) T0 89.34 ± 13.73 90.52 ± 12.34 0.456 0.649 T1 19.82 ± 6.79 26.27 ± 4.94 5.494 <0.001* T2 14.35 ± 4.29 15.17 ± 3.43 1.071 0.287 T3 7.32 ± 2.19 7.55 ± 1.76 0.579 0.564 F组间=9.525,P组间=0.003* F时间= 2533.623 ,P时间<0.001*F交互=3.656,P交互=0.040* IL-1β(pg/mL) T0 7.07 ± 1.03 7.55 ± 3.07 1.060 0.292 T1 1.69 ± 0.37 2.59 ± 0.74 7.785 <0.001* T2 1.13 ± 0.41 1.70 ± 0.68 5.077 <0.001* T3 0.94 ± 0.29 1.00 ± 0.29 1.178 0.242 F组间=19.519,P组间<0.001* F时间=566.608,P时间<0.001* F交互=1.916,P交互=0.006* *P < 0.05。 表 7 两组患者治疗前后PI3K/AKT/mTOR信号通路相关指标比较
Table 7. Comparison of PI3K/AKT/mTOR signaling pathway-related indicators before and after treatment in the two groups
指标 A组(n=51) B组(n=51) t P PI3K(pg/L) T0 12.18 ± 3.04 12.69 ± 3.12 0.828 0.410 T1 6.48 ± 1.00 7.06 ± 1.08 2.807 0.006* T2 5.01 ± 1.29 5.61 ± 1.36 2.292 0.024* T3 3.93 ± 1.44 4.04 ± 1.26 0.406 0.686 F组间=6.065,P组间=0.015* F时间=393.431,P时间<0.001* F交互=0.377,P交互=0.005* AKT(pg/L) T0 10.32 ± 3.55 10.98 ± 3.23 0.976 0.332 T1 4.65 ± 0.72 5.92 ± 1.04 7.167 <0.001* T2 4.05 ± 0.56 4.29 ± 1.46 1.097 0.275 T3 3.48 ± 0.54 3.51 ± 1.04 0.183 0.855 F组间=9.009,P组间=0.003* F时间=298.792,P时间<0.001* F交互=2.112,P交互=0.014* mTOR(pg/L) T0 7.75 ± 0.86 7.41 ± 0.95 −1.895 0.061 T1 3.16 ± 0.52 4.27 ± 0.47 11.298 <0.001* T2 2.95 ± 0.50 3.13 ± 0.84 1.277 0.205 T3 2.12 ± 0.57 2.28 ± 0.77 1.160 0.249 F组间=14.288,P组间<0.001* F时间= 1184.528 ,P时间<0.001*F交互=19.114,P交互<0.001* *P < 0.05。 表 8 两组患者治疗前后睡眠图检测指标比较
Table 8. Comparison of sleep graph detection indicators before and after treatment between the two groups of patients
指标 A组(n=51) B组(n=51) t P TST(min) T0 146.49 ± 15.09 148.00 ± 17.03 0.474 0.637 T1 238.08 ± 18.95 216.43 ± 19.64 −5.665 <0.001* T2 338.69 ± 24.90 306.75 ± 65.30 −3.264 0.002* T3 435.55 ± 39.07 424.35 ± 74.11 −0.954 0.342 F组间=12.852,P组间=0.001* F时间=991.944,P时间<0.001* F交互=3.415,P交互=0.030* AT(次) T0 6.75 ± 1.93 7.12 ± 1.89 0.985 0.327 T1 5.76 ± 1.24 6.71 ± 1.58 3.346 0.001* T2 4.51 ± 1.14 4.84 ± 1.71 1.157 0.250 T3 3.47 ± 0.88 3.59 ± 1.70 0.439 0.662 F组间=8.116,P组间=0.005* F时间=100.372,P时间<0.001* F交互=1.320,P交互=0.026* SL(min) T0 62.49 ± 6.53 62.78 ± 8.19 0.201 0.841 T1 47.37 ± 5.30 53.35 ± 7.84 4.516 <0.001* T2 33.59 ± 2.74 36.71 ± 6.56 3.131 0.002* T3 19.53 ± 2.34 20.69 ± 5.97 1.289 0.200 F组间=17.976,P组间<0.001* F时间=984.299,P时间<0.001* F交互=4.596,P交互=0.006* SE(%) T0 48.56 ± 5.48 48.13 ± 4.95 −0.414 0.680 T1 61.55 ± 6.06 53.17 ± 11.90 −4.483 <0.001* T2 74.41 ± 6.31 72.06 ± 7.65 −1.691 0.094 T3 91.27 ± 9.38 91.02 ± 10.62 −0.129 0.898 F组间=11.281,P组间=0.001* F时间=562.904,P时间<0.001* F交互=5.761,P交互=0.001* REM(%) T0 12.84 ± 1.20 13.09 ± 0.92 1.181 0.240 T1 15.15 ± 1.90 13.38 ± 2.65 −3.860 <0.001* T2 17.87 ± 2.01 17.45 ± 1.98 −1.080 0.283 T3 21.64 ± 3.36 21.04 ± 3.00 −0.956 0.342 F组间=6.970,P组间=0.010* F时间=293.309,P时间<0.001* F交互=3.656,P交互=0.021* *P < 0.05。 表 9 炎症指标、PI3K/AKT/mTOR通路指标、睡眠图指标与各评分的相关性分析
Table 9. Correlation analysis of inflammatory indicators,PI3K/AKT/mTOR pathway indicators,sleep graph indicators,and various vssessment scores
指标 PSOI评分 VAS评分 PD-Q评分 HAMA评分 HAMD评分 r P r P r P r P r P TNF-α 0.939 0.031* 0.690 <0.001* 0.654 0.045* 0.760 <0.001* 0.876 <0.001* CRP 0.515 0.024* 0.903 0.003* 0.929 0.034* 0.717 0.020* 0.508 <0.001* IL-6 0.560 0.049* 0.441 <0.001* 0.607 0.024* 0.504 <0.001* 0.887 <0.001* IL-1β 0.752 0.046* 0.913 <0.001* 0.721 0.044* 0.808 <0.001* 0.719 <0.001* PI3K 0.648 0.032* 0.752 0.006* 0.440 0.005* 0.993 0.002* 0.582 0.021* AKT 0.553 0.046* 0.550 0.010* 0.650 0.040* 0.759 0.031* 0.902 0.017* mTOR 0.675 0.012* 0.893 0.027* 0.528 0.002* 0.954 0.028* 0.553 0.030* TST −0.730 <0.001* −0.731 0.001* −0.586 0.012* −0.461 <0.001* −0.928 <0.001* SE −0.426 <0.001* −0.672 0.030* −0.902 0.029* −0.413 <0.001* −0.874 <0.001* REM −0.896 <0.001* −0.738 0.049* −0.416 0.024* −0.982 0.027* −0.654 0.018* AT 0.592 <0.001* 0.844 0.001* 0.524 0.017* 0.456 <0.001* 0.940 0.025* SL 0.757 <0.001* 0.938 0.003* 0.650 0.005* 0.948 0.004* 0.796 0.012* *P < 0.05。 -
[1] Warner B E, Goins W F, Kramer P R, et al. A guide to preclinical models of zoster-associated pain and postherpetic neuralgia[J]. Curr Top Microbiol Immunol, 2023, 438: 189-221. [2] Díez-Domingo J, Curran D, Del Rosario Cambronero M, et al. Economic burden and impact on quality of life of herpes zoster in Spanish adults aged 50 years or older: A prospective cohort study[J]. Adv Ther, 2021, 38(6): 3325-3341. doi: 10.1007/s12325-021-01717-7 [3] Wen H, Wang Y, Cheng H, et al. Outcomes of twice repeated high-voltage long-duration pulsed radiofrequency treatment in subacute postherpetic neuralgia: A retrospective single-center analysis[J]. J Pain Res, 2024, 17: 2043-2050. doi: 10.2147/JPR.S465251 [4] Wen B, Wang Y, Zhang C, et al. Efficacy of different interventions for the treatment of postherpetic neuralgia: A Bayesian network meta-analysis[J]. J Int Med Res, 2020, 48(12): 0300060520977416. [5] Zuo L, Su A, Xie Y, et al. Clinical study of short-term spinal cord stimulation for herpes zoster-associated pain[J]. Eur J Med Res, 2024, 29(1): 603. doi: 10.1186/s40001-024-02196-6 [6] Wang X, Gao Y, Yu J, et al. The efficacy and prognosis analysis of short-term spinal cord stimulation in the treatment of zoster-associated pain: A retrospective study[J]. Front Neurol, 2025, 16: 1611447. doi: 10.3389/fneur.2025.1611447 [7] Bharthi R, Kusyk D M, Patterson M, et al. Open surgical implantation of lumbosacral dorsal root ganglion stimulators for chronic pain: Analysis of patient outcomes and operative technique[J]. World Neurosurg, 2025, 193: 1099-1105. doi: 10.1016/j.wneu.2024.09.112 [8] 张妮楠, 高昕妍, 刘坤, 等. 活体钙成像探索电针对不同刺激在背根节神经元初级传入水平的影响[J]. 针刺研究, 2025, 50(4): 357-365. doi: 10.13702/j.1000-0607.20240065 [9] Ravaillault S, Samarut E, Ploteau S, et al. Involvement of the sinuvertebral nerve in the treatment of chronic low back pain through dorsal root ganglion neurostimulation: An anatomical study[J]. Surg Radiol Anat, 2025, 47(1): 160. doi: 10.1007/s00276-025-03671-3 [10] Chen Y Y, Sun H T. Response to: Comparing the efficacy of dorsal root ganglion stimulation with conventional medical management in patients with chronic postsurgical inguinal pain: Post hoc analyzed results of the SMASHING study[J]. Neuromodulation, 2025, 28(1): 188-189. doi: 10.1016/j.neurom.2024.09.474 [11] 陈燕中, 赖尚导, 刘炯锋, 等. 脊神经射频与脊髓电刺激治疗带状疱疹相关性疼痛的临床研究[J]. 中国现代医学杂志, 2024, 34(15): 94-98. [12] 陈嘉芳, 何龙, 林鹏, 等. 短时程脊髓电刺激与双极脉冲射频治疗带状疱疹后神经痛的临床研究[J]. 中国疼痛医学杂志, 2024, 30(9): 664-670. [13] 徐佳丽, 王昆鹏, 奚奇, 等. 短时程背根神经节电刺激治疗带状疱疹相关性疼痛的疗效观察[J]. 中国疼痛医学杂志, 2023, 29(6): 458-462. [14] 黄景妹, 王萍, 叶峻宏, 等. 背根神经节脉冲射频联合普瑞巴林治疗老年胸段带状疱疹后神经痛的疗效及对血清相关因子水平的影响[J]. 中国老年学杂志, 2023, 43(15): 3729-3732. [15] Patil A, Goldust M, Wollina U. Herpes zoster: A review of clinical manifestations and management[J]. Viruses, 2022, 14(2): 192. doi: 10.3390/v14020192 [16] Curran D, Doherty T M, Lecrenier N, et al. Healthy ageing: Herpes zoster infection and the role of zoster vaccination[J]. NPJ Vaccines, 2023, 8(1): 184. doi: 10.1038/s41541-023-00757-0 [17] Shen Y, Lin P. Association between frailty and postherpetic neuralgia in the older adult with herpes zoster[J]. Front Public Health, 2025, 13: 1511898. doi: 10.3389/fpubh.2025.1511898 [18] Han G, Han Y, Yu L, et al. Patterns and trends in pharmacological treatment for outpatients with postherpetic neuralgia in six major areas of China, 2015-2019[J]. Healthcare, 2023, 11(5): 764. doi: 10.3390/healthcare11050764 [19] Li Y, Wang J, Chen Y, et al. Comparative long-term efficacy of short-term spinal cord stimulation versus bipolar pulsed radiofrequency for refractory postherpetic neuralgia: A 24 month prospective study[J]. Eur J Med Res, 2025, 30(1): 272. doi: 10.1186/s40001-025-02560-0 [20] Malinowski M N, Chopra P R, Tieppo Francio V, et al. A narrative review and future considerations of spinal cord stimulation, dorsal root ganglion stimulation and peripheral nerve stimulation[J]. Curr Opin Anaesthesiol, 2021, 34(6): 774-780. doi: 10.1097/ACO.0000000000001072 [21] 乔保光, 吴方方, 陈巧艳, 等. 双电极短时程脊髓电刺激治疗带状疱疹后神经痛的应用研究[J]. 中国疼痛医学杂志, 2025, 31(3): 189-195. [22] Xue S, Yang W J, Cao Z X, et al. Comparing the efficacy and safety of short-term spinal cord stimulation and pulsed radiofrequency for zoster-related pain: A systematic review and meta-analysis[J]. Medicine, 2022, 101(11): e29073. [23] 陈可, 武彩花, 郑俊, 等. 基于PI3K/Akt信号通路探究电针对带状疱疹后遗神经痛大鼠神经功能的干预机制[J]. 中国老年学杂志, 2023, 43(6): 1374-1377. [24] Liu Y, Qin X, Lu X, et al. Effects of inhibiting the PI3K/Akt/mTOR signaling pathway on the pain of sciatic endometriosis in a rat model[J]. Can J Physiol Pharmacol, 2019, 97(10): 963-970. doi: 10.1139/cjpp-2019-0156 [25] 代景娜, 王琳琳, 付利然. 针灸疗法对带状疱疹后遗神经痛患者血清细胞因子和疼痛因子水平的影响[J]. 广州中医药大学学报, 2020, 37(7): 1292-1297. [26] Huang M, Chen Q, Wu S, et al. Treatment efficacy and technical advantages of temporary spinal nerve root stimulation compared to traditional spinal cord stimulation for postherpetic neuralgia[J]. Pain Physician, 2022, 25(6): 863-873. [27] Li X, Zhang H, Zhang X, et al. A central and peripheral dual neuromodulation strategy in pain management of zoster-associated pain[J]. Sci Rep, 2024, 14(1): 24672. doi: 10.1038/s41598-024-75890-4 -





 下载:
下载: