The Moderating Effect of Pain Frequency on Sleep Quality and Anxiety in Young Adults with Chronic Low Back Pain
-
摘要:
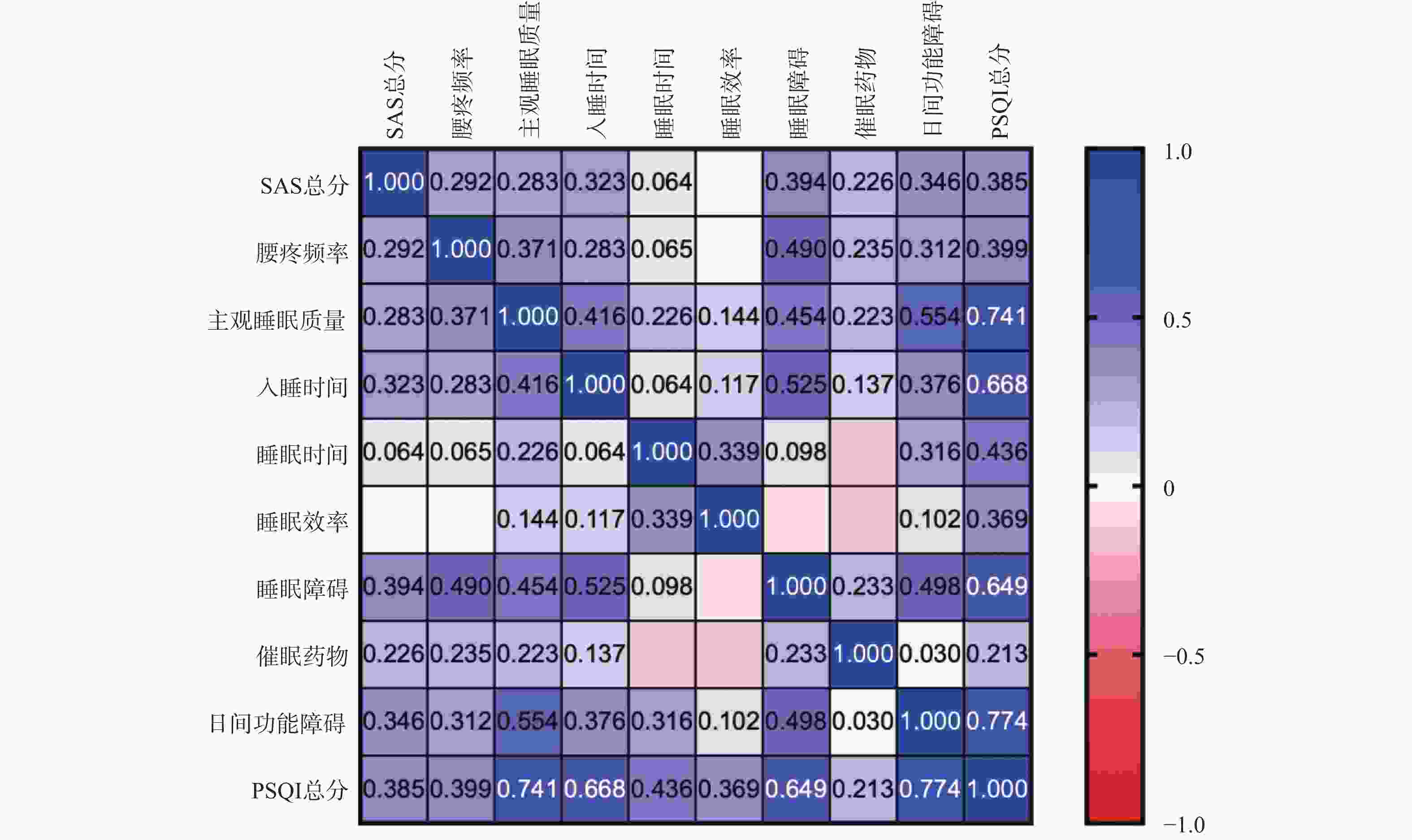
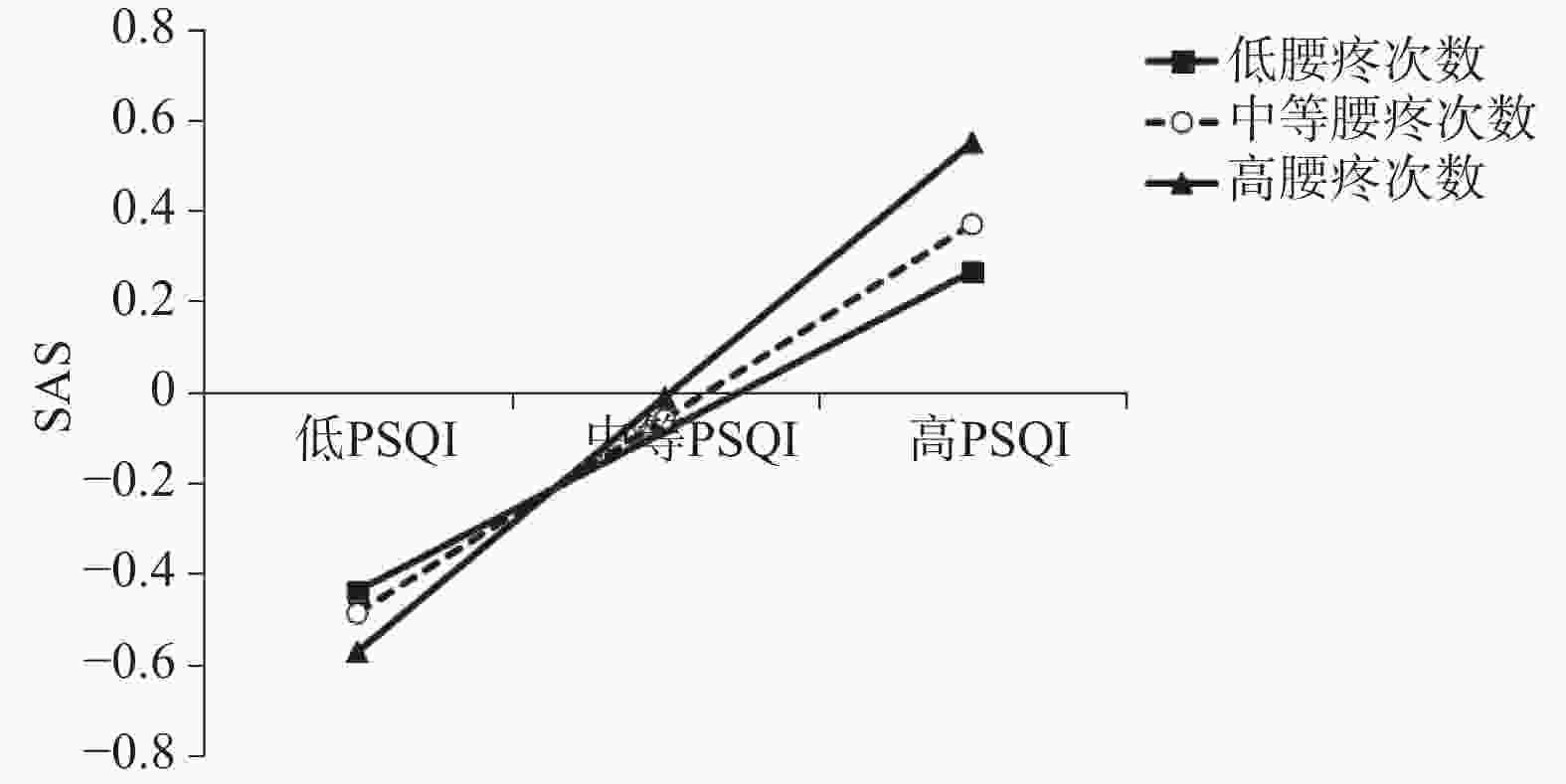
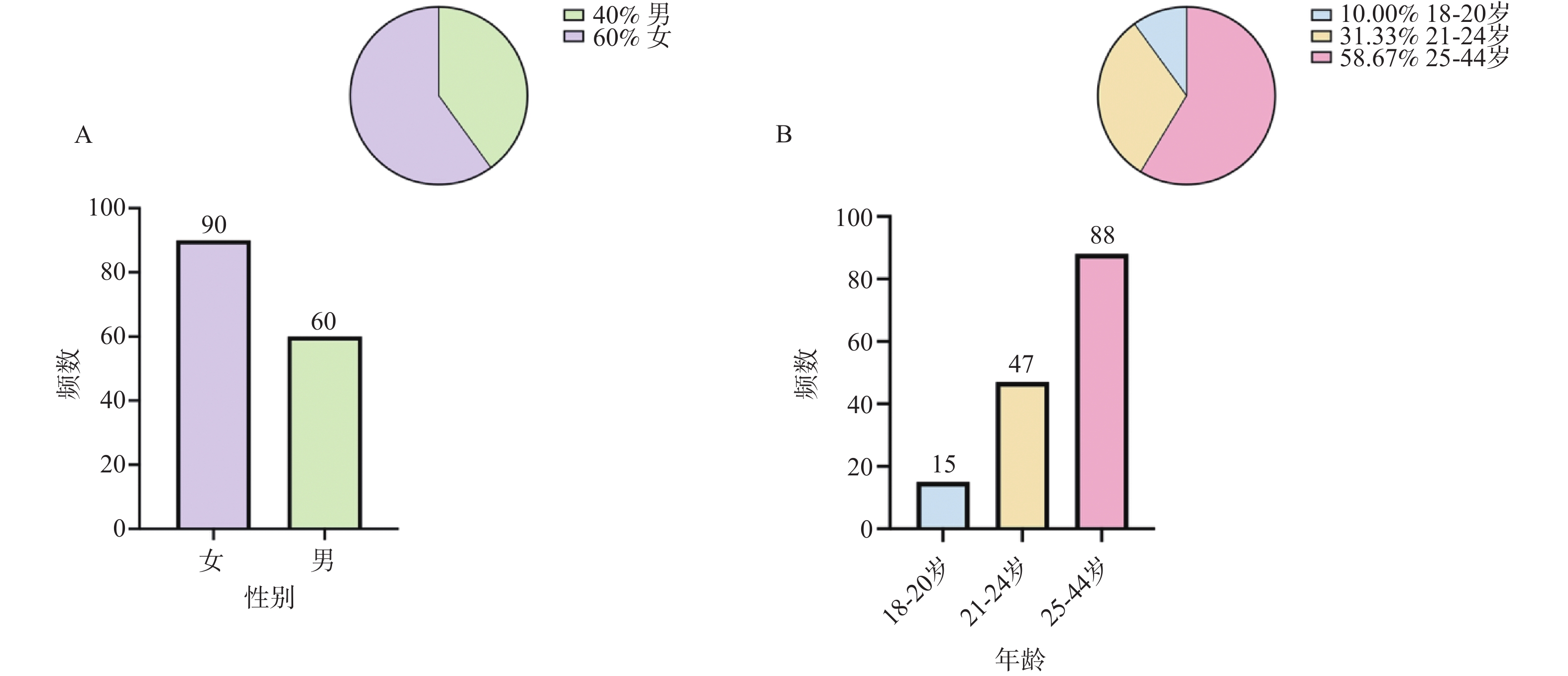
目的 探究青年慢性下背痛(chronic low back pain,CLBP)患者睡眠与焦虑情绪的关系并分析疼痛频率在睡眠-焦虑中是否发挥调节作用。 方法 横断面研究设计,对2024年9月至2025年5月在昆明医科大学第一附属医院康复科就诊的150例青年CLBP患者(18~44岁)进行问卷调查,利用匹兹堡睡眠质量指数(pittsburgh sleep quality index,PSQI)和焦虑自评量表(self-rating anxiety scale,SAS)分别评估睡眠质量与焦虑情绪,统计学方法采用非参数检验、Spearman相关分析和Process 4.2检验。 结果 PSQI总分与SAS总分呈正相关(rs = 0.385,P < 0.01),腰痛频率与PSQI总分(rs = 0.399)和睡眠障碍(rs = 0.490)呈正相关(P < 0.01);不同性别与年龄对睡眠和焦虑差异无统计学意义(P > 0.05);PSQI与腰痛频率的交互项对SAS有正向预测作用(β = 0.133,P < 0.05);不同腰痛频率水平的PSQI对SAS均呈显著预测效应(95%CI不包含0)。 结论 青年CLBP患者睡眠与焦虑情绪相关,且疼痛频率在睡眠-焦虑中发挥调节作用,腰痛频率增加可能加重睡眠障碍进而导致焦虑情绪,提示疼痛频率应作为临床干预的重要预警指标之一。 Abstract:Objective To investigate the correlation between sleep quality and anxiety symptoms in young adults with chronic low back pain (CLBP), and to analyze the moderating effect of pain frequency in the sleep-anxiety relationship. Methods A cross-sectional study design was employed, and a questionnaire survey was conducted among 150 young CLBP patients (aged 18 ~ 44 years) who attended the Rehabilitation Medicine Department of the First Affiliated Hospital of Kunming Medical University from September 2024 to May 2025. Sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI), while anxiety levels were measured with the Self-rating Anxiety Scale (SAS). Statistical analyses included non-parametric tests, Spearman correlation analysis, and Process macro (version 4.2). Results A significantly positive correlation was demonstrated between the total PSQI score and the total SAS score (rs = 0.385, P < 0.01). Low back pain frequency demonstrated significantly positive correlations with both the PSQI total score (rs = 0.399) and the sleep disturbance dimension (rs = 0.490, P < 0.01). No statistically significant differences in sleep or anxiety were found based on gender or age (P > 0.05). Hierarchical regression analysis revealed that the interaction term between PSQI and low back pain frequency had a significant positive predictive effect on SAS (β = 0.133, P < 0.05). PSQI scores significantly predicted SAS scores across different levels of low back pain frequency (95% CI did not include 0). Conclusions Sleep quality is correlated with anxiety in young adults with CLBP, and pain frequency plays a moderating role in the sleep-anxiety relationship. Increased frequency of low back pain may exacerbate sleep problems, thereby contributing to anxiety. This suggests that pain frequency should be regarded as an important early warning indicator in clinical intervention. -
Key words:
- Chronic low back pain /
- Sleep quality /
- Anxiety /
- Pain frequency /
- Young adult
-
表 1 PSQI量表与SAS量表分级得分情况 [n = 150,M(P25,P75) ]
Table 1. Score profiles of the PSQI and SAS scales[n = 150,M(P25,P75)]
量表 维度/等级 频数(%) 得分(分) PSQI 主观睡眠质量 1.00 (0.00,2.00) 入睡时间 1.00 (1.00,2.00) 睡眠时间 1.00 (0.00,1.00) 睡眠效率 0.00 (0.00,1.00) 睡眠障碍 1.00 (1.00,1.00) 催眠药物 0.00 (0.00,0.00) 日间功能障碍 0.00 (0.00,2.00) 睡眠质量好 67 (44.7) 4.00 (3.00,5.00) 睡眠质量差 83 (55.3) 8.00 (6.00,10.00) PSQI总分 6.00 (4.00,8.00) SAS 无焦虑 106 (70.7) 41.25 (38.75,45.00) 轻度焦虑 37 (24.7) 52.50 (50.00,55.63) 中度焦虑 5 (3.3) 63.75 (61.25,65.00) 重度焦虑 2 (1.3) 81.25 (81.25,81.25) SAS总分 43.75 (40.00,50.00) 表 2 不同性别SAS与PSQI得分比较 [n = 150,M(P25,P75)]
Table 2. Comparison of SAS and PSQI scores by genders [n = 150,M(P25,P75)]
项目 男(n = 60) 女(n = 90) Z P SAS总分 43.75 (40.00,50.94) 43.75 (40.00,50.00) −0.086 0.931 主观睡眠质量 1.00 (0.00,2.00) 1.00 (0.75,1.25) −0.231 0.817 入睡时间 1.00 (1.00,2.00) 1.00 (1.00,2.00) −1.401 0.161 睡眠时间 1.00 (0.00,1.00) 1.00 (0.00,1.00) −0.554 0.580 睡眠效率 0.00 (0.00,0.00) 0.00 (0.00,1.00) −1.629 0.103 睡眠障碍 1.00 (1.00,1.00) 1.00 (1.00,1.00) −1.313 0.189 催眠药物 0.00 (0.00,0.00) 0.00 (0.00,1.00) −1.366 0.172 日间功能障碍 1.00 (0.25,2.00) 1.00 (1.00,2.00) −0.881 0.378 PSQI总分 5.00 (4.00,7.00) 6.00 (4.00,8.00) −1.421 0.155 表 3 不同年龄的SAS、PSQI得分比较 [n = 150,M(P25,P75) ]
Table 3. Comparison of SAS and PSQI scores by age group [n = 150,M(P25,P75)]
项目 20岁及以下 21~24岁 24岁以上 H P (n = 15) (n = 47) (n = 88) SAS总分 46.25(42.50,50.00) 42.50(40.00,50.00) 44.38(40.00,51.25) 1.046 0.593 主观睡眠质量 1.00(1.00,1.00) 1.00(0.00,2.00) 1.00(0.00,1.75) 0.243 0.886 入睡时间 1.00(0.00,2.00) 1.00(1.00,2.00) 1.00(1.00,2.00) 4.768 0.092 睡眠时间 1.00(0.00,1.00) 1.00(0.00,1.00) 1.00(0.00,1.00) 0.936 0.626 睡眠效率 0.00(0.00,0.00) 0.00(0.00,1.00) 0.00(0.00,1.00) 4.394 0.111 睡眠障碍 1.00(1.00,1.00) 1.00(1.00,1.00) 1.00(1.00,1.75) 0.647 0.723 催眠药物 0.00(0.00,0.00) 0.00(0.00,0.00) 0.00(0.00,0.00) 1.545 0.462 日间功能障碍 1.00(1.00,2.00) 1.00(1.00,2.00) 1.00(1.00,2.00) 0.110 0.946 PSQI总分 5.00(4.00,7.00) 6.00(5.00,8.00) 6.00(4.00,8.00) 2.257 0.323 表 4 腰疼频率的调节效应分析
Table 4. Analysis of the modulating effects on the frequency of low back pain
项目 方程1 方程2 方程3 β t β t β t PSQI 0.499 7.013*** 0.432 5.461*** 0.428 5.471*** 腰疼频率 0.151 1.906 0.048 0.509 PSQI×腰疼频率 0.133 2.015* R2 0.249 0.268 0.287 F 49.177*** 26.842*** 19.621*** *P < 0.05;**P< 0.01;***P < 0.001;因变量为SAS总分。 表 5 不同腰疼频率水平下的Process分析
Table 5. Process analysis at different levels of low back pain frequency
水平 效应值 标准误 t P 95%CI M-SD 0.352 0.088 4.018 0.000 0.197 0.525 M 0.428 0.078 5.471 0.000 0.273 0.583 M+SD 0.561 0.101 5.541 0.000 0.361 0.762 注:M(mean):均值;SD(standard deviation):标准差;CI(confidence interval):置信区间。 -
[1] Kechagias D, Chatzipapas C, Karaglani M, et al. Efficacy of bioelectrical impedance analysis for the evaluation of physical impairment in chronic low back pain. results from a cohort study[J]. Folia Med, 2021, 63(6): 919-927. doi: 10.3897/folmed.63.e59311 [2] Goodin B R, Overstreet D S, Penn T M, et al. Epigenome-wide DNA methylation profiling of conditioned pain modulation in individuals with non-specific chronic low back pain[J]. Clin Epigenetics, 2022, 14(1): 45. doi: 10.1186/s13148-022-01265-z [3] Calvo-Muñoz I, Kovacs F M, Roqué M, et al. Risk factors for low back pain in childhood and adolescence: A systematic review[J]. Clin J Pain, 2018, 34(5): 468-484. doi: 10.1097/AJP.0000000000000558 [4] Wang L Y, Fu T S, Tsia M C, et al. The associations of depression, anxiety, and insomnia at baseline with disability at a five-year follow-up point among outpatients with chronic low back pain: A prospective cohort study[J]. BMC Musculoskelet Disord, 2023, 24(1): 565. doi: 10.1186/s12891-023-06682-6 [5] Xu C, Fu Z, Wang J, et al. Differences and correlations of anxiety, sleep quality, and pressure-pain threshold between patients with chronic low back pain and asymptomatic people[J]. Pain Res Manag, 2022, 2022: 8648584. [6] Burgess H J, Burns J W, Buvanendran A, et al. Associations between sleep disturbance and chronic pain intensity and function: A test of direct and indirect pathways[J]. Clin J Pain, 2019, 35(7): 569-576. doi: 10.1097/AJP.0000000000000711 [7] Yoo Y M, Kim K H. Current understanding of nociplastic pain[J]. Korean J Pain, 2024, 37(2): 107-118. doi: 10.3344/kjp.23326 [8] Čeko M, Baeuerle T, Webster L, et al. The effects of virtual reality neuroscience-based therapy on clinical and neuroimaging outcomes in patients with chronic back pain: A randomized clinical trial[J]. Pain, 2024, 165(8): 1860-1874. doi: 10.1097/j.pain.0000000000003198 [9] 国家卫生健康委能力建设和继续教育中心疼痛病诊疗专项能力提升项目专家组, 程志祥, 刘先国, 等. 中国慢性腰背痛诊疗指南(2024版)[J]. 中华疼痛学杂志, 2024, 20(01): 4-22. doi: 10.3760/cma.j.issn.1000-8039.2024.08.110 [10] Buysse D J, Reynolds C F, Monk T H, et al. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research[J]. Psychiatry Res, 1989, 28(2): 193-213. doi: 10.1016/0165-1781(89)90047-4 [11] 路桃影, 李艳, 夏萍, 等. 匹兹堡睡眠质量指数的信度及效度分析[J]. 重庆医学, 2014, 43(3): 260-263. doi: 10.3969/j.issn.1671-8348.2014.03.002 [12] Ghrouz A K, Noohu M M, Dilshad Manzar M, et al. Physical activity and sleep quality in relation to mental health among college students[J]. Sleep Breath, 2019, 23(2): 627-634. doi: 10.1007/s11325-019-01780-z [13] Zung W W. A rating instrument for anxiety disorders[J]. Psychosomatics, 1971, 12(6): 371-379. doi: 10.1016/S0033-3182(71)71479-0 [14] 王芳芳. 焦虑自评量表在中学生中的测试[J]. 中国学校卫生, 1994, 15(3): 202-203. [15] Xu J, Wei Y. Social support as a moderator of the relationship between anxiety and depression: An empirical study with adult survivors of Wenchuan earthquake[J]. PLoS One, 2013, 8(10): e79045. doi: 10.1371/journal.pone.0079045 [16] Sessler K, Blechschmidt V, Hoheisel U, et al. Spinal cord fractalkine (CX3CL1) signaling is critical for neuronal sensitization in experimental nonspecific, myofascial low back pain[J]. J Neurophysiol, 2021, 125(5): 1598-1611. doi: 10.1152/jn.00348.2020 [17] Jefferson T, Kelly C J, Martina M. Differential rearrangement of excitatory inputs to the medial prefrontal cortex in chronic pain models[J]. Front Neural Circuits, 2021, 15: 791043. doi: 10.3389/fncir.2021.791043 [18] Faria V, Ahs F, Appel L, et al. Amygdala-frontal couplings characterizing SSRI and placebo response in social anxiety disorder[J]. Int J Neuropsychopharmacol, 2014, 17(8): 1149-1157. doi: 10.1017/S1461145714000352 [19] Presto P, Mazzitelli M, Junell R, et al. Sex differences in pain along the neuraxis[J]. Neuropharmacology, 2022, 210: 109030. doi: 10.1016/j.neuropharm.2022.109030 [20] Bautista-Abad Á, García-Magro N, Pinto-Benito D, et al. Aging is associated with sex-specific alteration in the expression of genes encoding for neuroestradiol synthesis and signaling proteins in the mouse trigeminal somatosensory input[J]. Geroscience, 2024, 46(6): 6459-6472. doi: 10.1007/s11357-024-01268-z [21] Ferrari E, Cravello L, Muzzoni B, et al. Age-related changes of the hypothalamic-pituitary-adrenal axis: Pathophysiological correlates[J]. Eur J Endocrinol, 2001, 144(4): 319-329. doi: 10.1530/eje.0.1440319 [22] Pinto S M, Cheung J P Y, Samartzis D, et al. Are morphometric and biomechanical characteristics of lumbar multifidus related to pain intensity or disability in people with chronic low back pain after considering psychological factors or insomnia?[J]. Front Psychiatry, 2022, 13: 809891. doi: 10.3389/fpsyt.2022.809891 [23] Zheng P, Scheffler A, Ewing S, et al. Chronic low back pain causal risk factors identified by Mendelian randomization: A cross-sectional cohort analysis[J]. Spine J, 2025, 25(6): 1154-1166. doi: 10.1016/j.spinee.2024.12.029 [24] Fatemeh G, Sajjad M, Niloufar R, et al. Effect of melatonin supplementation on sleep quality: A systematic review and meta-analysis of randomized controlled trials[J]. J Neurol, 2022, 269(1): 205-216. doi: 10.1007/s00415-020-10381-w [25] Cheng Z, Xiang Q, Wang J, et al. The potential role of melatonin in retarding intervertebral disc ageing and degeneration: A systematic review[J]. Ageing Res Rev, 2021, 70: 101394. doi: 10.1016/j.arr.2021.101394 [26] Maurer L F, Schneider J, Miller C B, et al. The clinical effects of sleep restriction therapy for insomnia: A meta-analysis of randomised controlled trials[J]. Sleep Med Rev, 2021, 58: 101493. doi: 10.1016/j.smrv.2021.101493 [27] Goudman L, De Smedt A, Jansen J, et al. Virtual reality to improve sleep quality in patients suffering from painful diabetic polyneuropathy: A proof of concept study[J]. J Clin Med, 2024, 13(23): 7163. doi: 10.3390/jcm13237163 -





 下载:
下载: