Construction of A Predictive Model for High-risk ISS Stage in Newly Diagnosed Multiple Myeloma Patients Based on Coagulation Indicators
-
摘要:
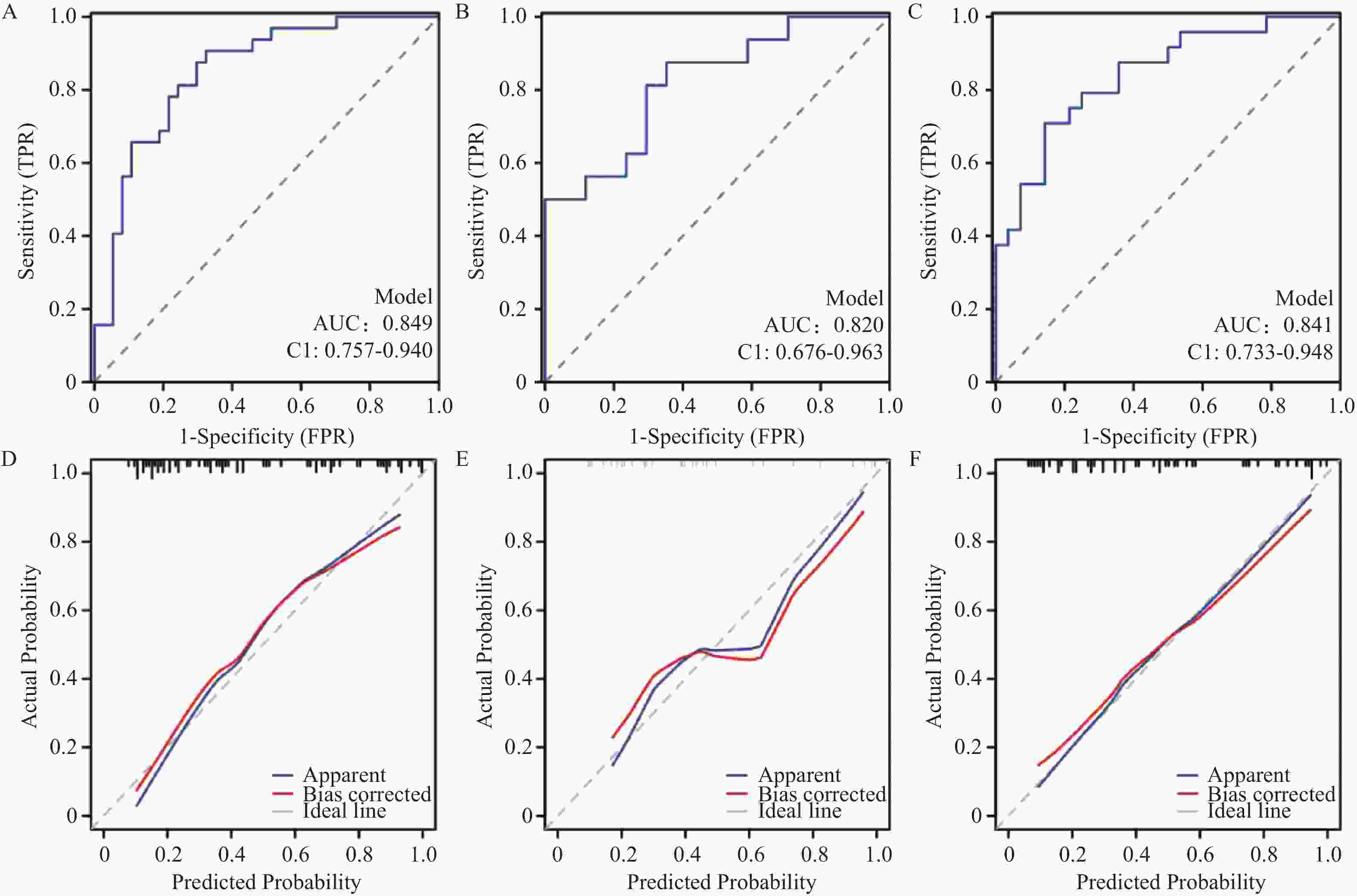
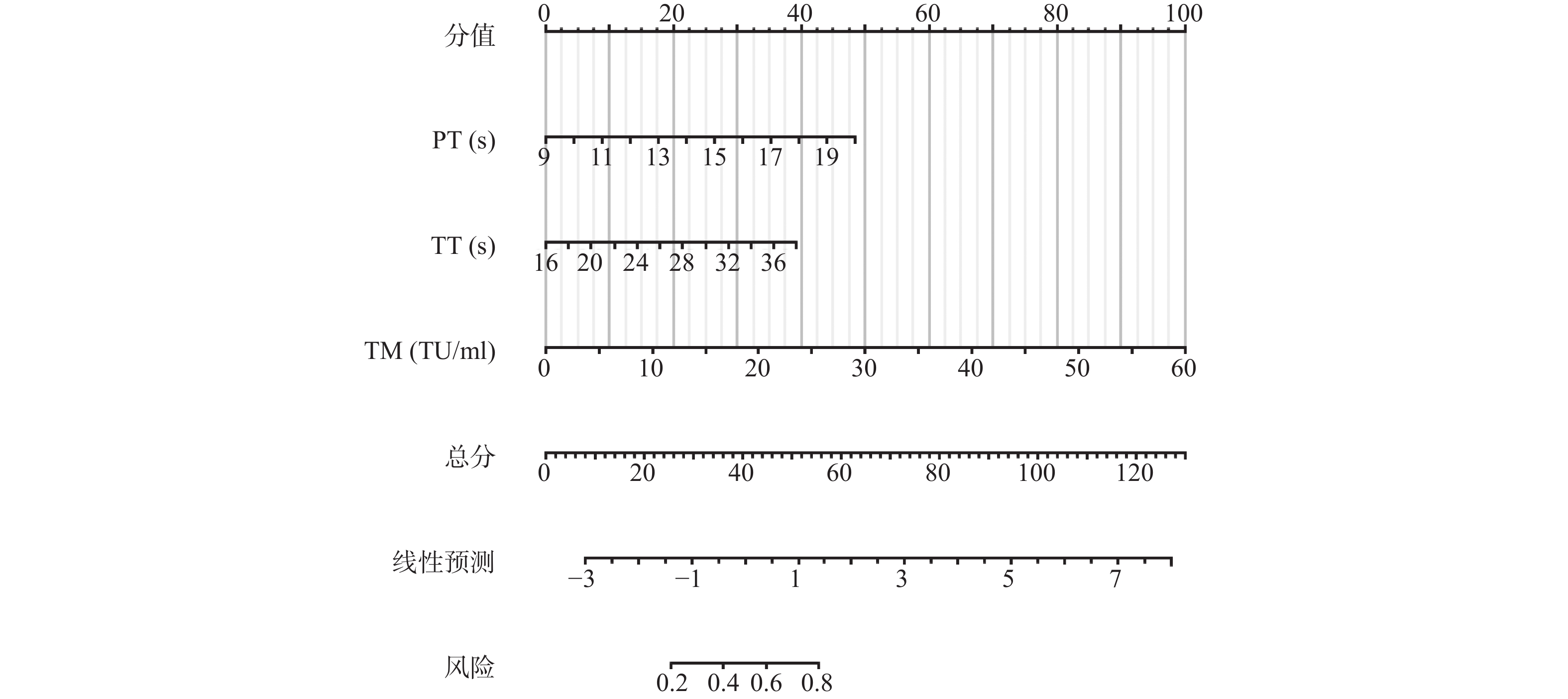
目的 探讨初诊多发性骨髓瘤(multiple myeloma,MM)患者凝血功能指标与国际分期系统(international staging system,ISS)分期的关系,建立以凝血指标为基础的ISS高危分期预测模型。 方法 收集2021年5月至2024年12月114例初诊MM患者作为模型开发队列,按7∶3比例随机分为训练集(80例)和内部验证集(34例);收集2025年1月至2025年6月52例患者作为外部验证队列。按照ISS分期将患者分成I/II期组和III期组,比较2组间凝血功能指标水平差异。利用Spearman相关分析评价各凝血指标与β2-微球蛋白(β2-microglobulin,β2-MG)、白蛋白(albumin,ALB)的相关性,通过二元Logistic回归法筛选出ISS高危分期的独立危险因素,构建列线图预测模型并评估其预测效能。 结果 ISS III期患者的凝血酶原时间(prothrombin time,PT)、活化部分凝血活酶时间(activated partial thromboplastin time,APTT)、纤维蛋白原含量(fibrinogen,FIB)、凝血酶时间(thrombin time,TT)和血栓调节蛋白(thrombomodulin,TM)水平均显著高于ISS I/II期患者(P < 0.05)。相关性分析显示,5项凝血功能指标均与β2-MG呈正相关,PT、APTT、TT与ALB呈负相关。多因素Logistic回归分析显示,PT、TT、TM是ISS高危分期的独立危险因素。基于PT、TT和TM构建的列线图预测模型显示AUC为0.849,敏感度90.6%,特异度67.6%。 结论 PT、TT和TM与ISS分期密切相关,可作为高危分期的独立危险因素。 Abstract:Objectives To investigate the correlation between coagulation function indicators and International Staging System (ISS) staging in newly diagnosed multiple myeloma (NDMM) patients, and to establish a predictive model for ISS high-risk staging based on coagulation indicators. Methods A total of 114 NDMM patients from May 2021 to December 2024 were collected as the model development cohort and randomly divided into training set (80 cases) and internal validation set (34 cases) at a ratio of 7∶3; 52 patients from January to June 2025 were collected as external validation cohort. Patients were stratified into stage I/II group and stage III group according to ISS staging, and differences in coagulation function indicators between the two groups were compared. Spearman correlation analysis was used to evaluate the correlations between coagulation indicators and β2-microglobulin (β2-MG) and albumin (ALB). Binary logistic regression was employed to identify independent risk factors for ISS high-risk staging, and a nomogram prediction model was constructed to assess its predictive performance. Results In ISS stage III patients, levels of prothrombin time (PT), activated partial thromboplastin time (APTT), fibrinogen (FIB), thrombin time (TT), and thrombomodulin (TM) were all significantly higher than those in ISS stage I/II patients (all P < 0.05). Correlation analysis showed that all five coagulation function indicators were positively correlated with β2-microglobulin, while PT, APTT, and TT were negatively correlated with albumin. Multivariate logistic regression analysis revealed that PT, TT, and TM were independent risk factors for ISS high-risk staging. The nomogram prediction model based on PT, TT, and TM showed an AUC of 0.849, with sensitivity of 90.6% and specificity of 67.6%. Conclusions PT, TT, and TM are closely associated with ISS staging and can serve as independent risk factors for high-risk staging. -
Key words:
- Multiple myeloma /
- Coagulation function /
- International staging system /
- Predictive model /
- Correlation
-
表 1 2组间基础资料比较[n(%)/M(P25,P75)]
Table 1. Comparison of basic clinical data between two groups [n(%)/M(P25,P75)]
项目 ISS I/II组(n=58) ISS III组(n=56) χ2/t/Z P 性别 1.989 0.158 男 33 (28.9) 39 (34.2) 女 25 (21.9) 17 (14.9) 年龄 (岁) 62.7 ± 8.7 64.3 ± 8.7 0.932 0.354 指标 PT (s) 11.9 (11.2, 12.8) 13.0 (12.0, 14.1) 3.974 <0.001 APTT (s) 28.9 (23.6, 35.0) 33.8 (28.4, 43.0) 2.916 0.004* FIB (g/L) 3.0 (2.5, 4.0) 2.6 (2.2, 3.6) 1.561 0.119 TT (s) 18.8 (17.7, 19.9) 20.5 (18.8, 23.6) 3.655 <0.001 FDP (mg/L) 4.2 (2.3, 6.6) 6.2 (3.0, 8.7) 1.857 0.064 D-D (mg/L) 1.3 (0.8, 2.1) 2.2 (1.1, 4.0) 2.069 0.039* TM (TU/mL) 7.2 (5.3, 9.7) 10.5 (6.3, 16.8) 3.319 0.001* TAT (ng/mL) 5.8 (4.0, 9.6) 5.5 (3.5, 7.2) 1.477 0.141 PIC (μg/mL) 0.7 (0.5, 1.5) 1.1 (0.6, 2.1) 1.530 0.127 t-PAIC (ng/L) 5.1 (4.0, 7.1) 5.6 (3.7, 10.1) 1.342 0.180 β2-MG(mg/L) 3.4 (2.7, 4.4) 13.4 (8.3, 19.5) 8.170 <0.001 ALB (g/L) 36.5 (30.4, 44.4) 34.5 (26.9, 38.3) 2.071 0.038* *P < 0.05。 表 2 凝血功能指标与β2-MG、ALB的相关性
Table 2. Correlation of coagulation function indicators with β2-MG and ALB
指标 β2-MG (mg/L) ALB (g/L) rS P rS P PT (s) 0.428 <0.001 −0.477 <0.001 APTT (s) 0.306 0.002* −0.325 0.001* TT (s) 0.327 0.001* −0.327 0.001* D-D (mg/L) 0.379 <0.001 −0.151 0.125 TM (TU/mL) 0.523 <0.001 0.031 0.756 注:数据均呈偏态分布,采用Spearman相关性分析;*P < 0.05。 表 3 凝血功能指标对ISS分期的多因素Logistic回归分析
Table 3. Logistic regression analysis of coagulation function indicators on ISS stages
指标 β SE Wald P OR 95%CI PT (s) 0.406 0.174 5.475 0.019* 1.501 1.068~2.109 TT (s) 0.165 0.088 3.495 0.062 1.179 0.992~1.402 TM
(TU/mL)0.154 0.051 9.020 0.003* 1.167 1.055~1.290 常量 −10.043 2.407 17.413 <0.001 0.000 − “−”表示无数据,TT的P值接近但未达到统计学显著性水平;*P < 0.05。 -
[1] Rajkumar S V. Multiple myeloma: 2024 update on diagnosis, risk-stratification, and management[J]. American J Hematol, 2024, 99(9): 1802-1824. doi: 10.1002/ajh.27422 [2] D’Agostino M, Cairns D A, Lahuerta J J, et al. Second revision of the international staging system (R2-ISS) for overall survival in multiple myeloma: A European myeloma network (EMN) report within the HARMONY project[J]. J Clin Oncol, 2022, 40(29): 3406-3418. doi: 10.1200/JCO.21.02614 [3] Ghansah H, Debreceni I B, Váróczy L, et al. Patients with multiple myeloma and monoclonal gammopathy of undetermined significance have variably increased thrombin generation and different sensitivity to the anticoagulant effect of activated protein C[J]. Thromb Res, 2023, 223(3): 44-52. [4] Papageorgiou L, Alhaj Hussen K, Thouroude S, et al. Modelization of blood-borne hypercoagulability in myeloma: A tissue-factor-bearing microparticle-driven process[J]. TH Open, 2019, 3(4): e340-e347. doi: 10.1055/s-0039-1700885 [5] Huang Y, Wang C, Wang H, et al. Rediscovering hemostasis abnormalities in multiple myeloma: The new era[J]. Heliyon, 2024, 10(13): 1-14. [6] Rajkumar S V, Dimopoulos M A, Palumbo A, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma[J]. Lancet Oncol, 2014, 15(12): e538-e548. doi: 10.1016/S1470-2045(14)70442-5 [7] 中国医师协会血液科医师分会, 中华医学会血液学分会. 中国多发性骨髓瘤诊治指南(2022年修订)[J]. 中华内科杂志, 2022, 61(5): 480-487. [8] Wang J H, Xiang P, Zhao E J, et al. Impact of type 2 and steroid-Induced diabetes mellitus on prognosis in patients with multiple myeloma[J]. World J Surg Oncol, 2025, 23(1): 1-10. doi: 10.1186/s12957-024-03642-9 [9] Mohan Lal B, Rhee F V, Al Hadidi S. Current state of evidence on definitions and management of high-risk multiple myeloma[J]. Curr Oncol Rep, 2025, 27(3): 258-277. doi: 10.1007/s11912-025-01639-5 [10] Hu M, Ma Y, Jia K, et al. Analysis of coagulation alteration and its correlation with β2-microglobulin in 371 patients with newly diagnosed multiple myeloma[J]. Hematology, 2024, 29(1): 1-8. [11] Martini F, Cecconi N, Paolicchi A, et al. Interference of monoclonal gammopathy with fibrinogen assay producing spurious dysfibrinogenemia[J]. TH Open, 2019, 3(1): e64-e66. doi: 10.1055/s-0039-1683969 [12] Geng C, Yang G, Wang H, et al. The prognostic role of prothrombin time and activated partial thromboplastin time in patients with newly diagnosed multiple myeloma[J]. Biomed Res Int, 2021, 2021(5): 1-9. [13] Melaccio A, Reale A, Saltarella I, et al. Pathways of angiogenic and inflammatory cytokines in multiple myeloma: Role in plasma cell clonal expansion and drug resistance[J]. J Clin Med, 2022, 11(21): 1-20. [14] Zhang T, Lin Z, Zheng Z, et al. Prognostic significance of β2-microglobulin decline index in multiple myeloma[J]. Front Oncol, 2024, 14(3): 1-10. [15] Cai Y, Zhao Y, Dai Q, et al. Prognostic value of the albumin-globulin ratio and albumin-globulin score in patients with multiple myeloma[J]. J Int Med Res, 2021, 49(3): 1-12. [16] Carlisi M, Lo Presti R, Mancuso S, et al. Calculated whole blood viscosity and albumin/fibrinogen ratio in patients with a new diagnosis of multiple myeloma: Relationships with some prognostic predictors[J]. Biomedicines, 2023, 11(3): 1-11. [17] Shen H, Wu C, Chen L, et al. Acquired heparin-like anticoagulation process in a patient with multiple myeloma: A case report and literature review[J]. Transl Cancer Res, 2020, 9(11): 7366-7371. doi: 10.21037/tcr-20-1968 [18] Pandey S, Post S R, Alapat D V, et al. Prolonged prothrombin time correlates with serum monoclonal protein concentration in patients with plasma cell dyscrasia[J]. Int J Lab Hematol, 2013, 35(4): 421-427. doi: 10.1111/ijlh.12036 [19] Zaharia A L, Tutunaru D, Oprea V D, et al. Thrombomodulin serum levels-a predictable biomarker for the acute onset of ischemic stroke[J]. Curr Issues Mol Biol, 2024, 46(1): 677-688. doi: 10.3390/cimb46010044 [20] Liu L, Qu J, Dai Y, et al. An interactive nomogram based on clinical and molecular signatures to predict prognosis in multiple myeloma patients[J]. Aging, 2021, 13(14): 18442-18463. doi: 10.18632/aging.203294 -





 下载:
下载: