Weight Gain Pattern during Pregnancy and Its Association with Delivery Fear and Cesarean Section Rate in Primiparous Women
-
摘要:
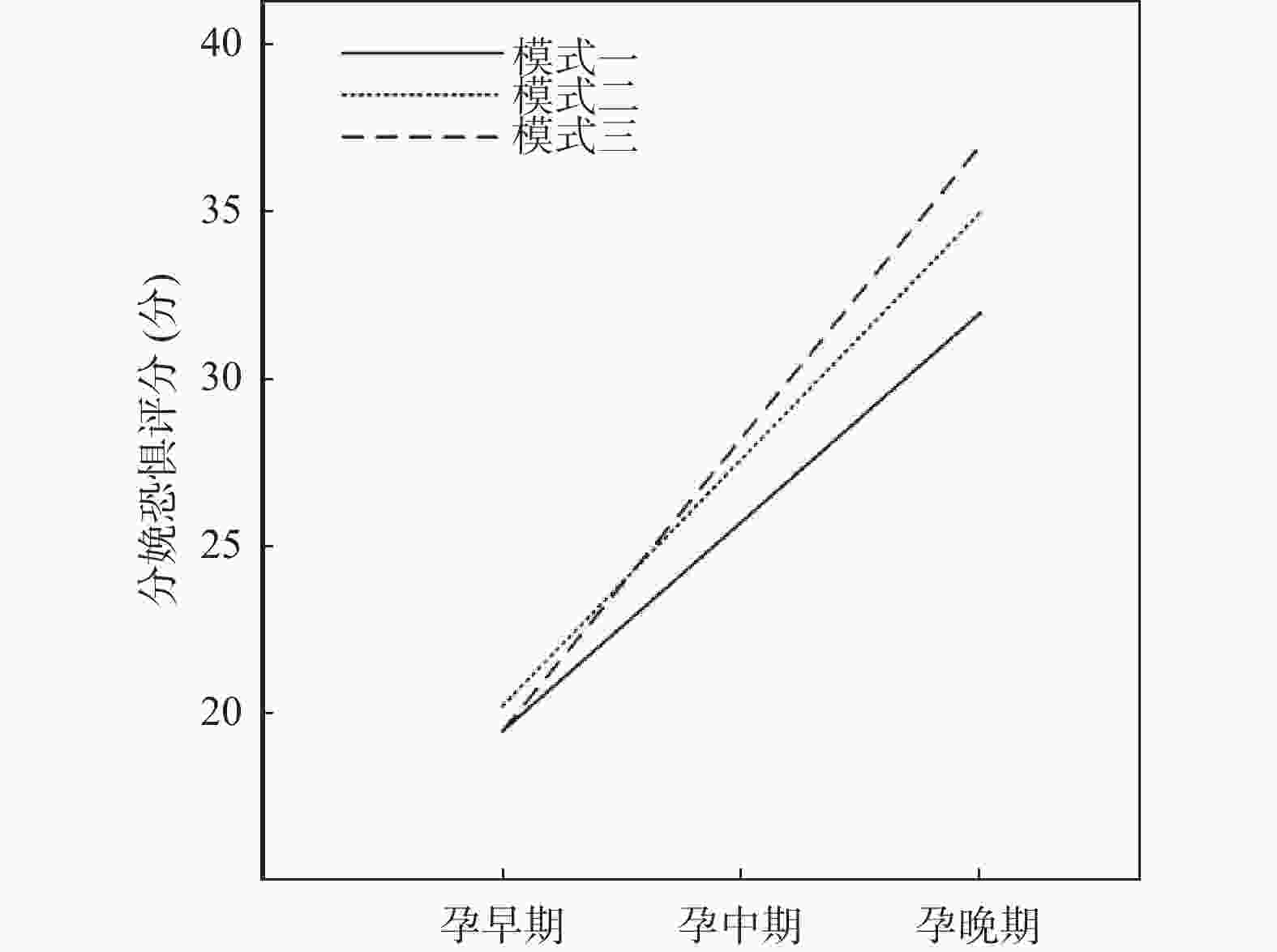
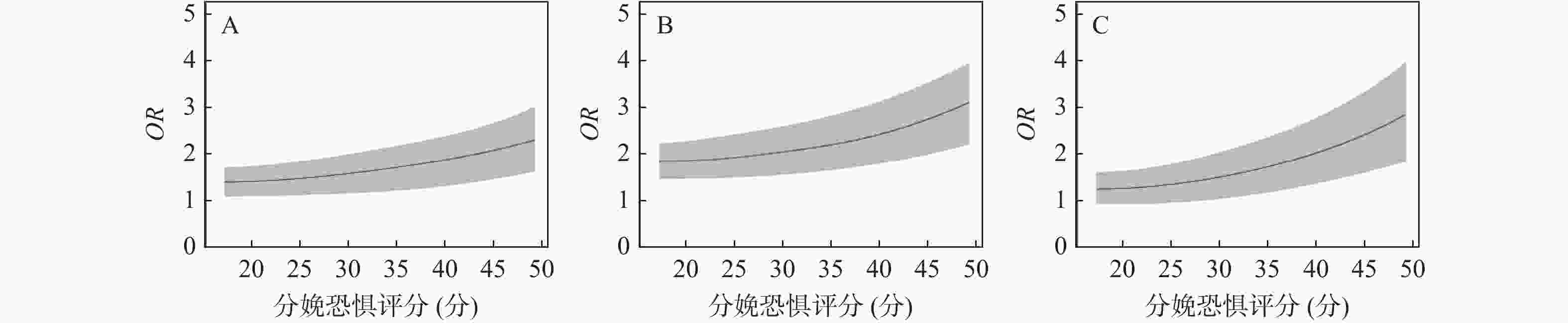
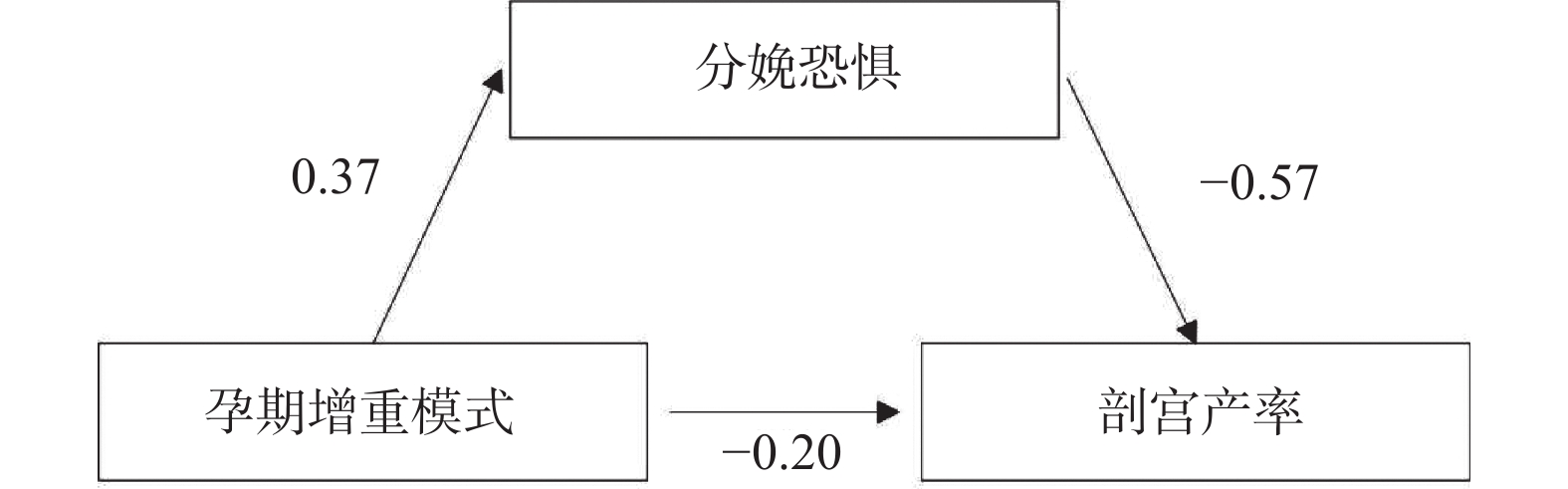
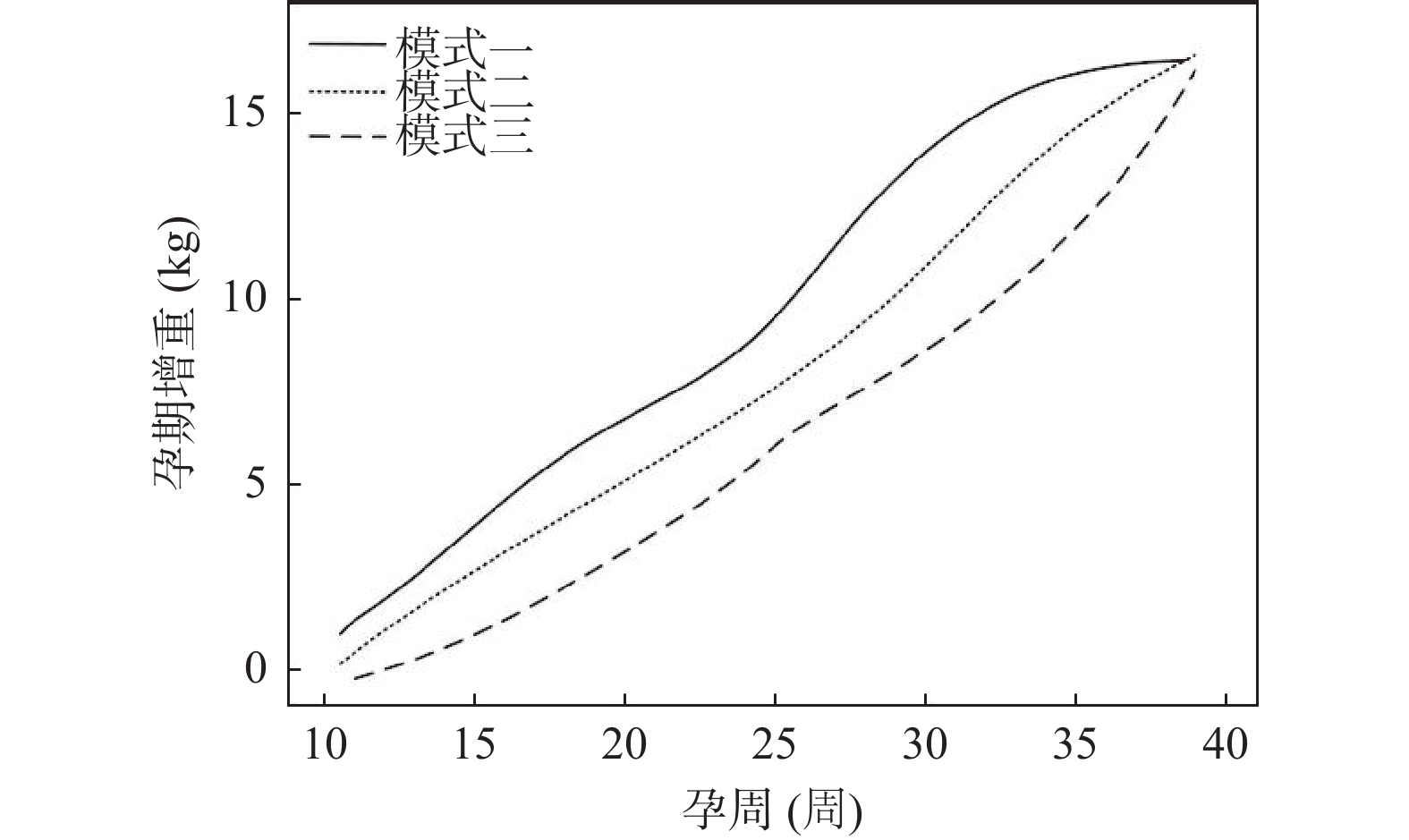
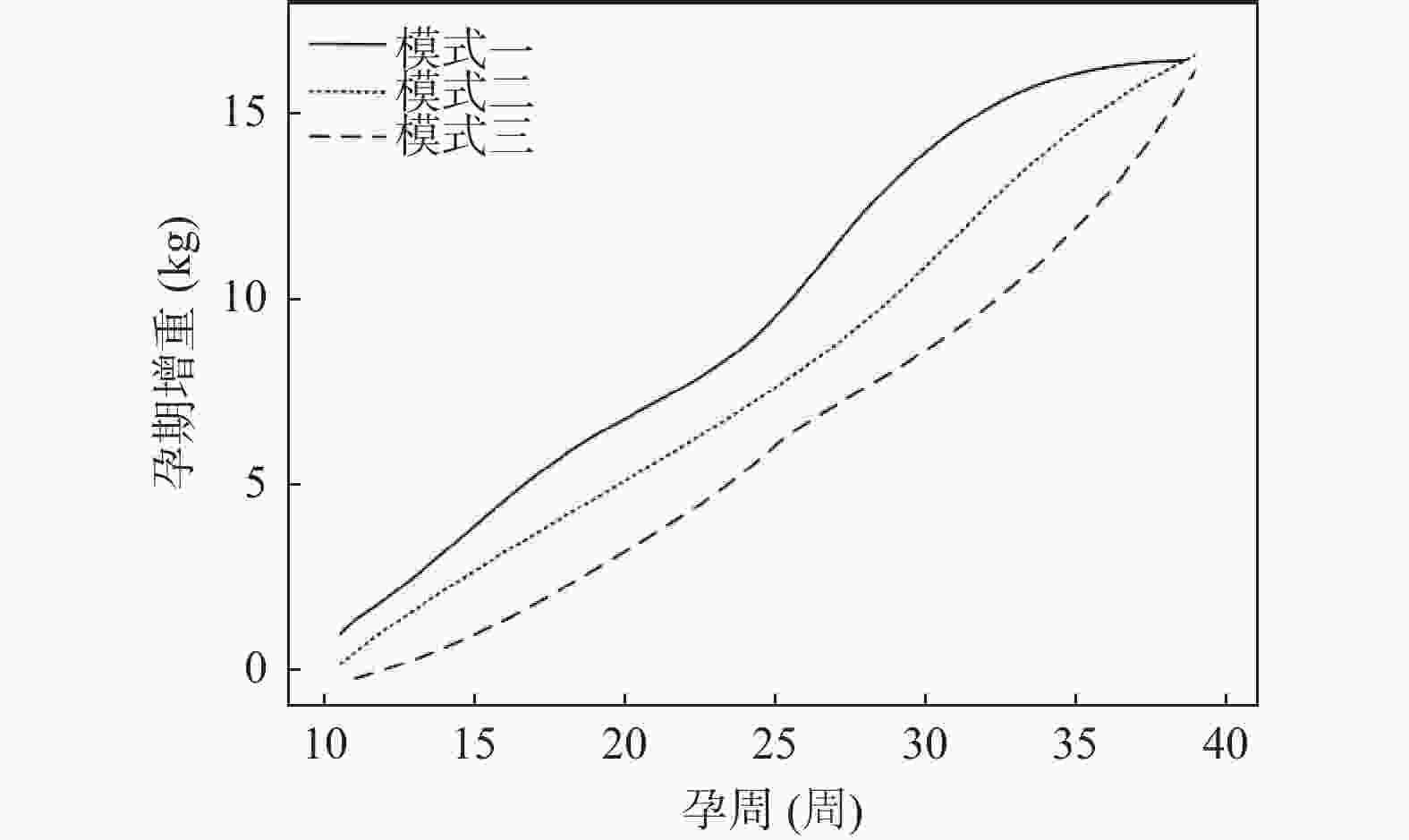
目的 探究孕期体重增长模式与初产孕妇分娩恐惧的关联以及分娩恐惧对孕期增重模式与剖宫产率的中介作用。 方法 选取2024年3月至2025年3月间于平凉市妇幼保健院分娩的242名孕妇作为研究对象,借助潜变量增长混合模型(LGMM)鉴别研究对象的孕期增重模式。多分类Logistic回归分析不同孕期增重模式的影响因素。比较不同孕期增重模式及不同分娩恐惧下的剖宫产率差异。限制性立方样条(RCS)分析分娩恐惧评分与不同孕期增重模式下选择剖宫产的关系。中介效应模型探究分娩恐惧对孕期增重模式与剖宫产率的中介作用。比较不同孕期增重模式孕妇的妊娠并发症及不良妊娠结局发生率。采用Log-binomial模型估计孕期增重模式与妊娠并发症的关联。 结果 LGMM模型在研究对象中确定了3种孕期增重模式:模式一为孕中期加速增重模式(n = 60);模式二为平稳加速增重模式(n = 98);模式三为孕晚期加速增重模式(n = 84)。多分类Logistic回归分析结果显示:以模式一、模式二为参考,孕前BMI高、年龄低、分娩恐惧评分高和孕前锻炼少更易出现孕期增重模式三(P < 0.05)。模式三增重模式的孕妇在分娩恐惧得分≥40分下,剖宫产人数占比最多(36.90%)。RCS曲线分析结果显示,分娩恐惧评分与三种孕期增重模式下选择剖宫产呈明显正相关。中介效应模型显示:分娩恐惧在孕期增重模式和剖宫产率中起部分中介效应,且中介效应占总效应的百分比为48.72%。模式一增重模式孕妇的妊娠期高血压和妊娠期糖尿病人数明显低于模式二、模式三增重模式(P < 0.05)。Log-binomial模型显示,孕期增重模式对妊娠并发症始终呈现明显影响(P < 0.05)。 结论 在不同孕期增长模式下,分娩恐惧评分均与选择剖宫产呈正相关;孕晚期加速增重模式初产孕妇的分娩恐惧得分更高,提示孕晚期孕妇应注重体重管理。 Abstract:Objective To examine the association between gestational weight gain patterns and childbirth fear in primiparous women, as well as the mediating effect of childbirth fear on the connection between gestational weight gain patterns and cesarean section rates. Methods A total of 242 pregnant women who delivered in Pingliang Maternal and Child Health Hospital from March 2024 to March 2025 were selected as the study subjects. Latent growth mixed model (LGMM) was used to identify the gestational weight gain patterns of the subjects. Multivariate Logistic regression was employed to analyze the influencing factors of various pregnancy weight gain patterns. The cesarean section rates were compared across different weight gain patterns and levels of childbirth fear. Restricted cubic splines (RCS) were used to analyze the relationship between fear of childbirth score and cesarean section selection under different gestational weight gain patterns. A mediating effect model was applied to investigate the mediating effect of fear of childbirth on gestational weight gain patterns and cesarean section rate. The incidence of pregnancy complications and adverse pregnancy outcomes in women with different weight gain patterns was compared. A Log-binomial model was used to estimate the association between gestational weight gain patterns and pregnancy complications. Results The LGMM model identified three patterns of gestational weight gain among the study subjects: Pattern I was characterized by mid-pregnancy accelerated weight gain (n = 60); Pattern II was defined as a steady accelerated weight gain pattern (n = 98); and Pattern III was identified as a late-pregnancy accelerated weight gain pattern (n = 84). Multinomial logistic regression analysis indicated that, compared to Patterns I and II, higher pre-pregnancy BMI, younger age, higher childbirth fear scores, and lower pre-pregnancy exercise levels were more likely to lead to Pattern III weight gain (P < 0.05). Among women with Pattern III weight gain, those with childbirth fear scores ≥40 exhibited the highest proportion of cesarean sections (36.90%). RCS curve analysis revealed a significant positive correlation between childbirth fear scores and cesarean section rates across the three gestational weight gain patterns. The mediation effect model demonstrated that childbirth fear played a partial mediating role between gestational weight gain patterns and cesarean section rates, with the mediation effect accounting for 48.72% of the total effect. Women with Pattern I weight gain experienced significantly fewer cases of gestational hypertension and gestational diabetes compared to those with Patterns II and III (P < 0.05). The Log-binomial model indicated that gestational weight gain patterns consistently had a significant impact on pregnancy complications (P < 0.05). Conclusion Under different growth patterns during pregnancy, the fear of childbirth scores were all positively correlated with the choice of cesarean section. For primiparous pregnant women with an accelerated weight gain pattern in the late pregnancy stage, their fear of childbirth scores were higher, suggesting that pregnant women in the late stage of pregnancy should pay attention to weight management. -
Key words:
- Pregnant women /
- Fear of childbirth /
- Weight /
- Cesarean section /
- Mediating effect
-
表 1 CAQ问题
Table 1. CAQ questions
编号 问题 问题1 害怕分娩时失去控制 问题2 害怕分娩的过程 问题3 做过关于分娩的噩梦 问题4 害怕分娩时出血过多 问题5 害怕在分娩过程中的知所措 问题6 害怕分娩过程中孩子会出现一些意外 问题7 害怕注射引起的疼痛 问题8 害怕独自面对分娩过程 问题9 害怕阴道分娩不顺利,最后还得进行剖宫产 问题10 害怕孩子的产出过程造成产道撕裂伤 问题11 害怕分娩过程中孩子受伤害 问题12 害怕子宫收缩引起的疼痛 问题13 想到即将来临的分娩就很难放松下来 问题14 害怕医院的环境 问题15 害怕得不到我想要的照顾 表 2 潜变量增长回合模型参数
Table 2. Latent variable growth round model parameters
分组数目 BIC 各组占比(%) 各组后验概率均值 1 145866.2 100 na. 2 144952.6 47.50,52.5 0.89,0.89 3 141002.1 24.79,40.50,34.71 0.84,0.85,0.85 4 135896.2 25.66,25.64,30.20,18.50 0.77,0.78,0.80,0.79 5 134420.9 35.40,36.80,12.0,9.30,6.50 0.73,0.71,0.72,0.75,0.74 6 132549.0 4.70,36.10,29.60,14.00,7.50,8.10 0.69,0.70,0.70,0.69,0.68,0.71 表 3 各增重模式的阶段性增速($\bar x \pm s $,kg/周)
Table 3. Phasic increases in each pattern of weight gain($\bar x \pm s $,kg/week)
阶段 模式一(n=60) 模式二(n=98) 模式三(n=84) 孕早期 0.20 ± 0.05 0.35 ± 0.04 0.15 ± 0.05 孕中期 0.72 ± 0.16 0.40 ± 0.15 0.53 ± 0.16 孕晚期 0.32 ± 0.14 0.44 ± 0.13 0.69 ± 0.17 表 4 不同体重增长模式组的基本资料比较[$\bar x \pm s $/n(%)]
Table 4. Comparison of basic data of different weight gain pattern groups[$\bar x \pm s $/n(%)]
基本特征 模式一(n=60) 模式二(n=98) 模式三(n=84) F/χ2 P 孕前BMI(kg/m2) 20.71 ± 1.63 20.40 ± 1.49 21.03 ± 1.60b 3.673 0.027* 身高(cm) 162.05 ± 2.31 162.42 ± 2.29 162.35 ± 2.25 0.516 0.598 年龄(岁) 28.61 ± 3.12 27.95 ± 3.05 27.33 ± 3.02a 3.091 0.047* 孕周(周) 39.6 ± 1.01 39.7 ± 1.02 39.7 ± 1.01 0.219 0.803 孕期总增重(kg) 16.59 ± 2.35 15.58 ± 3.02 16.37 ± 3.14 2.770 0.065 出生体重(kg) 3.41 ± 0.35 3.35 ± 0.40 3.30 ± 0.41 1.382 0.253 出生身长(cm) 50.51 ± 1.20 50.35 ± 1.13 50.20 ± 1.10 1.310 0.272 分娩恐惧评分(分) 32.25 ± 7.02 35.02 ± 6.59a 36.71 ± 7.19a 7.308 0.001* 教育水平 0.289 0.865 大专及以下 32(53.33) 50(51.02) 41(48.81) 本科及以上 28(46.67) 48(48.98) 43(51.19) 家庭人均月收入(元) 1.044 0.593 < 5000 25(41.67) 42(42.86) 30(35.71) ≥ 5000 35(58.33) 56(57.14) 54(64.29) 睡眠时长(h) 4.329 0.363 <7 4(6.67) 5(5.10) 5(5.95) 7~9 54(90.00) 87(88.78) 69(82.14) >9 2(3.33) 6(6.12) 10(11.90) 孕前锻炼 26.016 <0.001* 是 38(63.33) 27(27.55)a 22(26.19)a 否 22(36.67) 71(72.45)a 62(73.81)a 婴儿性别 0.105 0.949 男 33(55.00) 53(54.08) 44(52.38) 女 27(45.00) 45(45.92) 40(47.62) 吸烟史 0.114 0.944 是 5(8.33) 7(7.14) 7(8.33) 否 55(91.67) 91(92.86) 77(91.67) 饮酒史 0.011 0.994 是 3(5.00) 5(5.10) 4(4.76) 否 57(95.00) 93(94.90) 80(95.24) 符合剖宫产指征 0.249 0.883 是 11(18.33) 15(15.31) 14(16.67) 否 49(81.67) 83(84.69) 70(83.33) 是否剖宫产 7.006 0.030* 是 21(35.00) 34(34.69) 44(52.38)ab 否 39(65.00) 64(65.31) 40(47.62)ab *P < 0.05;与模式一比较,aP < 0.05;与模式二比较,bP < 0.05。 表 5 Logistic回归分析不同孕期增重模式的影响因素
Table 5. Logistic regression analysis of influencing factors of different weight gain patterns during pregnancy
因变量 影响因素 β SE Wald χ2 P OR 95%CI 模式二vs.模式三 截距 44.555 8.567 27.048 <0.001* 孕前BMI 0.988 0.523 3.569 0.035* 2.686 2.335~2.968 年龄 −0.759 0.342 4.929 <0.001* 0.468 0.326~0.561 分娩恐惧评分 0.799 0.433 3.404 0.041* 2.223 1.815~2.597 孕前锻炼 −0.792 0.411 3.712 <0.001* 0.453 0.401~0.523 模式一vs.模式三 截距 59.881 20.553 8.488 <0.001* 孕前BMI 0.997 0.473 4.446 <0.001* 2.711 2.325~2.998 年龄 −0.631 0.333 3.592 <0.001* 0.532 0.331~0.748 分娩恐惧评分 0.857 0.487 3.096 <0.001* 2.356 2.114~2.523 孕前锻炼 −0.594 0.331 3.223 <0.001* 0.552 0.412~0.665 *P < 0.05。 表 6 不同孕期增重模式及不同分娩恐惧下的剖宫产人数[n(%)]
Table 6. Number of cesarean sections under different gestational weight gain patterns and different fear of childbirth [n(%)]
分娩恐惧评分(分) 模式一(n=60) 模式二(n=98) 模式三(n=84) χ2 P <28(无分娩恐惧) 8(13.33) 9(9.18) 5(5.95) 11.632 0.020* 28~39(轻度分娩恐惧) 6(10.00) 11(11.22) 8(9.52) ≥40(中度、高度分娩恐惧) 7(11.67) 14(14.29) 31(36.90) *P < 0.05。 表 7 分娩恐惧对孕期增重模式与剖宫产率的中介作用分析
Table 7. Mediating effect of fear of childbirth on gestational weight gain pattern and cesarean section rate
变量 模型1 模型2 模型3 β t P β t P β t P 孕期增重模式 −0.51 −5.01 <0.001* 0.44 3.58 <0.001* −0.33 −2.51 0.04* 分娩恐惧 - - - - - - −0.55 −3.96 <0.001* R2 0.78 0.45 0.88 F 18.23 6.85 28.99 注:(1)模型中各变量均采用标准化后的变量带入回归方程;(2)模型1为分娩恐惧预测剖宫产率;模型2为孕期增重模式预测剖宫产率;模型3为分娩恐惧和孕期增重模式共同预测剖宫产率;*P < 0.05,“-”表示无数据。 表 8 Bootstrap中介效应检验结果
Table 8. Bootstrap mediation effect test results
分类 效应值 标准误 Bootstrap 95%CI 占总效
应比率(%)下限 上限 总效应 −0.39 0.09 −0.56 −0.31 直接效应 −0.20 0.09 −0.41 −0.03 间接效应 −0.19 0.09 −0.44 −0.01 48.72 表 9 不同孕期增重模式孕妇的妊娠并发症及不良妊娠结局发生率比较
Table 9. Comparison of the incidence of pregnancy complications and adverse pregnancy outcomes among pregnant women with different weight gain patterns during different pregnancy periods
指标 分类 模式一(n=60) 模式二(n=98) 模式三(n=84) χ2 P 妊娠并发症 妊娠期高血压 3(5.00) 7(7.14) 14(16.67)ab 6.752 0.034* 妊娠期糖尿病 5(8.33) 9(9.18) 17(20.23)ab 6.380 0.041* 贫血 48(80.00) 78(79.59) 67(79.76) 0.004 0.998 胎位异常 1(1.67) 2(2.04) 3(3.57) 0.656 0.720 不良妊娠结局 早产 3(5.00) 7(7.14) 8(9.52) 1.061 0.588 胎儿畸形 1(1.67) 3(3.06) 3(3.57) 0.469 0.791 葡萄胎 0 1(1.02) 1(1.19) 0.681 0.711 胎儿发育异常 1(1.67) 2(2.04) 3(3.57) 0.656 0.720 *P < 0.05;与模式一比较,aP < 0.05;与模式二比较,bP < 0.05。 表 10 孕期增重模式对妊娠并发症的Log-binomial分析
Table 10. Log-binomial analysis of the weight gain pattern during pregnancy and its association with pregnancy complications
因素 模型一 模型二 模型三 RR 95%CI RR 95%CI RR 95%CI 模式一 1.00 1.00 1.00 模式二 3.08* 2.59~3.62 3.07* 2.47~3.71 3.05* 2.66~3.53 模式三 2.25* 1.98~2.56 2.24* 2.04~2.45 2.23* 1.88~2.52 注:模型一不控制协变量;模型二控制的协变量为BMI、孕周、身高、孕期总增重、年龄、分娩方式和教育水平;模型三控制的协变量为BMI、孕周、身高、孕期总增重、年龄、分娩方式、教育水平、家庭人均月收入、睡眠时长、吸烟史、孕前锻炼、饮酒史和是否符合剖宫产指征;*P < 0.05。 -
[1] Gibson M E. Pain relief during childbirth in the context of 50 years of social and technological change[J]. J Obstet Gynecol Neonatal Nurs, 2021, 50(4): 369-381. doi: 10.1016/j.jogn.2021.04.004 [2] Dai J, Shi Y, Guo L, et al. Discrepancy in parental fear of childbirth: A scoping review[J]. Midwifery, 2023, 126: 103830. doi: 10.1016/j.midw.2023.103830 [3] Moran E, Bradshaw C, Tuohy T, et al. The paternal experience of fear of childbirth: An integrative review[J]. Int J Environ Res Public Health, 2021, 18(3): 1231. doi: 10.3390/ijerph18031231 [4] Bernardo D S, Carvalho C B, Conde M, et al. Effectiveness of a structured exercise intervention in gestational weight gain in pregnant women with overweight and obesity: A systematic review with meta-analysis[J]. Int J Gynaecol Obstet, 2023, 162(3): 811-822. doi: 10.1002/ijgo.14741 [5] Aung W, Saw L, Sweet L. An integrative review of interventions for limiting gestational weight gain in pregnant women who are overweight or obese[J]. Women Birth, 2022, 35(2): 108-126. doi: 10.1016/j.wombi.2021.04.009 [6] Erdősová A, Gašparová P, Ballová Z, et al. Caesarean section on request - a controversial request or the patient's right[J]? Ceska Gynekol, 2024, 89(3): 245-252. [7] 缑彦军, 葛玲燕. 高龄产妇剖宫产产后出血危险因素分析及预测模型构建[J]. 中国妇幼保健, 2025, 40(11): 2076-2079. [8] 王鹏, 甘玉杰, 彭学鸣, 等. 围产儿死亡的影响因素及其干预对策[J]. 广东医学, 2025, 46(05): 759-764. [9] 王洁洁. 初产妇自然分娩情况及影响因素分析[J]. 中国妇幼保健, 2021, 36(6): 1371-1373. [10] 钱静, 杨柳, 邓秀敏, 等. 妊娠早期孕妇分娩恐惧现状及影响因素分析[J]. 中国妇幼保健, 2025, 40(12): 2247-2251. [11] Mei X, Du P, Li Y, et al. Fear of childbirth and sleep quality among pregnant women: A generalized additive model and moderated mediation analysis[J]. BMC Psychiatry, 2023, 23(1): 931. doi: 10.1186/s12888-023-05435-y [12] 王菲, 王蓉, 翁惠婷, 等. 围产期妇女分娩恐惧的潜在剖面分析及影响因素研究[J]. 护理学报, 2025, 32(10): 1-6. [13] Kelly N M, Keane J V, Gallimore R B, et al. Neonatal weight loss and gain patterns in caesarean section born infants: Integrative systematic review[J]. Matern Child Nutr, 2020, 16(2): e12914. doi: 10.1111/mcn.12914 [14] Frampton S. Caesarean section: The history of a controversial operation[J]. Lancet, 2024, 403(10441): 2282-2283. doi: 10.1016/S0140-6736(24)01038-9 [15] Shrestha D B , Budhathoki P , Shrestha O, et al. Teenage pregnancy and associated risk factors and outcome in Nepal from 2000-2020: A systematic review and meta-analysis[J]. Kathmandu Univ Med J (KUMJ), 2022, 20(78): 225-233.Shrestha D B , Budhathoki P , Shrestha O, et al. Teenage pregnancy and associated risk factors and outcome in Nepal from 2000-2020: A systematic review and meta-analysis[J]. Kathmandu Univ Med J (KUMJ), 2022, 20(78): 225-233. [16] Sharp M, Ward L G, Solar C, et al. Internalized weight bias, weight-related experiences, and peripartum weight[J]. J Midwifery Womens Health, 2023, 68(4): 490-498.Sharp M, Ward L G, Solar C, et al. Internalized weight bias, weight-related experiences, and peripartum weight[J]. J Midwifery Womens Health, 2023, 68(4): 490-498. [17] 段婵芝, 李青, 孙恬, 等. 女性分娩恐惧相关因素的系统评价[J]. 中国妇幼保健, 2025, 40(12): 2320-2324. [18] Akgün M, Boz İ, Özer Z. The effect of psychoeducation on fear of childbirth and birth type: Systematic review and meta-analysis[J]. J Psychosom Obstet Gynaecol, 2020, 41(4): 253-265. doi: 10.1080/0167482X.2019.1689950 [19] Lin L, Lin J, Mao X, et al. Gestational weight gain charts for twin pregnancies in Southeast China[J]. BMC Pregnancy Childbirth, 2020, 20(1): 127. doi: 10.1186/s12884-020-2761-1 [20] Morisaki N, Piedvache A, Morokuma S, et al. Gestational weight gain growth charts adapted to Japanese pregnancies using a bayesian approach in a longitudinal study: The Japan environment and children's study[J]. J Epidemiol, 2023, 33(5): 217-226. doi: 10.2188/jea.JE20210049 [21] Dachew B A, Ayano G, Betts K, et al. The impact of pre-pregnancy BMI on maternal depressive and anxiety symptoms during pregnancy and the postpartum period: A systematic review and meta-analysis[J]. J Affect Disord, 2021, 281: 321-330. doi: 10.1016/j.jad.2020.12.010 [22] Alizadeh-Dibazari Z, Abdolalipour S, Mirghafourvand M. The effect of prenatal education on fear of childbirth, pain intensity during labour and childbirth experience: A scoping review using systematic approach and meta-analysis[J]. BMC Pregnancy Childbirth, 2023, 23(1): 541. doi: 10.1186/s12884-023-05867-0 -





 下载:
下载: