Predictive Ability of Platelet Reactivity,ROCK1 Combined with Electrocardiogram Findings for Slow Blood Flow/No Reflow in Elderly Patients after PCI
-
摘要:
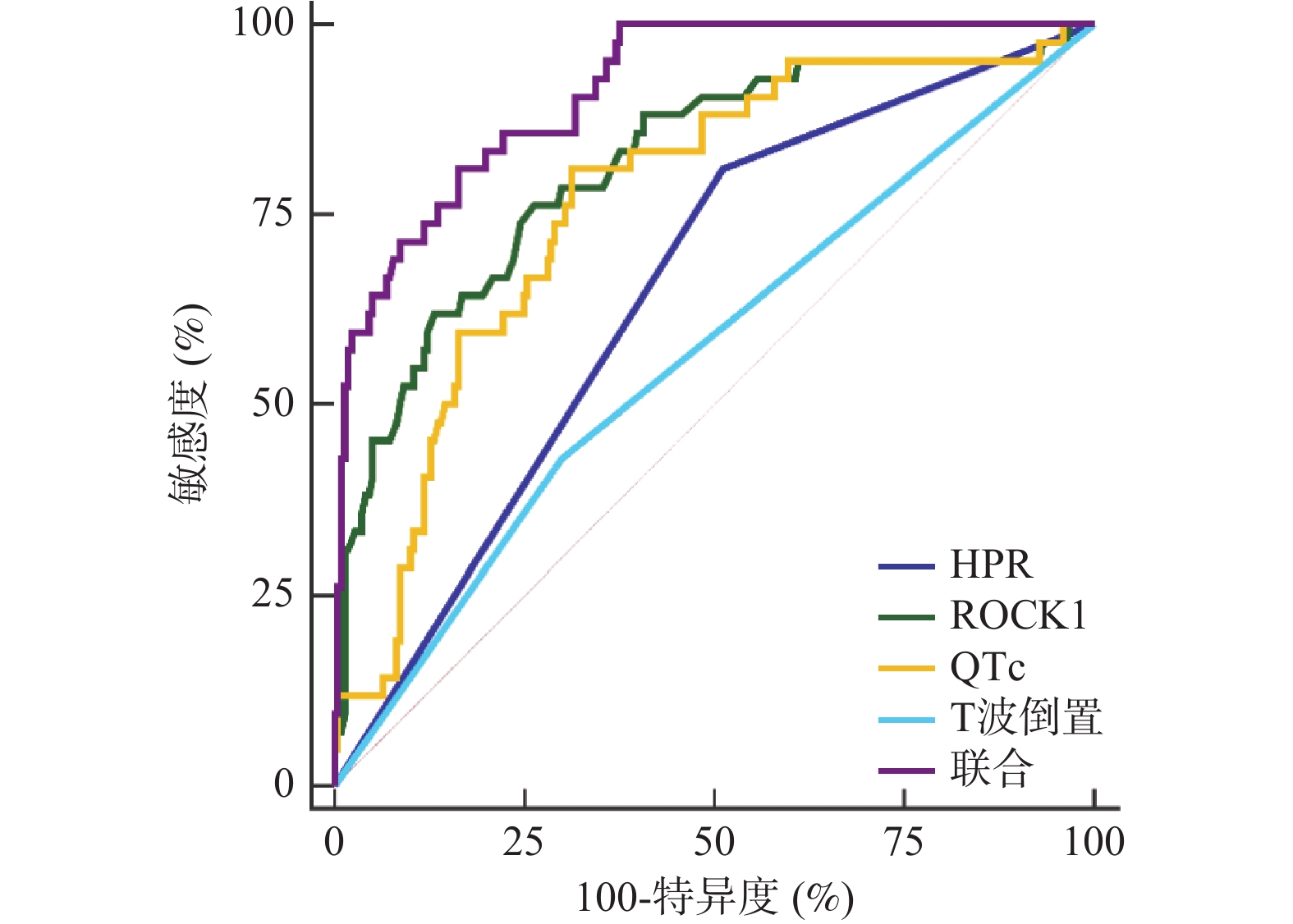
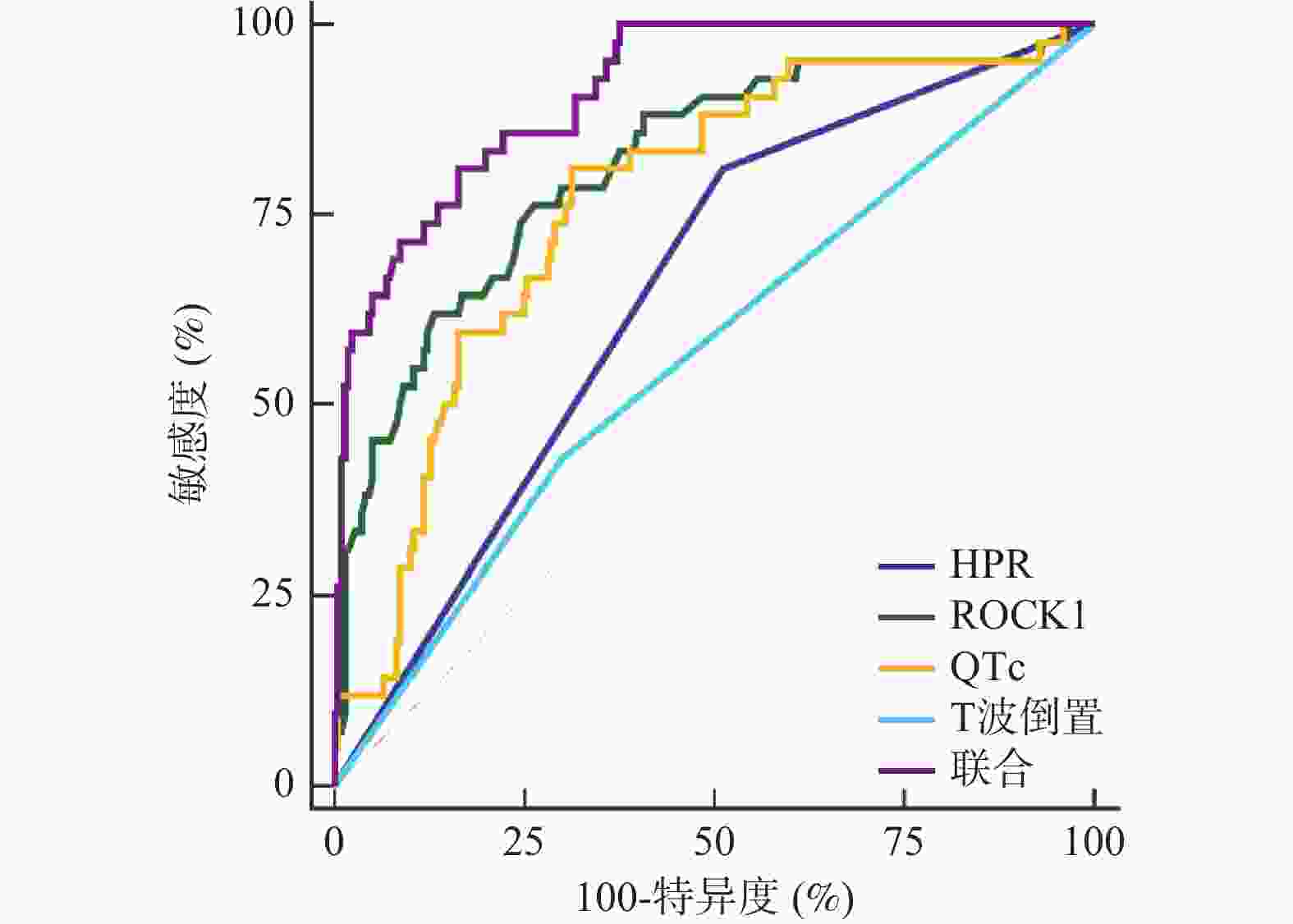
目的 探究血小板反应性、RhoC和Rho激酶1联合心电图表现对老年经皮冠状动脉介入治疗术(PCI)后慢血流/无复流(SF/NRF)的预测价值。 方法 回顾性分析张家口市第一医院2021年1月至2024年7月收治的263例老年PCI患者的临床资料,根据PCI后TIMI血流分级分为SF/NRF组42例(TIMI分级0~Ⅱ级)、对照组221例(TIMI分级Ⅲ级)。比较两组基线资料及血小板反应性、ROCK1、心电图表现。分析老年PCI后SF/NRF的影响因素。评价联合预测因子、各原始协变量预测老年PCI后SF/NRF的价值。 结果 SF/NRF组HPR患者占比、ROCK1、QTc、T波倒置患者占比高于对照组(P < 0.05);HPR、ROCK1升高、QTc升高、T波倒置是老年PCI后SF/NRF的独立危险因素(P < 0.05);联合预测因子预测老年PCI后SF/NRF的AUC显著高于原始协变量HPR(X1)、ROCK1(X2)、QTc(X3)、T波倒置(X4)(Z = 5.112、3.688、4.368、5.697,P < 0.05)。 结论 HPR、ROCK1升高、QTc升高、T波倒置是老年PCI后SF/NRF的独立危险因素,联合检测上述指标对老年PCI后SF/NRF发生具有一定预测价值。 -
关键词:
- 老年 /
- 经皮冠状动脉介入治疗术 /
- 慢血流/无复流 /
- 血小板反应性 /
- RhoC和Rho激酶1 /
- 预测
Abstract:Objective To investigate the predictive value of platelet reactivity, RhoC and Rho kinase 1 (ROCK1) combined with the electrocardiogram performance for slow flow/no reflow (SF/NRF) after the percutaneous coronary intervention (PCI) in elderly patients. Methods A retrospective analysis was conducted on the clinical data of 263 elderly PCI patients admitted to our hospital from January 2021 to July 2024. According to TIMI flow classification after PCI, they were divided into SF/NRF group (grade 0-II of TIMI flow classification, 42 cases) and the control group (grade III of TIMI flow classification, 221 cases). The baseline data and platelet reactivity, ROCK1, and ECG performance were compared between the two groups and the factors influencing SF/NRF after PCI in the elderly were analyzed. The value of joint predictors, each original covariate to predict SF/NRF after PCI in the elderly was evaluated. Results The proportion of patients with HPR, ROCK1, QTc, and T-wave inversion in SF/NRF group was higher than that in the control group (P < 0.05); increased HPR, ROCK1, QTc, and T-wave inversion were independent risk factors for SF/NRF after PCI in the elderly (P < 0.05); the AUC of the combined predictors for predicting SF/NRF after PCI in the elderly was significantly higher than that of the original covariates HPR (X1), ROCK1 (X2, QTc (X3), and T-wave inversion (X4) (Z = 5.112, 3.688, 4.368, 5.697, P < 0.05). Conclusion The increase of HPR, ROCK1, QTc and T wave inversion are independent risk factors for SF/NRF after PCI in the elderly. The combined detection of these indicators has certain predictive value for the occurrence of SF/NRF after PCI in the elderly. -
表 1 两组的基线资料比较[($ \bar x \pm s $)/n(%)]
Table 1. Comparison of baseline data between two groups[($ \bar x \pm s $)/n(%)]
资料 SF/NRF组(n=42) 对照组(n=221) t/χ2 P 年龄(岁) 66.74±2.17 67.02±2.11 0.785 0.433 性别 0.126 0.722 男 28(66.67) 141(63.80) 女 14(33.33) 80(36.20) 体质量指数(kg/m2) 24.25±0.60 24.19±0.72 0.507 0.612 糖尿病 18(42.86) 89(40.27) 0.098 0.755 高血压 15(35.71) 74(33.48) 0.078 0.779 高脂血症 24(57.14) 120(54.30) 0.115 0.734 病因 0.003 0.958 非ST段抬高型急性心肌梗死 23(54.76) 122(55.20) ST段抬高型急性心肌梗死 19(45.24) 99(44.80) 病变血管支数 0.009 0.924 单支 28(66.67) 149(67.42) ≥2支 14(33.33) 72(32.58) 靶血管 左前降支 25(59.52) 133(60.18) 0.006 0.936 旋支 14(33.33) 71(32.13) 0.023 0.878 左主干 9(21.43) 48(21.72) 0.002 0.967 右冠状动脉 12(28.57) 61(27.60) 0.017 0.898 发病至PCI时间(h) 4.26±1.38 4.09±1.29 0.774 0.440 Killip分级 0.008 0.929 <Ⅱ级 33(78.57) 175(79.19) ≥Ⅱ级 9(21.43) 46(20.81) 既往用药史 β受体阻滞剂 6(14.29) 29(13.12) 0.041 0.839 他汀类药物 18(42.86) 96(43.44) 0.005 0.944 双抗 11(26.19) 60(27.15) 0.016 0.898 AECI/ARB 10(23.81) 48(21.72) 0.090 0.765 表 2 两组HPR、ROCK1、QRS间期、QTc、PR间期、病理性Q波、T波倒置、ST段压低情况比较[n(%)/($ \bar x \pm s $)]
Table 2. Comparison of HPR,ROCK1,QRS interval,QTc,PR interval,pathological Q-wave,T-wave inversion,and ST-segment depression between two groups[n (%)/($ \bar x \pm s $)]
组别 n HPR ROCK1
(ng/mL)QRS间期
(ms)QTc
(ms)PR间期
(ms)病理性Q波 T波倒置 ST段压低 ST段抬高 SF/NRF组 42 34(80.95) 1.59±0.39 94.11±11.25 462.59±51.07 164.58±31.29 16(38.10) 24(57.14) 16(38.10) 19(45.24) 对照组 221 108(48.87) 1.20±0.28 92.89±10.76 421.38±46.25 161.90±29.75 78(35.29) 66(29.86) 80(36.20) 99(44.80) t 14.625 7.724 0.669 5.205 0.531 0.121 11.667 0.055 0.003 P <0.001* <0.001* 0.504 <0.001* 0.596 0.728 0.001* 0.815 0.958 *P < 0.05。 表 3 HPR(X1)、ROCK1(X2)、QTc(X3)、T波倒置(X4)联合预测老年PCI后SF/NRF的Logistic回归模型变量赋值
Table 3. Logistic regression model variable assignment of HPR (X1),ROCK1 (X2),QTc (X3),and T-wave inversion (X4) for joint prediction of SF/NRF after PCI in the elderly
影响因素 赋值 SF/NRF 否=0,是=1 HPR(X1) 否=0,是=1 ROCK1(X2) 按连续变量处理 QTc(X3) 按连续变量处理 T波倒置(X4) 否=0,是=1 表 4 HPR(X1)、ROCK1(X2)、QTc(X3)、T波倒置(X4)作为协变量预测老年PCI后SF/NRF的Logistic回归结果
Table 4. Logistic regression results of HPR (X1),ROCK1 (X2),QTc (X3),and T-wave inversion (X4) as covariates to predict SF/NRF after PCI in the elderly
影响因素 β SE Wald χ2 OR 95%CI P HPR(X1) 1.070 0.274 15.257 2.916 2.065~4.118 <0.001* ROCK1(X2) 0.134 0.042 10.162 1.143 1.103~1.185 <0.001* QTc(X3) 0.073 0.021 12.102 1.076 1.009~1.147 <0.001* T波倒置(X4) 0.798 0.311 6.586 2.221 1.642~3.005 0.031* 常数项 −0.284 0.067 17.926 0.753 − <0.001* *P < 0.05。 表 5 联合预测因子及各原始协变量预测老年PCI后SF/NRF的结果
Table 5. Results of predicting SF/NRF in elderly patients after PCI by combined predictive factors and various original covariates
指标 AUC 95%CI cut-off值 敏感度(%) 特异度(%) P HPR(X1) 0.649 0.588~0.707 是 80.95 78.87 <0.001* ROCK1(X2) 0.815 0.762~0.860 1.41 76.19 73.76 <0.001* QTc(X3) 0.767 0.711~0.817 461.81 80.95 68.78 <0.001* T波倒置(X4) 0.565 0.503~0.626 是 42.86 70.14 <0.001* 联合 0.914 0.873~0.945 0.154 80.95 83.71 <0.001* *P < 0.05。 -
[1] Xie E M,Li Q,Ye Z X,et al. Canada acute coronary syndrome risk score predicts no-/slow-reflow in ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention[J]. Heliyon,2023,9(11):e21276-e21286. doi: 10.1016/j.heliyon.2023.e21276 [2] Hu X M,Yang X,Li X D,et al. Elevated uric acid is related to the no-/slow-reflow phenomenon in STEMI undergoing primary PCI[J]. Eur J Clin Invest,2022,52(4):e13719-e13729. doi: 10.1111/eci.13719 [3] 尹江燕,聂倩文,郇轩,等. 血小板反应性对PCI术后远期心血管不良结局影响的研究进展[J]. 中国急救医学,2022,42(8):723-727. doi: 10.3969/j.issn.1002-1949.2022.08.013 [4] Sun T,Gong Q,Wu Y,et al. Dexmedetomidine alleviates cardiomyocyte apoptosis and cardiac dysfunction may be associated with inhibition of RhoA/ROCK pathway in mice with myocardial infarction[J]. Naunyn Schmiedebergs Arch Pharmacol,2021,394(7):1569-1577. doi: 10.1007/s00210-021-02082-6 [5] Flaherty D,Kim S,Zerillo J,et al. Preoperative QTc interval is not associated with intraoperative cardiac events or mortality in liver transplantation patients[J]. J Cardiothorac Vasc Anesth,2019,33(4):961-966. doi: 10.1053/j.jvca.2018.06.002 [6] Wu K C,Zhang L,Haberlen S A,et al. Predictors of electrocardiographic QT interval prolongation in men with HIV[J]. Heart,2019,105(7):559-565. doi: 10.1136/heartjnl-2018-313667 [7] 中华医学会心血管病学分会. 心血管疾病防治指南和共识[M]. 北京: 人民卫生出版社,2010: 79-86. [8] TIMI Study Group. The thrombolysis in myocardial infarction (TIMI) trial. Phase I findings[J]. N Engl J Med,1985,312(14):932-936. [9] Palmerini T,Calabrò P,Piscione F,et al. Impact of gene polymorphisms,platelet reactivity,and the SYNTAX score on 1-year clinical outcomes in patients with non-ST-segment elevation acute coronary syndrome undergoing percutaneous coronary intervention: The GEPRESS study[J]. JACC Cardiovasc Interv,2014,7(10):1117-1127. doi: 10.1016/j.jcin.2014.04.020 [10] Peng Y B,Wei X Q,Wu F,et al. Electroacupuncture for slow flow/no-reflow phenomenon in patients with acute myocardial infarction undergoing percutaneous coronary intervention: Protocol for a pilot randomized controlled trial[J]. Front Cardiovasc Med,2024,11(18):1401269-1401279. [11] Wu G Y,Wu Z F,Xu B D,et al. Slow-reflow and prognosis in patients with high parathyroid hormone levels undergoing primary percutaneous coronary intervention for acute ST-segment elevation myocardial infarction[J]. J Cardiovasc Transl Res,2024,17(3):657-668. doi: 10.1007/s12265-023-10457-8 [12] Ou Y H,Thant A T,Lee C H. Sudden deterioration of CPAP adherence after myocardial infarction in a Chinese patient: Potential effect of ACEI-induced airway hyperresponsiveness[J]. J Clin Sleep Med,2022,18(5):1463-1465. doi: 10.5664/jcsm.9880 [13] Nóbrega O T,Campos-Staffico A M,Oliveira E K,et al. Defective allele of the neuronal nitric oxide synthase gene increases insulin resistance during acute phase of myocardial infarction[J]. Int J Gen Med,2021,14(20):3669-3676. [14] 申文彬,白静,杨霞,等. 血小板高反应性对冠状动脉钙化患者介入术后发生主要不良心血管事件的研究[J]. 中华老年心脑血管病杂志,2016,18(2):153-157. doi: 10.3969/j.issn.1009-0126.2016.02.012 [15] Mol J Q,van Tuijl J,Bekkering S,et al. Peripheral blood mononuclear cell hyperresponsiveness in patients with premature myocardial infarction without traditional risk factors[J]. iScience,2023,26(7):107183-107193. doi: 10.1016/j.isci.2023.107183 [16] Yi Z C,Ke J Y,Wang Y G,et al. Fluvastatin protects myocardial cells in mice with acute myocardial infarction through inhibiting RhoA/ROCK pathway[J]. Exp Ther Med,2020,19(3):2095-2102. [17] Shi J L,Xiao P L,Liu X L,et al. Notch3 modulates cardiac fibroblast proliferation,apoptosis,and fibroblast to myofibroblast transition via negative regulation of the RhoA/ROCK/Hif1α axis[J]. Front Physiol,2020,11(30):669-679. [18] Min F,Jia X J,Gao Q,et al. Remote ischemic post-conditioning protects against myocardial ischemia/reperfusion injury by inhibiting the Rho-kinase signaling pathway[J]. Exp Ther Med,2020,19(1):99-106. [19] Wang W J,Peng X,Zhao L,et al. Extracellular vesicles from bone marrow mesenchymal stem cells inhibit apoptosis and autophagy of ischemia-hypoxia cardiomyocyte line in vitro by carrying miR-144-3p to inhibit ROCK1[J]. Curr Stem Cell Res Ther,2023,18(2):247-259. doi: 10.2174/1574888X17666220503192941 [20] Balamurugesan K,Karthik S,Fredrick J. Comparison of heart rate variability,QTc,and JT interval between diabetic patients and healthy controls: Role of gender and phases of menstrual cycle[J]. Cureus,2022,14(4):e24179-e24189. [21] Orchard J J,Orchard J W,Raju H,et al. Analysis of athlete QT intervals by age: Fridericia and Hodges heart rate corrections outperform Bazett for athlete ECG screening[J]. J Electrocardiol,2022,74(1):59-64. [22] Andršová I,Hnatkova K,Šišáková M,et al. Influence of heart rate correction formulas on QTc interval stability[J]. Sci Rep,2021,11(1):14269-14279. [23] Kleiman R B,Darpo B,Thorn M,et al. Potential strategy for assessing QT/QTc interval for drugs that produce rapid changes in heart rate: Electrocardiographic assessment of the effects of intravenous remimazolam on cardiac repolarization[J]. Br J Clin Pharmacol,2020,86(8):1600-1609. [24] 时长琴,龚艳艳,潘令新. De Winter心电图改变对急性前壁心肌梗死患者病情进展的影响[J]. 中国循证心血管医学杂志,2021,13(6):738-741. doi: 10.3969/j.issn.1674-4055.2021.06.24 [25] 邓启垣,郭志强,李浩平. 血小板高反应性、Lp-PLA2及GRACE评分联合评估AMI患者急诊PCI治疗预后的价值[J]. 岭南心血管病杂志,2020,26(5):503-506. doi: 10.3969/j.issn.1007-9688.2020.05.02 [26] 王国强,张丽美,李娜,等. ROCK1和ROCK2与心血管疾病的研究进展[J]. 华南国防医学杂志,2021,35(1):72-75. [27] 赵汉如,侯丽芳,周单,等. 心电图联合血清氨基末端脑钠肽前体对急性心肌梗死患者择期经皮冠状动脉介入治疗后近期发生主要不良心血管事件的预测价值研究[J]. 实用心脑肺血管病杂志,2021,29(4):32-37. doi: 10.12114/j.issn.1008-5971.2021.00.077 -





 下载:
下载: