Correlation between Glycolytic Pathway of Monocytes and Intracranial Pressure and Clinical Prognosis in Patients with Hypertensive Cerebral Hemorrhage
-
摘要:
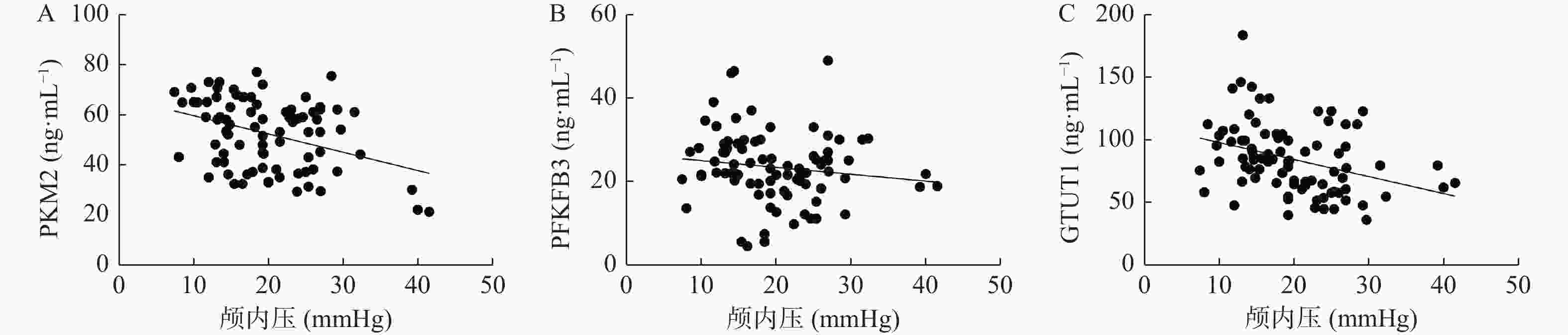
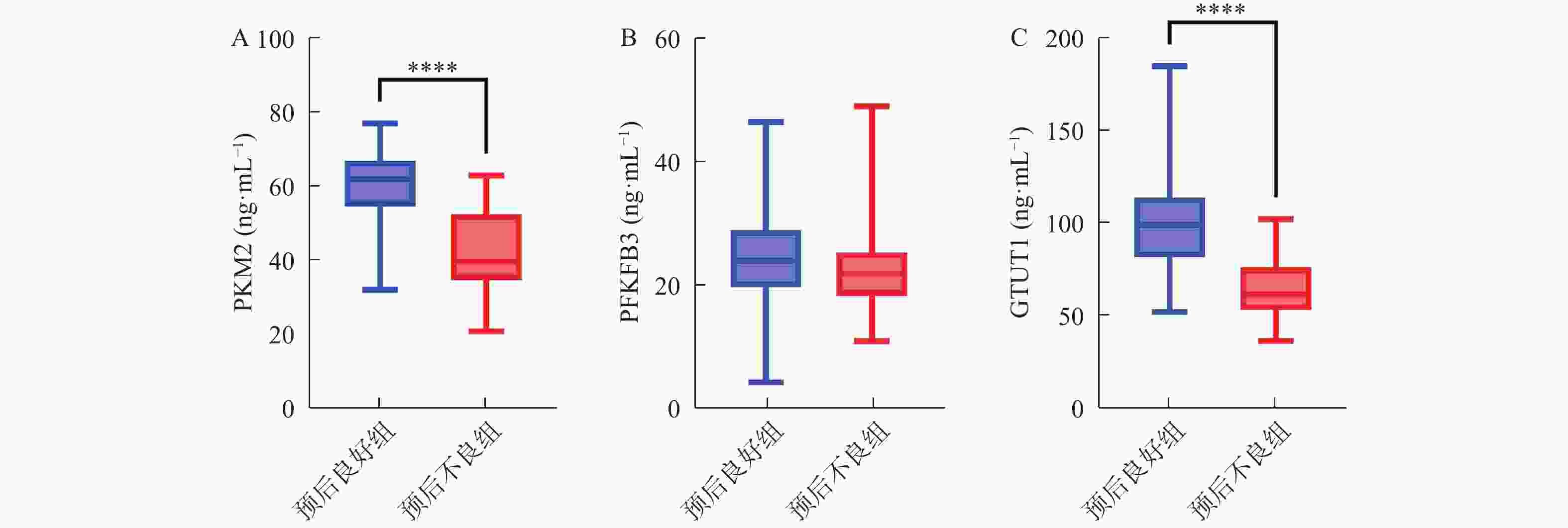
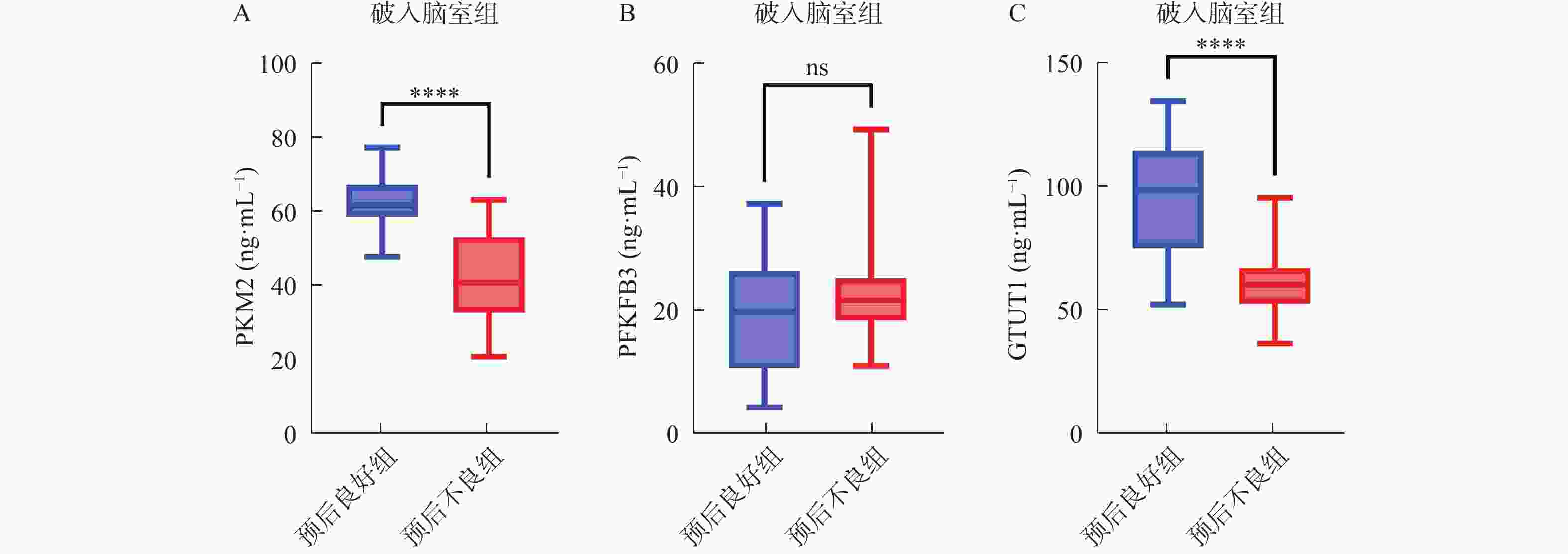
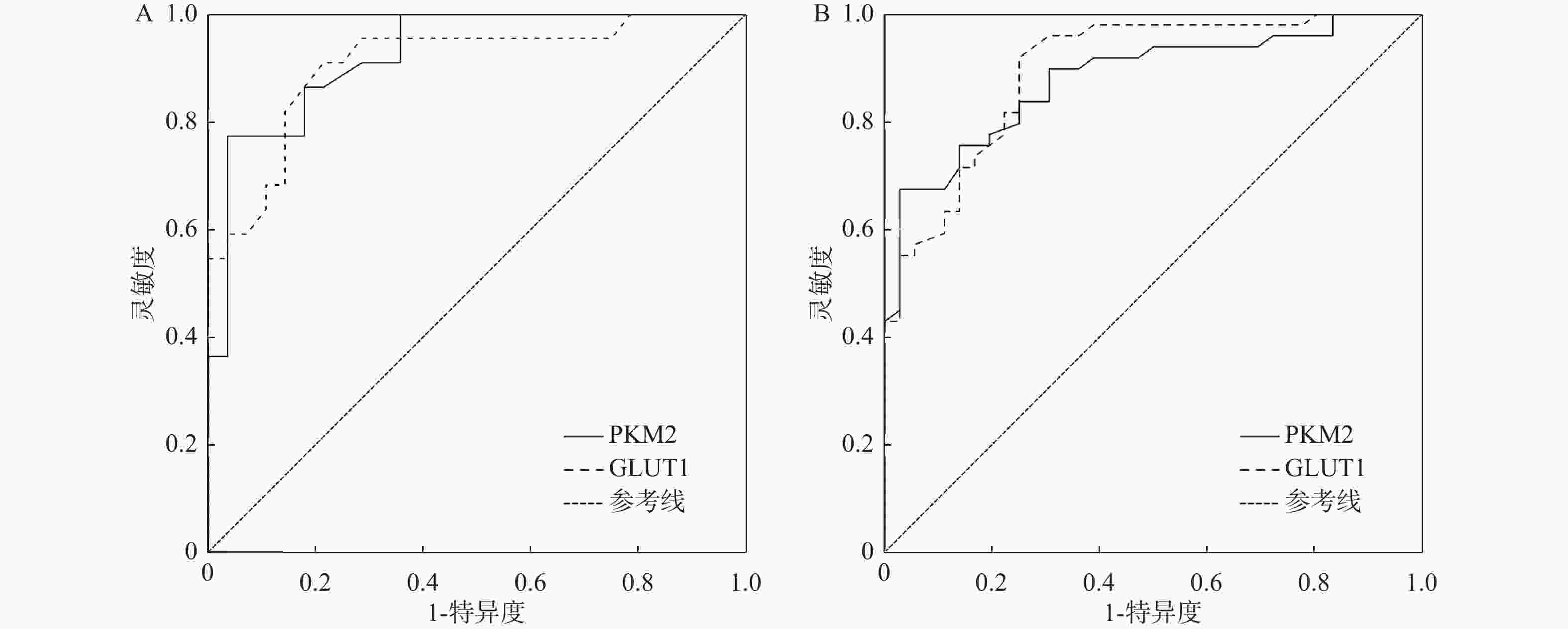
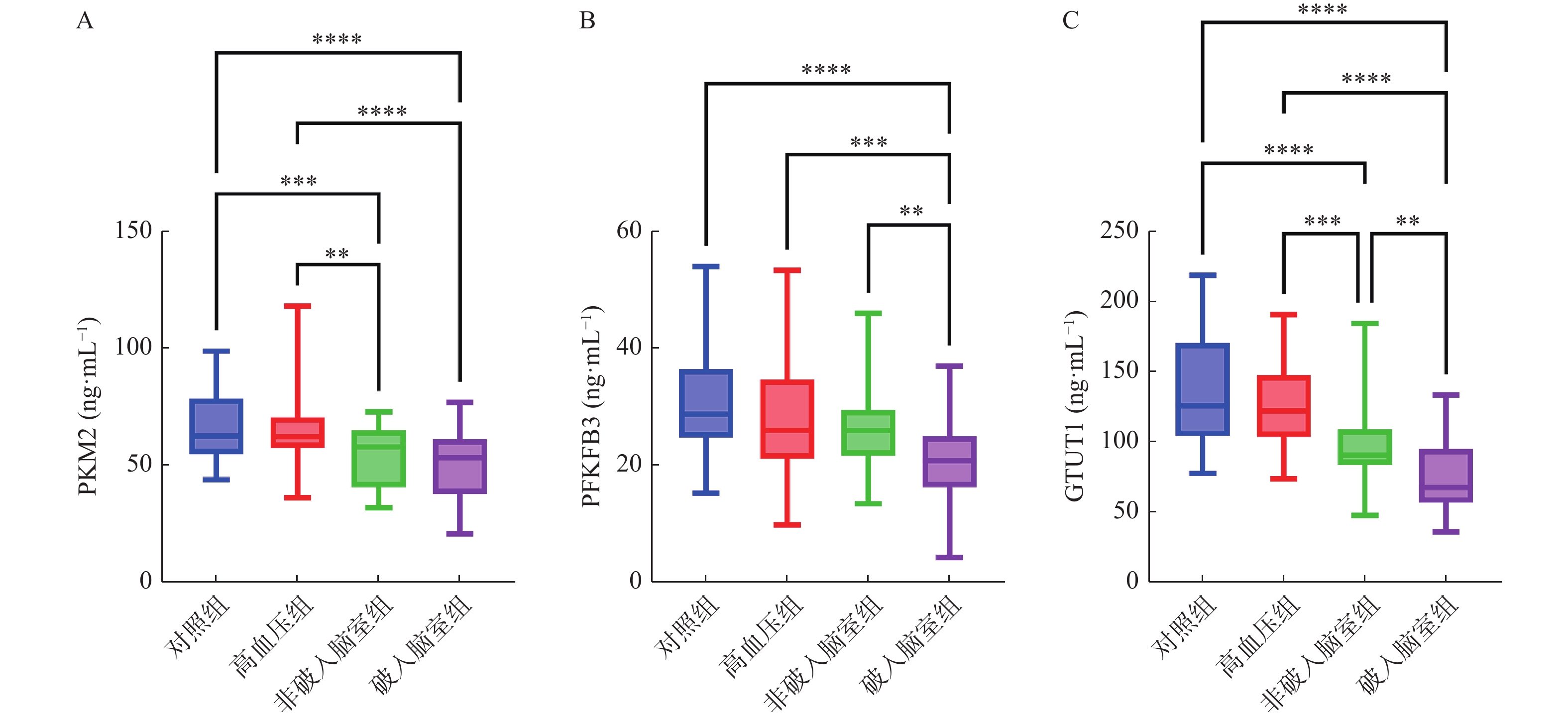
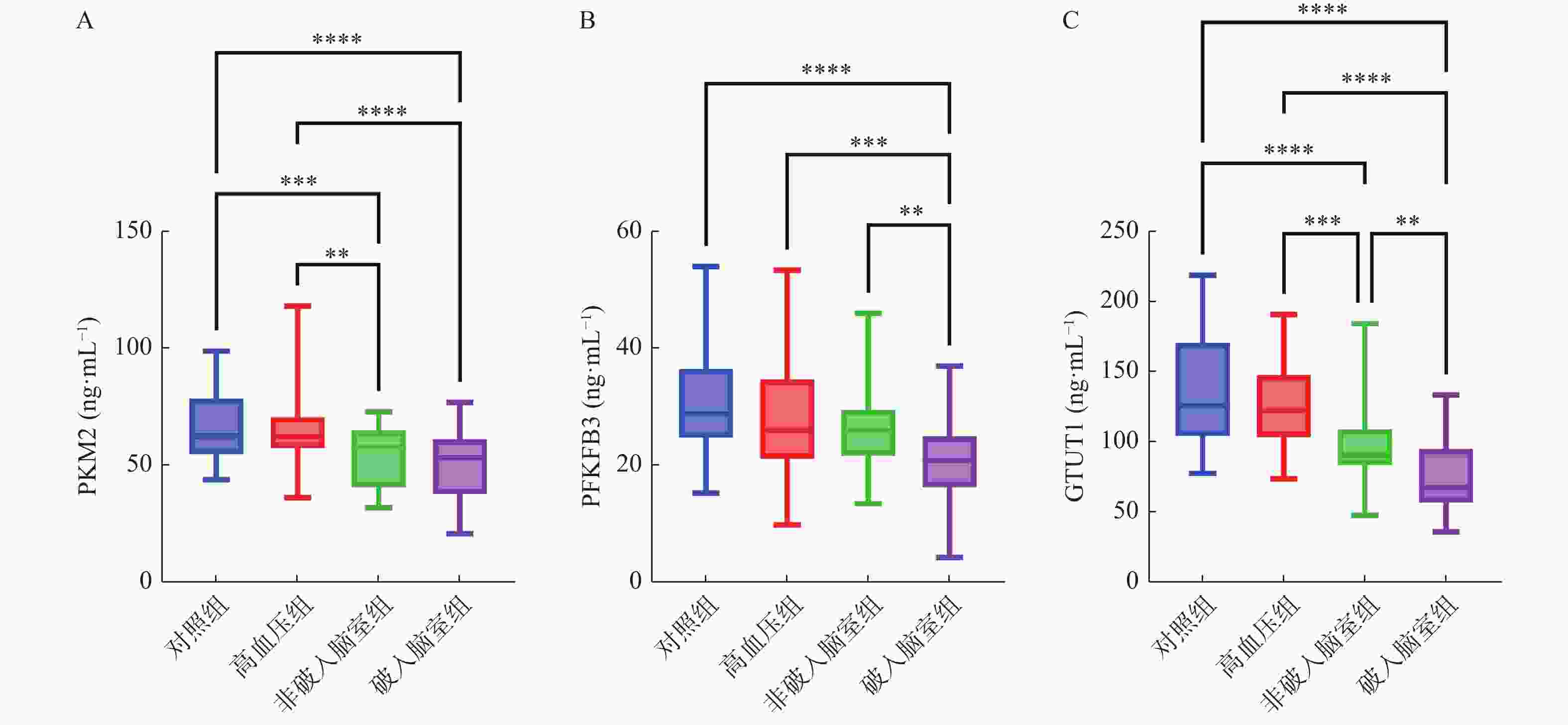
目的 探讨外周血单核细胞(peripheral blood mononuclear cells,PBMCs)糖酵解相关指标[葡萄糖转运蛋白1(glucose transporter 1,GLUT1),果糖-2,6-二磷酸酶3(fructose-2,6-bisphosphatase 3,PFKFB3),乳酸激酶M2(Pyruvate kinase M2,PKM2)]与高血压脑出血(hypertensive intracerebral hemorrhage,HICH)患者颅内压及临床预后的相关性。 方法 回顾性收集2021年1月至2022年6月在邢台市中心医院住院的85例HICH患者作为研究对象。通过酶联免疫吸附测定试剂盒分析PBMCs中PKM2,GLUT1,PFKFB3水平。在HICH发作后6个月,使用改良Rankin量表(modified Rankin scale,mRS)评分来评估短期结局,将患者分为预后良好(mRS评分≤2)和预后不良(mRS得分≥3)。 结果 破入脑室组HICH患者PBMCs中PKM2,PFKFB3和GLUT1水平较非破入脑室组患者进一步降低(P < 0.05)。出院6个月后,非破入脑室组HICH患者中8例(22.9%)患者预后不良,破入脑室组HICH患者中28例(56.0%)患者预后不良,差异具有统计学意义(χ2 = 9.263,P = 0.002)。与预后良好组相比,预后不良组HICH患者PBMCs中PKM2,GLUT1水平降低(P < 0.05)。在破入脑室组HICH患者中,与预后良好组相比,预后不良组HICH患者PBMCs中PKM2,GLUT1水平降低(P < 0.05)。在破入脑室组HICH患者中,PKM2,GLUT1预测HICH患者不良预后的AUC分别为0.879(95%CI 0.807~0.951),0.897(95%CI 0.831~0.963)。 结论 HICH破入脑室患者PBMCs中PKM2,GLUT1水平明显降低,二者表达与患者颅内压呈负相关性,并可用于预测患者的短期预后。 Abstract:Objective To explore the correlation between glycolysis related indexes of peripheral blood mononuclear cells (PBMCs) [glucose transporter 1(GLUT1), fructose-2, 6-diphosphatase 3(PFKFB3) and lactate kinase M2(PKM2)] and intracranial pressure and clinical prognosis of patients with hypertensive cerebral hemorrhage (HICH) who broke into the ventricle. Methods 85 HICH patients hospitalized in our hospital from January 2021 to June 2022 were retrospectively collected as the research participants. The levels of PKM2, GLUT1 and PFKFB3 in PBMCs were analyzed by enzyme-linked immunosorbent assay kit. Six months after the onset of HICH, the short-term outcome was evaluated by modified Rankin scale (mRS), and the patients were divided into good prognosis (mRS score ≤2) and poor prognosis (mRS score ≥3). Results The levels of PKM2, PFKFB3 and GLUT1 in PBMCs of HICH patients with ventricular rupture were further lower than those of the patients without ventricular rupture (P < 0.05). Six months after discharge, 8 patients (22.9%) with HICH in non-ventricular rupture group had poor prognosis, while 28 patients (56.0%) with HICH in ventricular rupture group had poor prognosis, and the difference was statistically significant (χ2=9.263, P = 0.002). Compared with the group with good prognosis, the levels of PKM2 and GLUT1 in PBMCs of HICH patients with poor prognosis were lower (P < 0.05). Compared with the good prognosis group, the levels of PKM2 and GLUT1 in PBMCs of HICH patients with poor prognosis group were lower in HICH patients with ventricular rupture (P < 0.05). In HICH patients who broke into the ventricle, the AUC of PKM2 and GLUT1 in predicting the poor prognosis of HICH patients were 0.879 (95%CI: 0.807~0.951) and 0.897 (95%CI: 0.831~0.963), respectively. Conclusion The levels of PKM2 and GLUT1 in PBMCs of patients with HICH breaking into ventricles decrease significantly, and are negatively correlated with intracranial pressure, which can be used to predict the short-term prognosis of the patients. -
表 1 非破入脑室组和破入脑室组患者特征[($\bar x \pm s $)/n(%)]
Table 1. Characteristics of patients in non-ruptured ventricle group and ruptured ventricle group [($\bar x \pm s $)/n(%)]
特征 对照组(n=50) 高血压组(n=50) 非破入脑室组(n=35) 破入脑室组(n=50) F/t/χ2 P 男性 18(36.0) 25(50.0) 12(34.3) 18(36.0) 3.219 0.359 BMI (kg/m2) 24.94 ± 3.31 23.44 ± 3.66 24.40 ± 3.94 25.45 ± 4.08 1.915 0.129 年龄(岁) 51.86 ± 6.34 52.10 ± 7.94 53.09 ± 14.91 51.20 ± 10.56 0.249 0.862 ICU住院时间(d) 23.37 ± 18.45 33.64 ± 23.83 2.139 0.035b 机械通气时间(d) 16.23 ± 15.51 22.96 ± 17.38 1.829 0.071 糖尿病 1(2.9) 1(2.0) − 0.638a 心血管疾病 5(14.3) 3(6.0) 1.658 0.198 吸烟 14(40.0) 18(36.0) 0.130 0.883 饮酒 3(8.6) 4(8.0) 0.009 0.825 收缩压(mmHg) 118.77 ± 14.86 143.23 ± 17.81* 147.26 ± 21.48* 147.67 ± 20.69* 26.300 <0.001b 舒张压(mmHg) 75.09 ± 9.31 88.11 ± 10.18* 95.90 ± 12.38* 92.60 ± 11.64* 32.692 <0.001b 颅内压(mmHg) 16.60 ± 5.42 23.11 ± 7.27 4.681 <0.001b GCS评分 7.51 ± 2.52 6.21 ± 2.54 2.362 0.020b 诊断和治疗的时间间隔 2.022 0.155 <12 h 20(57.1) 36(72.0) ≥12 h~24 h 15(42.9) 14(28.0) 实验数据 总胆固醇(mmol/L) 4.25 ± 0.89 4.22 ± 1.02 0.170 0.866 甘油三酯(mmol/L) 1.16 ± 0.60 1.08 ± 0.42 0.723 0.471 LDL-C(mmol/L) 2.59 ± 0.71 2.38 ± 0.77 1.250 0.215 HDL-C(mmol/L) 1.07 ± 0.41 1.23 ± 0.41 1.766 0.081 a为Fisher精确检验;b为差异有统计学意义;与对照组相比,*P < 0.05。 表 2 多变量回归分析HICH患者不良预后的影响因素
Table 2. Multivariate regression analysis of influencing factors of poor prognosis in HICH patients
指标 B S.E. Wald P OR 95%CI 下限 上限 PKM2 −0.153 0.043 12.447 <0.001* 0.858 0.789 0.934 PFKFB3 0.102 0.057 3.139 0.076 1.107 0.989 1.238 GLUT1 −0.112 0.030 13.537 <0.001* 0.894 0.843 0.949 常量 13.846 3.356 17.024 <0.001* 1030862.018 *P < 0.05。 -
[1] Seiffge D J,Fandler-Höfler S,Du Y,et al. Intracerebral haemorrhage-mechanisms,diagnosis and prospects for treatment and prevention[J]. Nat Rev Neurol,2024,20(12):708-723. doi: 10.1038/s41582-024-01035-w [2] Minhas J S,Moullaali T J,Rinkel G J E,et al. Blood pressure management after intracerebral and subarachnoid hemorrhage: The knowns and known unknowns[J]. Stroke,2022,53(4):1065-1073. doi: 10.1161/STROKEAHA.121.036139 [3] Lee B C,Tsai H H,Chen Z W,et al. Aldosteronism is associated with more severe cerebral small vessel disease in hypertensive intracerebral hemorrhage[J]. Hypertens Res,2024,47(3):608-617. doi: 10.1038/s41440-023-01458-w [4] Chen X,Zhou Y,Wang S,et al. Mechanism of baicalein in brain injury after intracerebral hemorrhage by inhibiting the ROS/NLRP3 inflammasome pathway[J]. Inflammation,2022,45(2):590-602. doi: 10.1007/s10753-021-01569-x [5] Xiao L,Wang M,Shi Y,et al. Secondary white matter injury mediated by neuroinflammation after intracerebral hemorrhage and promising therapeutic strategies of targeting the NLRP3 inflammasome[J]. Curr Neuropharmacol,2023,21(3):669-686. doi: 10.2174/1570159X20666220830115018 [6] Zhang R,Zhang Y,Liu Z,et al. Association between neutrophil-to-albumin ratio and long-term mortality of aneurysmal subarachnoid hemorrhage[J]. BMC Neurol,2023,23(1):374-384. doi: 10.1186/s12883-023-03433-x [7] Revilla-González G,Varela L M,Ruiz de Azua-López Z,et al. Changes in adhesion and the expression of adhesion molecules in PBMCs after aneurysmal subarachnoid hemorrhage: Relation to cerebral vasospasm[J]. Transl Stroke Res,2024,15(2):378-387. doi: 10.1007/s12975-023-01136-6 [8] Ya X,Ma L,Liu C,et al. Metabolic alterations of peripheral blood immune cells and heterogeneity of neutrophil in intracranial aneurysms patients[J]. Clin Transl Med,2024,14(2):e1572-e1606. [9] Zink F,Vogt J,Wachter U,et al. Effects of acute subdural hematoma-induced brain injury on energy metabolism in peripheral blood mononuclear cells[J]. Shock,2021,55(3):407-417. doi: 10.1097/SHK.0000000000001642 [10] Schellinger P D,Bryan R N,Caplan L R,et al. Evidence-based guideline: The role of diffusion and perfusion MRI for the diagnosis of acute ischemic stroke: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology[J]. Neurology,2010,75(2):177-185. doi: 10.1212/WNL.0b013e3181e7c9dd [11] 周永芳,伍国锋,董文涛,等. 急性脑出血患者低血钾发生情况及其与短期预后的关系[J]. 重庆医学,2023,52(7):961-966. doi: 10.3969/j.issn.1671-8348.2023.07.001 [12] Wang C,Bai J,He Q,et al. Therapy management and outcome of acute hydrocephalus secondary to intraventricular hemorrhage in adults[J]. Chin Neurosurg J,2024,10(1):17-26. doi: 10.1186/s41016-024-00369-0 [13] 郑海军,戴凯茜,娄晓辉,等. 缺氧诱导因子-1α/血管内皮生长因子通路表达与高血压脑出血破入脑室患者颅内压及预后的相关性[J]. 中华高血压杂志,2022,30(3):283-286. [14] Maida C D,Norrito R L,Rizzica S,et al. Molecular pathogenesis of ischemic and hemorrhagic strokes: background and therapeutic approaches[J]. Int J Mol Sci,2024,25(12):6297-6331. doi: 10.3390/ijms25126297 [15] Johnson C W,Askenase M H,Beatty H E,et al. Single cell rna-sequencing reveals array of immune activation states in intracerebral hemorrhage[J]. Stroke,2022,53(Suppl_1):A99-A99. [16] Ya X L,Ma L,Liu C L,et al. Metabolic alterations of peripheral blood immune cells and heterogeneity of neutrophil in intracranial aneurysms patients[J]. Clin Transl Med,2024,14(2):e1572-e1606. doi: 10.1002/ctm2.1572 [17] Xiong X Y,Liang Y J,Zhang X X,et al. PKM2 Nuclear Translocation Promotes Glial Cell Activation and Aggravates the Brain Injury of Intracerebral Hemorrhage[J]. J Integr Neurosci,2023,22(6):168-179. doi: 10.31083/j.jin2206168 [18] Zhang X,Peng L,Kuang S,et al. Lactate accumulation from HIF-1α-mediated PMN-MDSC glycolysis restricts brain injury after acute hypoxia in neonates[J]. J Neuroinflammation,2025,22(1):59-84. doi: 10.1186/s12974-025-03385-8 [19] Walsh K B,Zhang X,Zhu X,et al. Intracerebral hemorrhage induces monocyte-related gene expression within six hours: Global transcriptional profiling in swine ICH[J]. Metab Brain Dis,2019,34(3):763-774. doi: 10.1007/s11011-019-00399-z [20] Goods B A,Askenase M H,Markarian E,et al. Leukocyte dynamics after intracerebral hemorrhage in a living patient reveal rapid adaptations to tissue milieu[J]. JCI insight,2021,6(6):e145857-e145868. doi: 10.1172/jci.insight.145857 [21] Giralt-Steinhauer E,Jiménez-Balado J,Fernández-Pérez I,et al. Genetics and epigenetics of spontaneous intracerebral hemorrhage[J]. Int J Mol Sci,2022,23(12):6479-6490. doi: 10.3390/ijms23126479 [22] Ya X,Liu C,Ma L,et al. Single‐cell atlas of peripheral blood by CyTOF revealed peripheral blood immune cells metabolic alterations and neutrophil changes in intracranial aneurysm rupture[J]. MedComm,2024,5(8):e637-e655. doi: 10.1002/mco2.637 [23] Xie W,Fang J,Shan Z,et al. Regulation of autoimmune disease progression by Pik3ip1 through metabolic reprogramming in T cells and therapeutic implications[J]. Sci Adv,2022,8(39):eabo4250-eabo4266. doi: 10.1126/sciadv.abo4250 -





 下载:
下载: