Efficacy Analysis of BMD,T-scores,HU Values,and Modified VBQ Scores in Predicting Thoracolumbar Fragility Fractures
-
摘要:
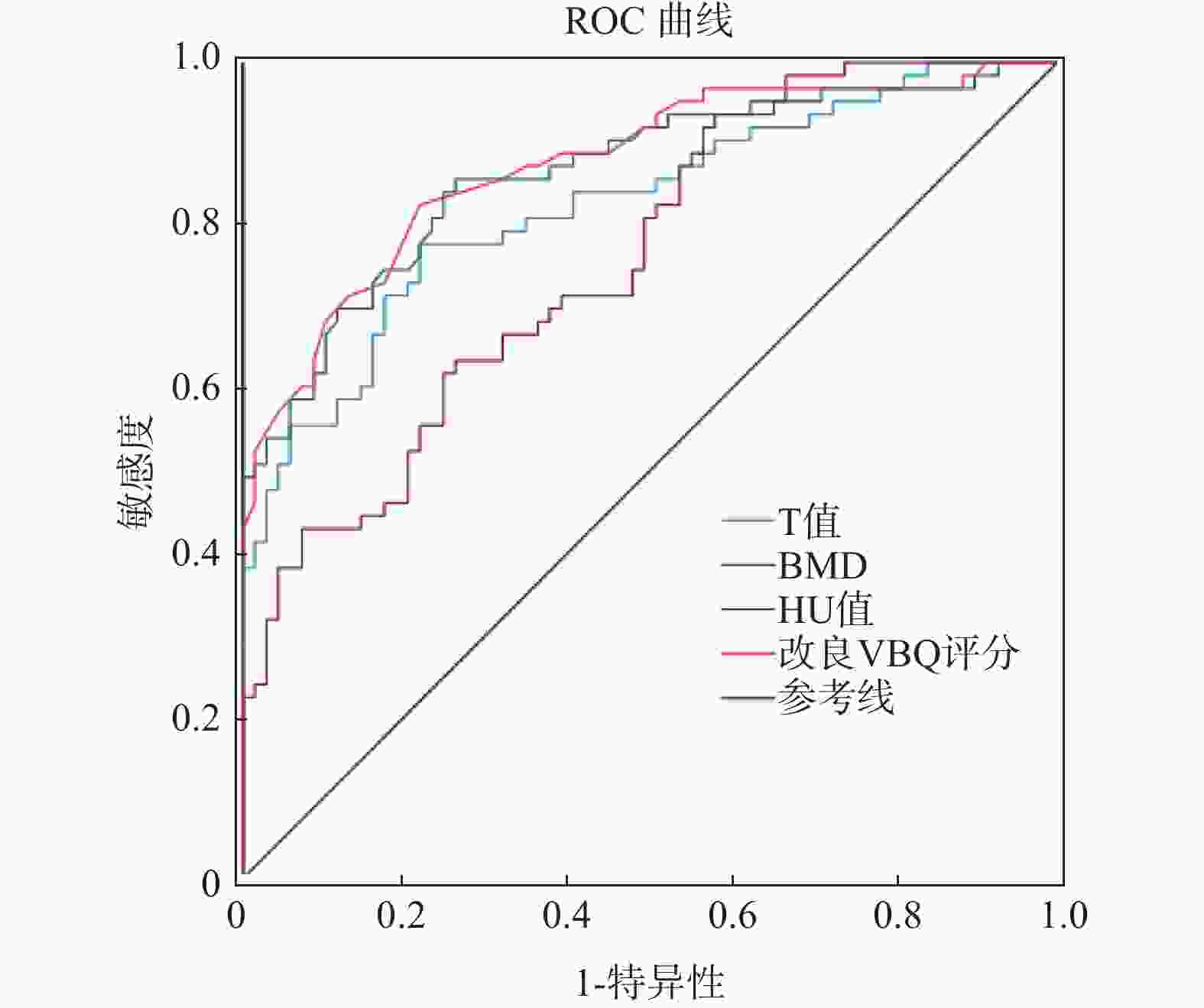
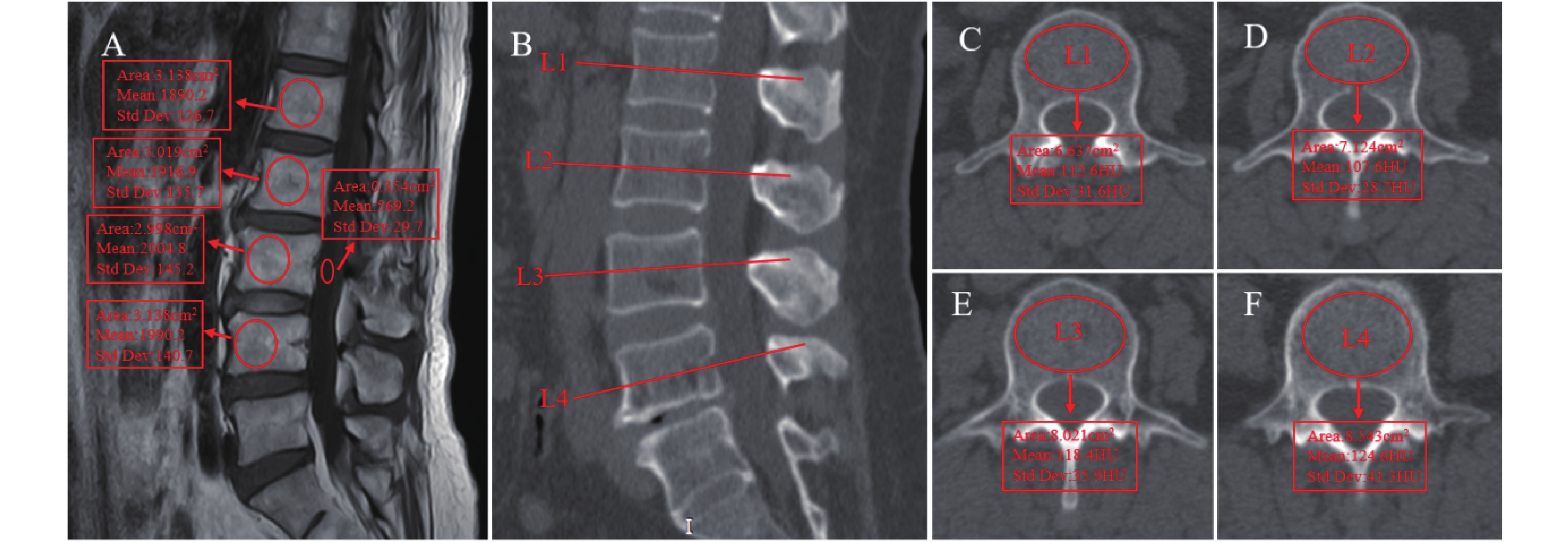
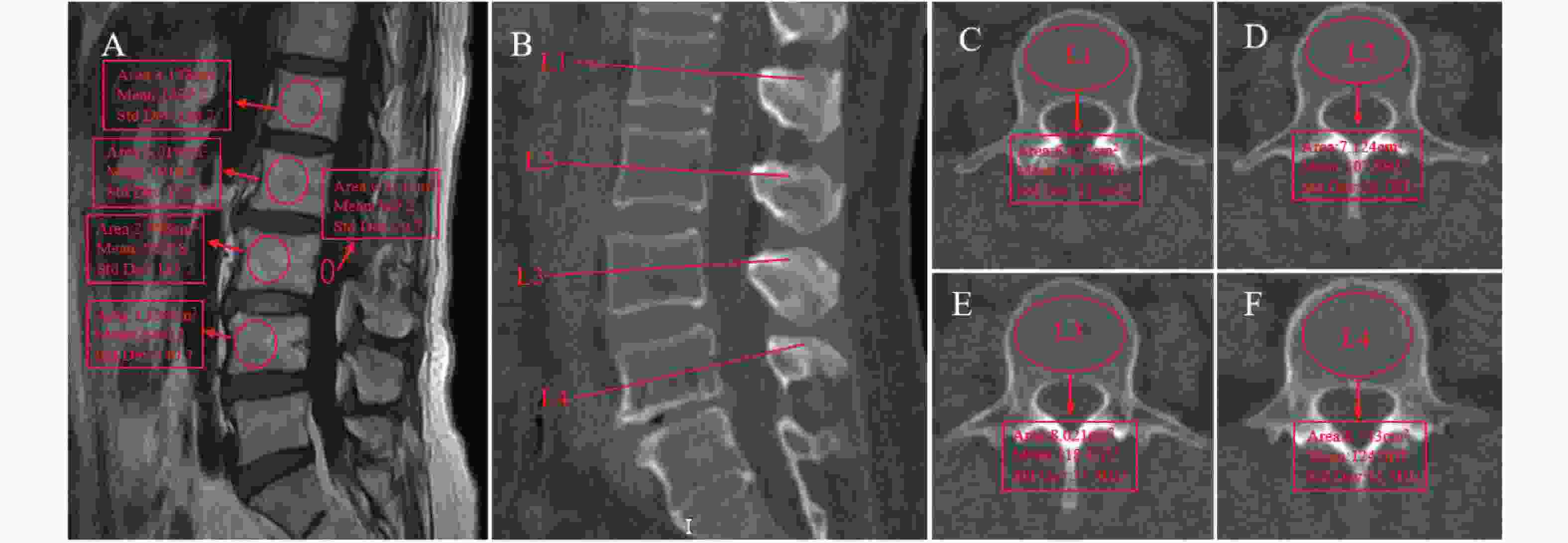
目的 研究胸腰椎骨折患者DEXA(dual-energy X-ray absorptiometry,DEXA)所测BMD(bone mineral density,BMD)、T值(T-score)、腰椎HU值(hounsfield unit,HU)和改良VBQ (vertebral body quality,VBQ)评分的差异,并分析四者间的相关性以及BMD 、T值、腰椎HU值和改良VBQ评分在预测胸腰椎骨折的效能特点。 方法 收集2022年1月至2025年3月在昆明医科大学第二附属医院骨科行住院治疗的胸腰椎脆性骨折患者。将符合纳入标准的132例患者分为骨折组(n = 63)与非骨折组(n = 69),并分别在DEXA上记录L1~L4椎体BMD、T值,腰椎CT测量HU值,腰椎MRI(magnetic resonance imaging,MRI)测量计算VBQ评分。组间比较采用独立样本t检验,BMD、T值、HU值、改良VBQ评分四者之间的相关性采用Pearson's相关性检验,并用受试者工作曲线(receiver-operator curve,ROC)分析其预测胸腰椎骨折的效能。 结果 骨折组患者中L1~L4的平均BMD、T值、HU值均低于非骨折组,而改良VBQ评分高于非骨折组,两组之间均存在显著差异(P < 0.001 )。相关性分析中,L1~L4的BMD、T值与L1~L4 HU值呈显著正相关(P < 0.001),L1~L4的BMD、T值、L1~L4HU值三者与改良VBQ评分之间呈显著负相关(P < 0.001)。L1~L4平均T值、BMD 、HU值和改良VBQ评分预测胸腰椎骨折的AUC值分别为0.826、0.836、0.759、0.875,其分别对应最佳阈值为T值(-1.65)、BMD(0.836)、HU值(68.4)、改良VBQ评分(3.01)。 结论 L1~L4椎体BMD、T值、HU值和改良VBQ评分四者之间相关性显著,都可以作为预测胸腰椎骨折效能的指标,其中改良VBQ评分预测表现最好,是良好的椎体骨质量评估辅助手段。 Abstract:Objective To investigate the differences in BMD, T-scores, lumbar HU values, and modified VBQ scores in patients with thoracolumbar fractures, analyze their correlations, and evaluate their predictive efficacy for thoracolumbar fractures. Methods Patients with thoracolumbar fragility fractures and hospitalized in the Department of Orthopedics at the Second Affiliated Hospital of Kunming Medical University from January 2022 to March 2025 were retrospectively enrolled. Among them, 132 eligible patients were divided into the fracture group (n = 63) and the non-fracture group (n = 69). BMD and T-scores of L1~L4 vertebrae were measured via DEXA, lumbar HU values were obtained from CT scans, and modified VBQ scores were calculated using lumbar MRI. Intergroup comparisons were performed using independent samples t-tests. Pearson's correlation analysis was used to assess the relationships among BMD, T-scores, HU values, and modified VBQ scores. Receiver operating characteristic (ROC) curve analysis was conducted to evaluate their predictive performance for thoracolumbar fractures. Results The fracture group exhibited significantly lower mean BMD, T-scores, and HU values in L1~L4 compared to the non-fracture group, while modified VBQ scores were significantly higher (P < 0.001). Correlation analysis revealed a significant positive correlation between BMD, T-scores, and HU values in L1~L4, whereas all three parameters showed a significant negative correlation with modified VBQ scores (P < 0.001). The AUC values for predicting thoracolumbar fractures were 0.826 (T-score), 0.836 (BMD), 0.759 (HU value), and 0.875 (modified VBQ score), with optimal cutoff thresholds of -1.65 (T-score), 0.836 g/cm2 (BMD), 68.4 (HU value), and 3.01 (modified VBQ score), respectively. Conclusion BMD, T-scores, HU values, and modified VBQ scores in L1~L4 vertebrae are significantly correlated and can serve as the predictive indicators for thoracolumbar fractures. Among them, the modified VBQ score demonstrates the best predictive performance, making it a valuable auxiliary tool for assessing the vertebral bone quality. -
Key words:
- Fragility fracture /
- Bone density /
- Hounsfield unit /
- Vertebral body quality score
-
表 1 骨折组与非骨折组患者的一般资料比较($\bar x \pm s $)
Table 1. Comparison of general information of patients in the fracture group and non-fracture group ($\bar x \pm s $)
骨折组
(n=63)非骨折组
(n=69)t P 男性 17/63 25/69 女性 46/63 44/69 年龄(岁) 71.03 ± 8.49 69.41 ± 5.16 1.315 0.192 BMI(g/cm2) 23.31 ± 3.31 24.30 ± 3.24 −1.733 0.086 L1~L4 BMD 0.79 ± 0.15 1.01 ± 0.15 −8.485 <0.01* L1~L4 T值 −2.61 ± 1.20 −0.70 ± 1.24 −8.996 <0.01* L1~L4 HU值 64.63 ± 21.26 91.27 ± 29.67 −5.965 <0.01* 改良VBQ评分 3.39 ± 0.60 2.72 ± 0.39 7.604 <0.01* *P < 0.05。 表 2 L1~L4平均BMD 、T值、 HU值和改良VBQ评分相关性
Table 2. Correlation between mean BMD,T-scores,HU,and modified VBQ scores at L1–L4
指标 BMD T HU 改良VBQ评分 BMD 1 T值 0.988** 1 HU值 0.854** 0.858** 1 改良VBQ评分 −0.684** −0.702** −0.661** 1 **在 0.001 级别(双尾),相关性显著。 表 3 L1~L4平均T值、BMD 、HU值和改良VBQ评分预测胸腰椎骨折的效能
Table 3. Predictive efficacy of mean T-scores,BMD,HU,and modified VBQ scores at L1–L4 for thoracolumbar fractures
指标 AUC 95%CI 敏感度(%) 特异度(%) 约登指数 最佳阈值 T值 0.826 0.756~0.897 77.8 78.3 0.608 −1.65 BMD 0.836 0.803~0.928 82.5 73.9 0.596 0.91 HU值 0.759 0.680~0.839 63.5 73.9 0.374 68.40 改良VBQ评分 0.875 0.815~0.935 85.7 78.3 0.560 3.01 -
[1] Wright N C, Saag K G, Dawson-Hughes B, et al. The impact of the new National Bone Health Alliance (NBHA) diagnostic criteria on the prevalence of osteoporosis in the USA[J]. Osteoporosis Int, 2017, 28(4): 1225-1232. doi: 10.1007/s00198-016-3865-3 [2] Salari N, Darvishi N, Bartina Y, et al. Global prevalence of osteoporosis among the world older adults: A comprehensive systematic review and meta-analysis[J]. J Orthop Surg Res, 2021, 16(1): 669. doi: 10.1186/s13018-021-02821-8 [3] Zou D, Ye K, Tian Y, et al. Characteristics of vertebral CT Hounsfield units in elderly patients with acute vertebral fragility fractures[J]. European Spine Journal, 2020, 29(5): 1092-1097. doi: 10.1007/s00586-020-06363-1 [4] Johannesdottir F, Allaire B, Bouxsein M L. Fracture prediction by computed tomography and finite element analysis: Current and future perspectives[J]. Curr Osteoporos Rep, 2018, 16(4): 411-422. doi: 10.1007/s11914-018-0450-z [5] Yu F, Xia W. The epidemiology of osteoporosis, associated fragility fractures, and management gap in China[J]. Arch Osteoporos, 2019, 14(1): 32. doi: 10.1007/s11657-018-0549-y [6] Celi M, Rao C, Scialdoni A, et al. Bone mineral density evaluation in osteoporosis: Why yes and why not [J]? Aging Clin Exp Res, 2013, 25 Suppl 1 S47-9. [7] Wagner S, Kang D, Steelman T, et al. Diagnosing the undiagnosed: Osteoporosis in patients undergoing lumbar fusion[J]. Spine J, 2016, 16(10): S301. [8] Alacreu E, Moratal D, Arana E. Opportunistic screening for osteoporosis by routine CT in Southern Europe[J]. Osteoporosis Int, 2017, 28(3): 983-990. doi: 10.1007/s00198-016-3804-3 [9] Pompe E, de Jong PA, de Jong WU, et al. Inter-observer and inter-examination variability of manual vertebral bone attenuation measurements on computed tomography[J]. Eur Radiol, 2016, 26(9): 3046-3053. doi: 10.1007/s00330-015-4145-x [10] Zou D, LI W, Deng C, et al. The use of CT Hounsfield unit values to identify the undiagnosed spinal osteoporosis in patients with lumbar degenerative diseases[J]. Eur Spine J, 2019, 28(8): 1758-1766. doi: 10.1007/s00586-018-5776-9 [11] LI Y L, Wong K H, Law M W, et al. Opportunistic screening for osteoporosis in abdominal computed tomography for Chinese population[J]. Arch Osteoporos, 2018, 13(1): 76. doi: 10.1007/s11657-018-0492-y [12] Ehresman J, Pennington Z, Schilling A, et al. Novel MRI-based score for assessment of bone density in operative spine patients[J]. Spine J, 2020, 20(4): 556-562. doi: 10.1016/j.spinee.2019.10.018 [13] Jones C, Okano I, Arzani A, et al. The predictive value of a novel site-specific MRI-based bone quality assessment, endplate bone quality (EBQ), for severe cage subsidence among patients undergoing standalone lateral lumbar interbody fusion[J]. Spine J, 2022, 22(11): 1875-1883. doi: 10.1016/j.spinee.2022.07.085 [14] Shah L M, Hanrahan C J. MRI of spinal bone marrow: Part I, techniques and normal age-related appearances[J]. Am J Roentgenol, 2011, 197(6): 1298-308. doi: 10.2214/AJR.11.7005 [15] Cheng X, Zhao K, Zha X, et al. Opportunistic screening using low-dose CT and the prevalence of osteoporosis in China: A nationwide, multicenter study[J]. J Bone Miner Res, 2021, 36(3): 427-35. [16] Siris E S, Adler R, Bilezikian J, et al. The clinical diagnosis of osteoporosis: A position statement from the National Bone Health Alliance Working Group[J]. Osteoporos Int, 2014, 25(5): 1439-43. doi: 10.1007/s00198-014-2655-z [17] Kim D K, Kim J Y, Kim D Y, et al. Risk factors of proximal junctional kyphosis after multilevel fusion surgery: More than 2 years follow-up data[J]. J Korean Neurosurg Soc, 2017, 60(2): 174-180. doi: 10.3340/jkns.2016.0707.014 [18] Pinter Z W, Monsef J B, Salmons H I, et al. Does preoperative bone mineral density impact fusion success in anterior cervical spine surgery? A prospective cohort study[J]. World Neurosurg, 2022, 16(4): 830-834. [19] Adams J E. Quantitative computed tomography[J]. European Journal of Radiology, 2009, 71(3): 415-24. doi: 10.1016/j.ejrad.2009.04.074 [20] Salzmann S N, Okano I, Jones C, et al. Preoperative MRI-based vertebral bone quality (VBQ) score assessment in patients undergoing lumbar spinal fusion[J]. Spine J, 2022, 22(8): 1301-1308. doi: 10.1016/j.spinee.2022.03.006 [21] Tafida M A, Wagatsuma Y, Ma E, et al. Descriptive epidemiology of traumatic spinal injury in Japan[J]. J Orthop Sci, 2018, 23(2): 273-276. doi: 10.1016/j.jos.2017.10.013 [22] Bloem J L, Reijnierse M, Huizinga T W J, et al. MR signal intensity: Staying on the bright side in MR image interpretation[J]. RMD Open, 2018, 4(1): e000728. doi: 10.1136/rmdopen-2018-000728 [23] Haffer H, Muellner M, Chiapparelli E, et al. Bone quality in patients with osteoporosis undergoing lumbar fusion surgery: Analysis of the MRI-based vertebral bone quality score and the bone microstructure derived from microcomputed tomography[J]. Spine J, 2022, 22(10): 1642-1650. doi: 10.1016/j.spinee.2022.05.008 [24] Ehresman J, Schilling A, Yang X, et al. Vertebral bone quality score predicts fragility fractures independently of bone mineral density[J]. Spine J, 2021, 21(1): 20-27. doi: 10.1016/j.spinee.2020.05.540 [25] LI Q, Hu B, Yang H, et al. MRI-based pedicle bone quality score: correlation to quantitative computed tomography bone mineral density and its role in quantitative assessment of osteoporosis[J]. Spine J, 2023, 24(10): 1825-1832. [26] Huang W, Gong Z, Wang H, et al. Use of MRI-based vertebral bone quality score (VBQ) of S1 body in bone mineral density assessment for patients with lumbar degenerative diseases[J]. Eur Spine J, 2023, 32(5): 1553-1560. doi: 10.1007/s00586-023-07643-2 [27] Yin H, Lin W, Xie F, et al. MRI-based Vertebral bone quality score for osteoporosis screening based on different osteoporotic diagnostic criteria using DXA and QCT[J]. Calcif Tissue Int, 2023, 113(4): 383-392. doi: 10.1007/s00223-023-01115-x [28] Özmen E, Biçer O, Meriç E, et al. Vertebral bone quality score for opportunistic osteoporosis screening: A correlation and optimal threshold analysis[J]. Eur Spine J, 2023, 32(11): 3906-3911. doi: 10.1007/s00586-023-07912-0 -





 下载:
下载: