Diagnostic Value of Magnetic Resonance Imaging in Immediate Injury of Temporomandibular Joint Without Condylar Fracture
-
摘要:
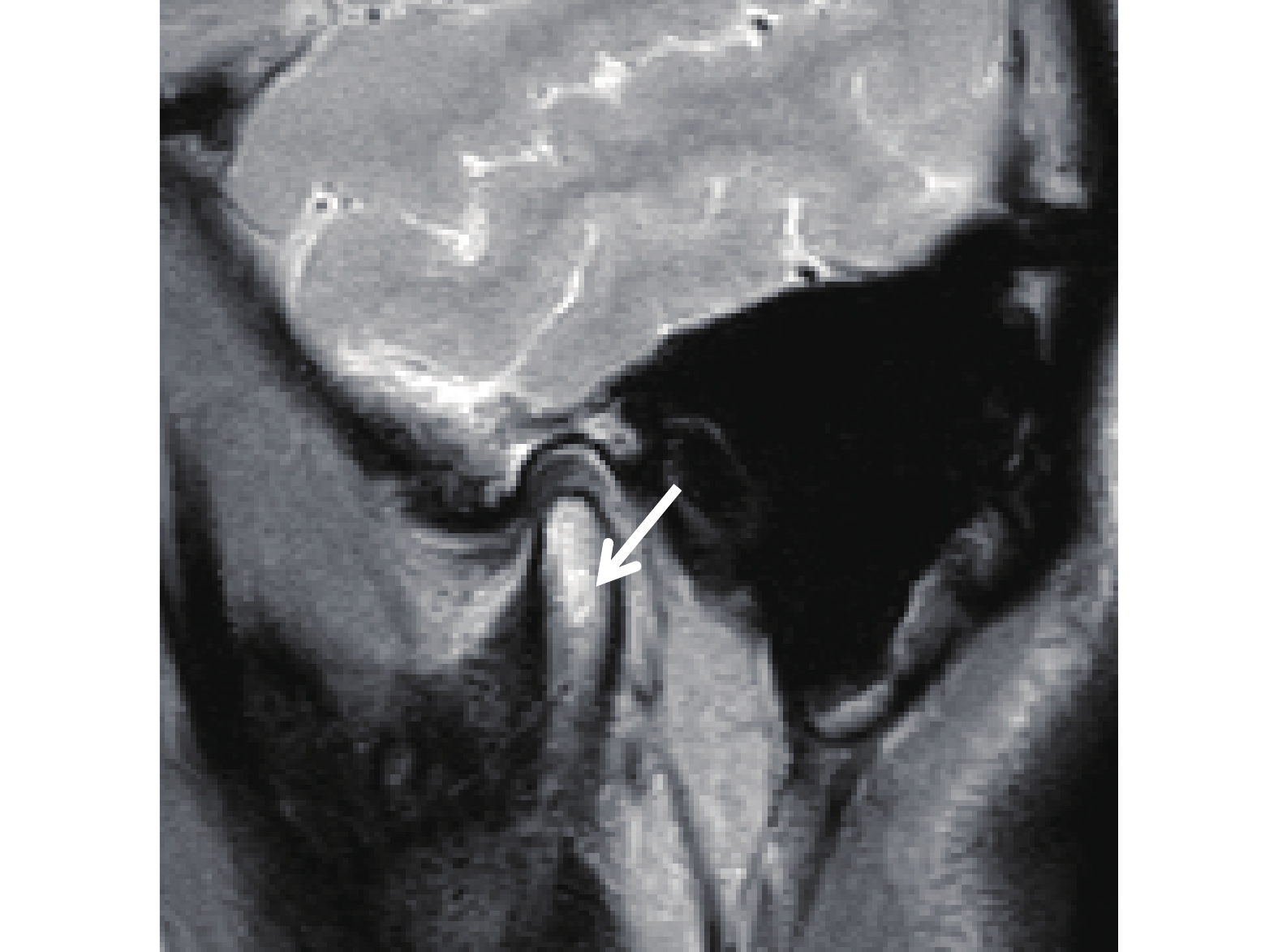
目的 探讨磁共振成像(magnetic resonance imaging,MRI)在无髁突骨折的颞颌关节即刻损伤后的潜在诊断价值。 方法 选取云南大学附属医院口腔颌面外科2018年6月至2021年3月收治的无髁突骨折的颞下颌关节损伤患者36例,共72侧关节纳入研究。所有的患者锥形束CT结果均显示髁突及关节窝无骨折且伤后髁突表面骨质“完整”。患者伤前均无关节疾患,伤后均出现不同程度的关节区疼痛和张口受限及弹响,其中24例合并有面部及其他部位的骨折。通过MRI对纳入患者进行影像检查,并对结果进行分析。 结果 MRI检查显示有关节48侧关节发生不同程度损伤,发生率为66.7%。损伤类型为骨髓水肿12侧(25%),关节盘后区损伤撕裂27侧(56.25%),关节盘移位33侧(68.75%)以及关节腔积血、积液36侧(75%)。关节盘后区损伤撕裂,关节盘移位,关节腔积血(积液)与骨髓水肿的发生率相比较,前3者发病率明显高于骨髓水肿,差异有统计学意义( P < 0.05)。 结论 MRI在无髁突骨折的颞颌关节即刻损伤后,能清楚的显示出关节软组织的损伤部位和类型。此外,在这些损伤中关节盘后区损伤撕裂,关节盘移位,关节腔积血(积液)与骨髓水肿的发生率相比较,前三者发生率明显高于骨髓水肿。MRI是无髁突骨折的颞颌关节即刻损伤后重要检查和评价手段。 -
关键词:
- 磁共振成像(MRI) /
- 锥形束CT /
- 无髁突骨折 /
- 颞颌关节
Abstract:Objective To investigate the diagnostic value of MRI in immediate injury of temporomandibular joint without condylar fracture. Methods 36 patients with temporomandibular joint injury without condylar fracture treated in the Department of Oral and Maxillofacial Surgery of the Affiliated Hospital of Yunnan University from June 2018 to March 2021 were selected, with a total of 72 joints included in the study. Cone beam CT results of all patients showed that there was no fracture of condyle and articular fossa, and the bone on the surface of condyle was “complete” after injury. All patients had no history of joint diseases. After injury, they had varying degrees of joint pain, limited opening and popping. Among them, 24 cases were complicated with fractures of face and other parts. The included patients were examined by MRI, and the results were statistically analyzed. Results MRI showed that 48 joints had different degrees of injury, and the incidence was 66.7%. The injury types included 12 joints with bone marrow edema (25%), 27 joints with posterior disc tear (56.25%), 33 joints with disc displacement (68.75%), and 36 joints with joint cavity hematocele and effusion (75%). The incidence of posterior disc disruption, disc displacement, and intraarticular blood accumulation (bone effusion) were significantly higher than those of bone marrow edema( P <0.05). Conclusion MRI can clearly show the location and type of injury of joint soft tissue after immediate injury of temporomandibular joint without condylar fracture. In addition, in these injuries, the incidence of posterior disc tear, disc displacement, joint cavity hematocele (effusion) was significantly higher than that of bone marrow edema. MRI is an important examination and evaluation method after immediate injury of temporomandibular joint without condylar fracture. -
表 1 患者的基本资料
Table 1. Basic information of the patients
项目 性别 致伤因素 面部相关损伤 男 女 摔伤 车祸 运动 高坠伤 伴有颏部裂伤或
下颌正中骨折全面部
骨折同侧颧骨
颧弓骨折同侧耳区鼓板
骨折,外耳道出血病例数(n) 21 15 12 12 9 3 27 3 3 3 构成比(%) 58.33 41.67 33.33 33.33 25.00 8.33 75.00 8.33 8.33 8.33 表 2 颞下颌关节即刻损伤的MRI评价
Table 2. MRI evaluation of immediate injury of temporomandibular joint
MRI评价 损伤侧数(侧) 发生率(%) 骨髓水肿(A) 12/48 25.00 关节盘后区损伤撕裂(B) 27/48 56.25* 关节盘移位(C) 33/48 68.75* 关节腔积血(液)(D) 36/48 75.00* 与A组比较,*P < 0.05。 -
[1] Merrill R G. Discussion. the arthroscopic appearance of acute temporomandibular joint trauma[J]. J Oral Maxillofac Surg,2019,48(8):780-784. [2] Sullivan S M,Banghart P R,Anderson Q. Magnetic resonance imaging assessment of acute soft tissue injuries to the temporomandibular joint[J]. J Oral Maxillofac Surg,2015,53(7):763-766. [3] Emshoff R,Rudisch A,Ennemoser T,et al. Magnetic resonance imaging finding s of temporomandibular joint soft tissue changes in type V and VI condylar injuries[J]. J Oral Maxillofac Surg,2007,65(8):1550-1554. doi: 10.1016/j.joms.2006.10.068 [4] Wang P,Yang J,Yu Q. MR imaging assessment of temporo[1]mandibular joint soft tissue injuries in dislocated and nondislo[1]cated mandibular condylar fractures[J]. AJNR Am J Neuroradiol,2019,30(1):59-63. [5] 徐淑江. 不同方法治疗儿童下颌骨髁突骨折效果观察[J]. 河南外科学杂志,2018,24(3):142-144. [6] Gerhard S,Ennemoser T,Rudisch A,et al. Condylar injury:Magnetic resonance imaging finds oftemporomandibular joint soft tissue changes[J]. Int J Oral Maxillofac Surg,2017,36(3):214-218. [7] 王靖虎,邓 勇,方一鸣,等. 颞下颌关节损伤的早期MRI表现[J]. 口腔医学研究,2008,24(4):443-517. [8] 初晓阳,张颜,田树平,等. 髁突骨折急性期颞下颌关节MRI表现[J]. 临床误诊误治,2013,26(12):43-45. [9] 张军. 下颌骨骨折的诊治进展J]. 北京口腔医学杂志,2016,24(3):170-173. [10] Han C,Dilxat D,Zhang X,et al. Does intraoperative navigation improve the anatomical reduction of intracapsular condylar fractures[J]. J Oral Maxillofac Surg,2018,76(12):2583-2591. doi: 10.1016/j.joms.2018.07.030 [11] 朱晸,史俊. 儿童下颌骨髁突骨折的治疗进展[J]. 国际口腔医学杂志,2017,44(2):222-227. doi: 10.7518/gjkq.2017.02.022 [12] Luz J G,Jaeger R G,de Araújo V C,et al. The effect of indirect trauma on the rat temporomandibular joint.[J]. International Journal of Oral and Maxillofacial Surgery,1991,20(1):48-52. doi: 10.1016/S0901-5027(05)80697-6 [13] Ying B B,Zhang Q Q,Zhu S S,et al. Outcomes of treatment for intracap-sular fractures of the mandibular condyle:Recommendation for a new classification[J]. Br J Oral Maxillofac Surg,2018,56(2):139-143. doi: 10.1016/j.bjoms.2018.01.002 [14] Dreizin D,Nam A J,Tirada N,et al. Multidetector CT of mandibular fractures,reductions,and complications:A clinically relevant primer for the radiologist[J]. Radiographics,2016,36(5):1539-1564. doi: 10.1148/rg.2016150218 [15] Tripathi R,Sharma N,Dwivedi A N,et al. Severity of soft tissue injury within the temporomandibular joint following condylar fracture as seen on magnetic resonance imaging and its impact on outcome of functional management[J]. J Oral Maxillofac Surg,2015,73(12):2371-2379. [16] 傅开元. 颞下颌关节紊乱病影像学检查的必要性以及存在的问题[J]. 中华口腔医学杂志,2019,58(8):505-509. [17] Jaryna Eder,Pavol Szomolanyi,Martina Schmid-Schwap,et al. Early diagnosis of degenerative changes in the articular/fibrocartilaginous disc of the temporomandibular joint in patients with temporomandibular disorders using delayed gadolinium-enhanced MRI at 3 Tesla-preliminary results[J]. Magn Reson Imaging,2020,67:24-27. [18] 裴宇文,曾春光,杨光明,等. 颞下颌关节紊乱综合征的 MRI 诊断价值[J]. 江西医药,2020,55(10):1522-1523. doi: 10.3969/j.issn.1006-2238.2020.10.058 [19] 郑有华,张志光,孔繁军,等. 颞下颌关节盘移位中国专家共识研讨会纪要[J]. 中华口腔医学杂志,2017,52(7):443-444. doi: 10.3760/cma.j.issn.1002-0098.2017.07.010ZHENG Youhua,ZHANG Zhiguang,KONG Fanjun,et al. Summary of Chinese expert consensus workshop on temporomandibular joint disc displacement[J]. Chinese Journal of Stomatology,2017,52(7):443-444. doi: 10.3760/cma.j.issn.1002-0098.2017.07.010 [20] Matsubara R,Yanagi Y,Oki K,et al. Assessment of MRI findings and clinical symptoms in patients with temporomandibular joint disorders[J]. Dentomaxillofac Radiol,2018,47(4):1-8. [21] 陈建中,杨春,王维琦,等. 下颌骨三维有限元模型分析模拟咬合创伤对髁突的力学影响[J]. 昆明医科大学学报,2018,39(6):82-85. doi: 10.3969/j.issn.1003-4706.2018.06.017 [22] 何冬梅,杨驰,陈敏洁,等. 无髁突骨折颞下颌关节急性创伤后的变化:影像学和手术所见[J]. 中国口腔颌面外科杂志,2011,9(4):301-303. -






 下载:
下载: