Relationship between Latent Class of Frailty and Symptom Distress in Lung Cancer Radiotherapy Patients
-
摘要:
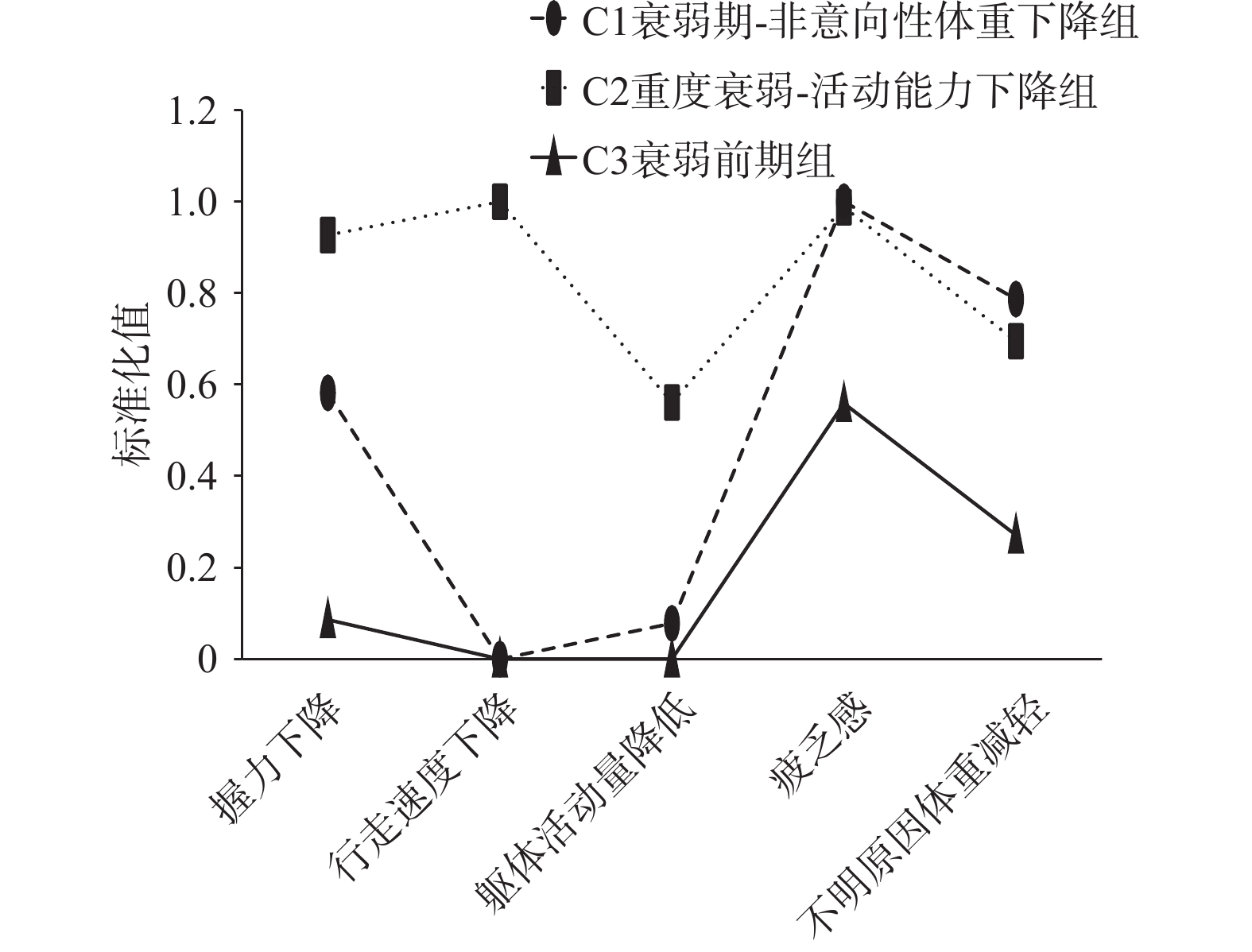
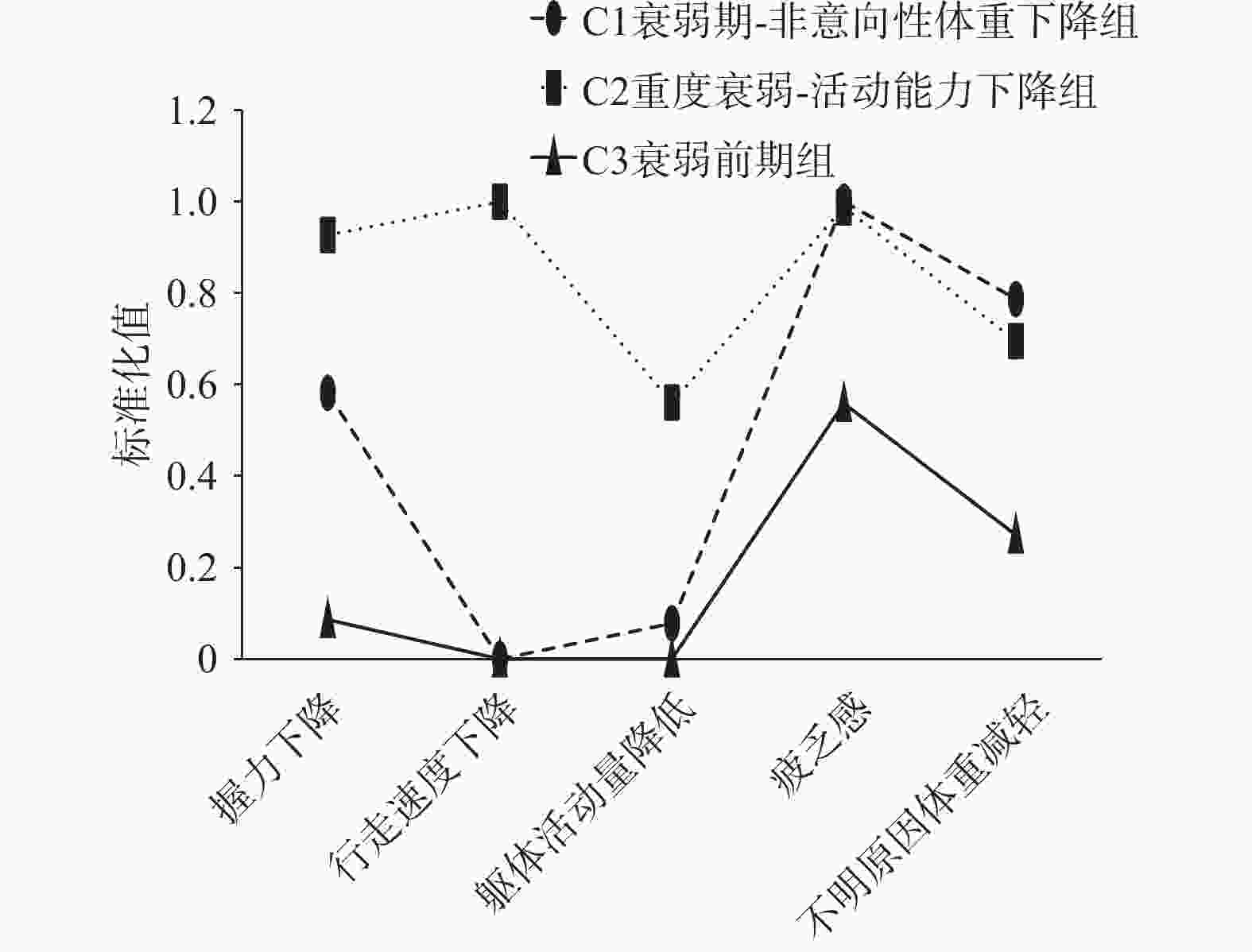
目的 分析肺癌放疗患者衰弱的潜在类别和影响因素,并探讨不同类别与症状困扰的关系。 方法 采用方便抽样法选取2023年4月至12月云南省某三级甲等肿瘤专科医院放射治疗科收治的241名肺癌放疗患者,采用肺癌放疗患者一般资料调查问卷、衰弱表型量表、安德森症状评估量表、营养风险筛查2002进行问卷调查,采用潜在类别分析肺癌放疗患者不同人群衰弱的内部异质性,和多分类Logistic回归分析探讨其衰弱内部异质性的影响因素,采用广义线性模型分析不同类别衰弱对患者症状困扰的影响。 结果 肺癌放疗患者衰弱可呈现3个潜在类别:衰弱前期组(30.29%)、衰弱期-非意向性体重下降组(35.68%)、重度衰弱-活动能力下降组(34.02%);放疗次数(P < 0.05)、年龄(P < 0.05)、营养风险评分(P < 0.05)是肺癌放疗患者衰弱潜在类别的影响因素;肺癌放疗患者衰弱潜在类别是症状困扰得分的影响因素(P < 0.001)。 结论 肺癌放疗患者衰弱存在人群异质性,不同类别间影响因素各异,衰弱潜在类别是症状困扰得分的影响因素。 Abstract:Objective To analyze potential latent class of frailty and influencing factors in lung cancer radiotherapy patients, and to explore the relationship between different frailty categories and symptom distress. Methods A convenience sampling method was used to recruit 241 lung cancer radiotherapy patients admitted to the Radiotherapy Department of a tertiary Grade-A oncology hospital in Yunnan Province from April to December 2023. Data were collected using questionnaires including: general demographic survey of lung cancer radiotherapy patients, frailty phenotype scale, Anderson Symptom Assessment Scale, and Nutritional Risk Screening 2002. Latent class analysis was employed to identify heterogeneity of frailty among different populations of lung cancer radiotherapy patients. Multinomial logistic regression analysis was used to explore factors influencing the internal heterogeneity of frailty. Generalized linear modeling was applied to analyze the impact of different frailty classes on patients' symptom burden. Results Results: Frailty in lung cancer radiotherapy patients presented three latent classes: pre-frailty group (30.29%), frailty with unintentional weight loss group (35.68%), and severe frailty with decreased physical activity group (34.02%). Radiotherapy frequency (P < 0.05), age (P < 0.05), and nutritional risk score (P < 0.05) were identified as influencing factors for latent classes of frailty. Latent frailty classes were significant predictors of symptom burden scores (P < 0.001). Conclusion Frailty in lung cancer radiotherapy patients demonstrates population heterogeneity, with varying influencing factors across different classes. Latent frailty classes significantly impact symptom burden scores. -
Key words:
- Lung cancer /
- Radiotherapy /
- Enervation /
- Potential categories /
- Symptom disturbance
-
表 1 肺癌放疗患者疾病及人口学资料[n(%)]
Table 1. Disease and demographic data of lung cancer patients undergoing radiotherapy [n(%)]
项目 选项 人数 性别 男 187(77.59) 女 54(22.41) 年龄(岁) <60 134(55.60) ≥60 107(44.40) 文化程度 小学及以下 92(38.17) 初中 78(32.37) 高中或中专 41(17.01) 大专及以上 30(12.45) 婚姻状况 已婚 214(88.80) 其他(离异、
丧偶、未婚)27(11.20) 职业 农民 143(59.34) 工人 23(9.54) 职员 19(7.88) 无业或退休 56(23.24) 居住地 城镇 107(44.40) 农村 134(55.60) 家庭人均月收入(元) <2000 112(46.48) 2000~ 3999 63(26.14) 4000 ~5999 33(13.69) ≥ 6000 33(13.69) 医疗费支付方式 职工医保 85(35.27) 居民医保 156(64.73) 肺癌细胞分型 鳞癌 59(24.48) 腺癌 112(46.47) 小细胞肺癌 53(21.99) 其他 17(7.06) 疾病分期 II期 23(9.54) III期 138(57.26) IV期 80(33.20) 转移情况 局部转移 159(65.98) 远处转移 82(34.02) 有无合并其他慢性
疾病(种)无 197(81.74) ≥1种 44(18.26) 曾接受何种治疗 手术 21(8.71) 化疗 157(65.15) 手术+化疗 39(16.18) 靶向/免疫/
中医治疗24(9.96) 睡眠情况 正常 171(70.95) 异常 70(29.05) 病程(月) ≤12 114(47.30) >12 127(52.70) 放疗次数(次) <10 101(41.91) 10~19 67(27.80) ≥20 73(30.29) 营养风险(分) <3 131(54.36) ≥3 110(45.64) 表 2 肺癌放疗患者衰弱、症状困扰、营养风险得分[n = 241,M(P25,P75),分]
Table 2. Scores of frailty,symptom distress and nutritional risk in lung cancer patients undergoing radiotherapy[n = 241,M(P25,P75),points]
变量 得分 衰弱表型量表 2.00(1.00,4.00) 营养风险评分 2.00(1.00,4.00) 安德森症状评估量表 45.00(17.00,75.00) 表 3 肺癌放疗患者衰弱潜在类别模型拟合信息适配指标
Table 3. Fitness indicators of frailty latent class model for lung cancer patients undergoing radiotherapy
模型 AIC BIC aBIC Etropy LMR(P) BLRT(P) 类别概率(%) 1 1438.013 1455.437 1439.588 1 2 1235.730 1274.063 1239.195 0.854 <0.001 <0.001 0.353,0.647 3 1213.262 1272.503 1218.617 0.812 <0.001 <0.001 0.357,0.340,0.303 4 1216.252 1296.403 1223.498 0.849 0.0047 0.0500 0.336,0.357,0.004,0.303 5 1226.436 1327.495 1235.571 0.837 0.6485 1.0000 0.349,0.012,0.332,0.004,0.303 表 4 肺癌放疗患者3个衰弱潜在类别单因素分析[n(%)](1)
Table 4. Univariate analysis of three potential classes of frailty in lung cancer patients undergoing radiotherapy[n(%)](1)
项目 C1(n =86) C2(n =82) C3(n =73) χ2/H P 性别 男 73(84.88) 62(75.61) 52(71.23) 4.513 0.105 女 13(15.12) 20(24.39) 21(28.77) 年龄(岁) <60 47(54.65) 33(40.24) 54(73.97) 17.846 <0.001* ≥60 39(45.35) 49(59.76) 19(26.03) 文化程度 小学及以下 38(44.19) 27(32.92) 27(36.99) 2.446 0.294 初中 26(30.23) 25(30.49) 27(36.99) 高中或中专 11(12.79) 20(24.39) 10(13.69) 大专及以上 11(12.79) 10(12.20) 9(12.33) 婚姻状况 已婚 77(89.53) 68(82.93) 69(94.52) 5.529 0.071 其他(离异、丧偶、未婚) 9(10.47) 14(17.07) 4(5.48) 职业 农民 59(68.60) 36(43.90) 48(65.75) 17.395 0.008* 工人 6(6.98) 9(10.98) 8(10.96) 职员 7(8.14) 6(7.32) 6(8.22) 无业或退休 14(16.28) 31(37.80) 11(15.07) 居住地 9.299 0.062 城镇 31(36.04) 46(56.10) 30(41.10) 农村 55(63.96) 36(43.90) 43(58.90) C1:衰弱期-非意向性体重下降组;C2:重度衰弱-活动能力下降组;C3:衰弱前期组;*P < 0.05。 4 肺癌放疗患者3个衰弱潜在类别单因素分析[n(%)](2)
4. Univariate analysis of three potential classes of frailty in lung cancer patients undergoing radiotherapy[n(%)](2)
项目 C1(n =86) C2(n =82) C3(n =73) χ2/H P 家庭人均月收入(元) <2000 47(54.65) 28(34.15) 37(50.68) 10.792 0.095 2000~ 3999 18(20.93) 24(29.27) 21(28.77) 4000 ~5999 9(10.47) 17(20.73) 7(9.59) ≥ 6000 12(13.95) 13(15.85) 8(10.96) 医疗费支付方式 职工医保 22(25.58) 41(50.00) 22(30.14) 12.172 0.002* 居民医保 64(74.42) 41(50.00) 51(69.86) 肺癌细胞分型类型 鳞癌 25(29.07) 18(21.95) 16(21.92) 3.393 0.686 腺癌 34(39.53) 39(47.56) 39(53.42) 小细胞肺癌 20(23.26) 20(24.39) 13(17.81) 其他 7(8.14) 5(6.10) 5(6.85) 疾病分期 II期 9(10.47) 5(6.10) 9(12.33) 15.162 0.001* III期 54(62.79) 36(43.90) 48(65.75) IV期 23(26.74) 41(50.00) 16(21.92) 转移情况 局部转移 62(72.09) 40(48.78) 57(78.08) 17.001 <0.001* 远处转移 24(27.91) 42(51.22) 16(21.92) 有无合并其他慢性疾病(种) 无 73(84.88) 61(74.39) 63(86.30) 4.536 0.103 ≥1种 13(15.12) 21(25.61) 10(13.70) 曾接受何种治疗 手术 8(9.30) 6(7.31) 7(9.59) 0.451 0.930 化疗 52(60.47) 60(73.17) 45(61.64) 手术+化疗 17(19.76) 7(8.54) 15(20.55) 靶向/免疫/中医治疗 9(10.47) 9(10.98) 6(8.22) 睡眠情况 正常 64(74.42) 55(67.07) 52(71.23) 1.103 0.576 异常 22(25.58) 27(32.93) 21(28.77) 病程(月) ≤12 41(47.67) 33(40.24) 40(54.79) 3.288 0.193 >12 45(52.33) 49(59.76) 33(45.21) 放疗次数(次) <10 29(33.72) 14(17.07) 58(79.45) 29.530 <0.001* 10~19 27(31.40) 30(36.59) 10(13.70) ≥20 30(34.88) 38(46.34) 5(6.85) 营养风险(分) <3 40(46.51) 24(29.27) 67(91.78) 63.880 <0.001* ≥3 46(53.49) 58(70.73) 6(8.22) C1:衰弱期-非意向性体重下降组;C2:重度衰弱-活动能力下降组;C3:衰弱前期组;*P < 0.05。 表 5 多因素Logistic回归分析自变量赋值表
Table 5. Multivariate Logistic regression analysis of independent variable assignment table
变量名 赋值 年龄(岁) <60=0,≥60=2 从事职业 农民=0,工人=1,职员=2,无业或退休=3 医疗费支付方式 职工医保=0,居民医保=1 疾病分期(期) II=0,III=1,IV=2 营养风险评分(分) <3=0,≥3=1 放疗次数(次) <10=0,10~19=1,≥20=2 表 6 肺癌放疗患者衰弱3个潜在类别多分类Logistic回归分析
Table 6. Multinomial Logistic regression analysis of three latent categories of frailty in lung cancer patients undergoing radiotherapy
类别比较 自变量 β SE Wald P OR 95%CI C1vsC3比较 常量 4.182 1.089 14.750 0.001* 放疗次数(≥20次为参照) <10 −2.502 0.600 17.389 <0.001* 0.082 0.025~0.265 营养风险评分(≥3分为参照) <3 −2.334 0.517 20.337 <0.001* 0.097 0.035~0.267 C2vsC3比较 常量 6.150 1.192 26.635 <0.001* 营养风险评分(≥3分为参照) <3 −2.807 0.562 24.957 <0.001* 0.060 0.020~0.182 放疗次数(≥20次为参照) <10 −3.756 0.687 29.896 <0.001* 0.023 0.006~0.090 10~19 −1.550 0.706 4.816 0.028* 0.212 0.053~0.847 年龄(≥60岁为参照) <60 −1.182 0.497 5.662 0.017* 0.307 0.116~0.812 C2vsC1比较 常量 1.968 0.782 6.326 0.012* 放疗次数(≥20次为参照) 放疗次数<10 −1.254 0.408 7.182 0.007* 0.285 0.114~0.714 注: C1:衰弱期-非意向性体重下降组;C2:重度衰弱-活动能力下降组;C3:衰弱前期组;*P < 0.05。 表 7 不同衰弱类别肺癌放疗患者症状困扰得分单因素分析[n = 241,M(P25,P75),分]
Table 7. Univariate analysis of symptom distress scores of lung cancer patients undergoing radiotherapy in different frailty categories[n = 241,M(P25,P75),points]
项目 得分 H P 肺癌放疗患者衰弱潜在类别 C1衰弱期-非意向性体重下降组 57.00(36.00,98.00) 92.094 <0.001* C2重度衰弱-活动能力下降组 75.00(62.00,107.00) C3衰弱前期 17.00(7.00,35.00) *P < 0.05。 表 8 肺癌放疗患者衰弱潜在类别与症状困扰评分广义线性模型分析 (n = 241)
Table 8. Generalized linear model analysis of latent classes of frailty and symptom distress score in lung cancer patients undergoing radiotherapy (n = 241)
变量 β SE 95%CI Waldχ2 P 截距 19.178 3.5394 12.241~26.115 29.360 <0.001* 衰弱期-非意向性体质量下降组 35.741 4.8126 26.308~45.173 55.153 <0.001* 重度衰弱-活动能力下降组 54.005 4.8662 44.467~63.542 123.167 <0.001* *P < 0.05。 -
[1] Bray F, Laversanne M, Sung H, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2024, 74(3): 229-263. [2] Ethun C G, Bilen M A, Jani A B, et al. Frailty and cancer: Implications for oncology surgery, medical oncology, and radiation oncology[J]. CA Cancer J Clin, 2017, 67(5): 362-377. [3] Komici K, Bencivenga L, Navani N, et al. Frailty in patients with lung cancer: A systematic review and meta-analysis[J]. Chest, 2022, 162(2): 485-497. doi: 10.1016/j.chest.2022.02.027 [4] Chen K, Yang D, Li F, et al. Changes in the symptom clusters of elderly patients with lung cancer over the course of postoperative rehabilitation and their correlation with frailty and quality of life: A longitudinal study[J]. Eur J Oncol Nurs, 2023, 67: 102388. doi: 10.1016/j.ejon.2023.102388 [5] Mathur S, Prince L, Bucher O, et al. The impact of the modified frailty index on clinical outcomes for patients with stage IV non-small cell lung cancer receiving chemotherapy[J]. J Geriatr Oncol, 2022, 13(5): 654-661. doi: 10.1016/j.jgo.2022.02.015 [6] Armstrong T S. Symptoms experience: A concept analysis[J]. Oncol Nurs Forum, 2003, 30(4): 601-606. doi: 10.1188/03.ONF.601-606 [7] Chen Z, He G, Zhao Y, et al. Symptom burden and emotional distress in advanced lung cancer: The moderating effects of physicians' communication skills and patients' disease understanding[J]. Support Care Cancer, 2022, 30(11): 9497-9505. [8] 田晓宇. 社区老年人疼痛与衰弱的关系: 抑郁的中介作用及其与疼痛的交互作用[D]. 济南: 山东大学, 2018. [9] Jia S, Zhao W, Zhang Y, et al. Multiple physical symptoms of community-dwelling older people in western China: Prevalence and its association with frailty[J]. Gerontology, 2021, 67(3): 290-298. doi: 10.1159/000513246 [10] Kirkhus L, Šaltytė Benth J, Grønberg B H, et al. Frailty identified by geriatric assessment is associated with poor functioning, high symptom burden and increased risk of physical decline in older cancer patients: Prospective observational study[J]. Palliat Med, 2019, 33(3): 312-322. doi: 10.1177/0269216319825972 [11] Han C J, Rosko A E, Spakowicz D J, et al. Associations of frailty with symptoms, and HRQOL in older cancer survivors after cancer treatments: A systematic review and meta-analyses[J]. Qual Life Res, 2024, 33(3): 583-598. doi: 10.1007/s11136-023-03537-4 [12] 董懂, 黄意恒, 张亚杰, 等. 中华医学会肺癌临床诊疗指南(2023版)解读[J]. 中华胸心血管外科临床杂志, 2023, (11): 1533-1538. [13] 刘源, 刘红云. 非连续性与异质性——多阶段混合增长模型在语言发展研究中的应用[J]. 华东师范大学学报(教育科学版), 2018, 36(1): 137-148+166. doi: 10.16382/j.cnki.1000-5560.2018.01.017 [14] Fried L P, Tangen C M, Walston J, et al. Frailty in older adults: Evidence for a phenotype[J]. J Gerontol A Biol Sci Med Sci, 2001, 56(3): M146-M156. doi: 10.1093/gerona/56.3.M146 [15] 徐婉莹, 王霄, 岳跃学, 等. 体感游戏康复运动对社区老年人衰弱及平衡能力的影响[J]. 护理学杂志, 2024, 39(14): 1-5. [16] 韩君, 王君俏, 谢博钦, 等. Fried衰弱表型和FRAIL量表及埃德蒙顿衰弱评估量表在社区高龄老年人衰弱筛查中一致性和适用性的比较研究[J]. 中国全科医学, 2021, 24(21): 2669-2675. [17] 斯彩娟, 王卫光, 洪秀芳, 等. NRS2002、SGA在恶性肿瘤住院患者营养筛查与评估中的应用[J]. 浙江医学, 2021, 43(11): 1192-1195. [18] 夏萍, 史俏蓉, 霍永忠, 等. 欧洲营养风险筛查方法NRS-2002简介及应用现状[J]. 现代预防医学, 2007, 34(15): 2860-2861, 2866. [19] Cleeland C S, Mendoza T R, Wang X S, et al. Assessing symptom distress in cancer patients: The M. D. Anderson Symptom Inventory[J]. Cancer, 2000, 89(7): 1634-1646. doi: 10.1002/1097-0142(20001001)89:7<1634::AID-CNCR29>3.0.CO;2-V [20] 王德生, 王爱平. 安德森症状评估量表在癌症病人症状群研究中的应用[J]. 护理研究, 2013, 27(19): 1923-1924. [21] Green M J. Latent class analysis was accurate but sensitive in data simulations[J]. J Clin Epidemiol, 2014, 67(10): 1157-1162. doi: 10.1016/j.jclinepi.2014.05.005 [22] Zhang Q, Ip E H. Variable assessment in latent class models[J]. Comput Stat Data Anal, 2014, 77: 146-156. doi: 10.1016/j.csda.2014.02.017 [23] Ouyang J, Xu G. Identifiability of latent class models with covariates[J]. Psychometrika, 2022, 87(4): 1343-1360. doi: 10.1007/s11336-022-09852-y [24] Larsen R T, Turcotte L A, Westendorp R, et al. Frailty index status of Canadian home care clients improves with exercise therapy and declines in the presence of polypharmacy[J]. J Am Med Dir Assoc, 2020, 21(6): 766-771. e1. [25] Xu L, Zhang J, Shen S, et al. Association between body composition and frailty in elder inpatients[J]. Clin Interv Aging, 2020, 15: 313-320. doi: 10.2147/CIA.S243211 [26] Lin S , Wang F , Huang M , et al. Multidomain intervention for delaying aging in community-dwelling older adults (MIDA): Study design and protocol[J]. Annals of Medicine, 2025, 57(1): 2496409. [27] 冯静宜, 张雪芳, 周雪迎, 等. 老年衰弱患者真实体验质性研究的Meta整合[J]. 中华护理杂志, 2023, 58(23): 2928-2935. [28] 孙梦杰, 刘腊梅, 王佳南, 等. 老年慢性病患者医院-家庭过渡期真实经历与护理体验质性研究的Meta整合[J]. 中国全科医学, 2023, 26(28): 3565-3572. [29] O’Donovan A, Leech M, Gillham C. Assessment and management of radiotherapy induced toxicity in older patients[J]. J Geriatr Oncol, 2017, 8(6): 421-427. doi: 10.1016/j.jgo.2017.07.001 [30] 汪燃, 黄菲. 中老年肺癌患者胸部放疗期间症状群的调查及护理对策[J]. 中华护理杂志, 2023, 58(13): 1596-1602. [31] Wu Y, Liao W, Chen J, et al. Phosphate metabolic inhibition contributes to irradiation-induced myelosuppression through dampening hematopoietic stem cell survival[J]. Nutrients, 2022, 14(16): 3395. doi: 10.3390/nu14163395 [32] Kiss N, Curtis A. Current insights in nutrition assessment and intervention for malnutrition or muscle loss in people with lung cancer: A narrative review[J]. Adv Nutr, 2022, 13(6): 2420-2432. doi: 10.1093/advances/nmac070 [33] Hazell S Z, Mai N, Fu W, et al. Hospitalization and definitive radiotherapy in lung cancer: Incidence, risk factors and survival impact[J]. BMC Cancer, 2020, 20(1): 334. doi: 10.1186/s12885-020-06843-z [34] 杨振, 张会君. 社区老年慢性病患者认知衰弱风险预测模型的构建及验证[J]. 护理学杂志, 2021, 36(12): 86-89. [35] Kelaiditi E, Guyonnet S, Cesari M. Is nutrition important to postpone frailty?[J]. Curr Opin Clin Nutr Metab Care, 2015, 18(1): 37-42. [36] 罗宝林, 罗泽槟, 陈森芸, 等. 老年人衰弱预防与延迟或逆转干预的证据总结[J]. 护理学杂志, 2021, 36(14): 32-37. [37] Hou Y G, Feng S M, Wang S M, et al. The construction and validation of a frailty risk prediction model for older adults with lung cancer: A cross-sectional study[J]. Eur J Oncol Nurs, 2023, 64: 102316. [38] Rodríguez-Gómez I, Mañas A, Losa-Reyna J, et al. Prospective changes in the distribution of movement behaviors are associated with bone health in the elderly according to variations in their frailty levels[J]. J Bone Miner Res, 2020, 35(7): 1236-1245. doi: 10.1002/jbmr.3988 [39] Pandya C, Magnuson A, Flannery M, et al. Association between symptom burden and physical function in older patients with cancer[J]. J Am Geriatr Soc, 2019, 67(5): 998-1004. -





 下载:
下载: