Predictive Value of Serum miRNA-126a and miRNA-130b Levels in Cognitive Impairment among Patients with Diabetes Mellitus Complicated with Acute Stroke
-
摘要:
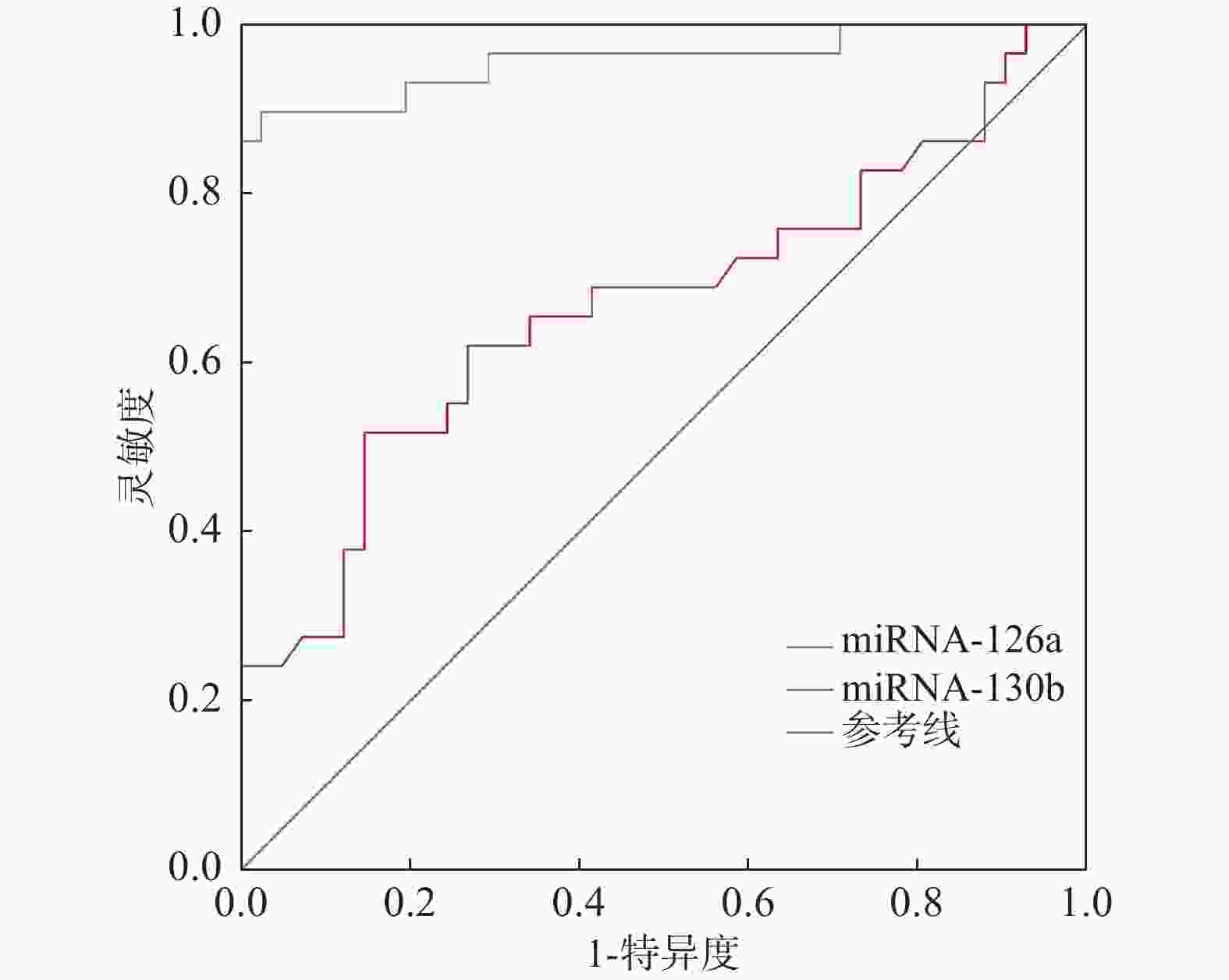
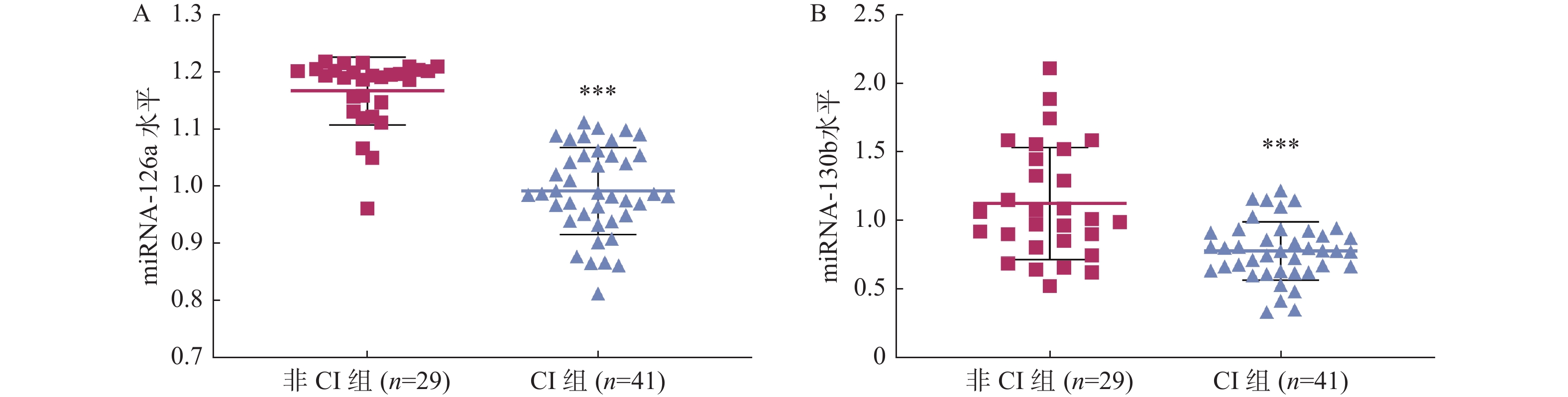
目的 探讨糖尿病(DM)合并急性脑卒中(AS)患者血清miRNA-126a、miRNA-130b水平与认知障碍(CI)的关系。 方法 对武汉市第一医院2019年1月至2021年12月收治的70例DM合并AS患者进行回顾性分析。根据是否发生CI,将患者分为CI组(n = 41)和非CI组(n = 29)。通过实时荧光定量PCR检测miRNA-126a、miRNA-130b在外周血中的相对表达水平。 结果 与非CI组比较,CI组的白蛋白增大(P < 0.05),miRNA-126a、miRNA-130b表达水平降低(P < 0.05)。Logistic回归分析显示,白蛋白(OR = 19.045,95%CI = 2.001~181.230)、miRNA-126a(OR = 200.603,95%CI = 15.663~ 2569.162 )、miRNA-130b(OR = 11.770,95%CI = 1.966~70.474)是影响DM合并AS患者CI发生的相关因素。ROC曲线检测外周血中miRNA-126a诊断DM合并AS患者CI发生具有最高的AUC(0.958),灵敏度和特异度分别为97.6%和89.7%。miRNA-130b诊断DM合并AS患者CI发生的AUC(0.669)较低,灵敏度和特异度分别为73.2%和62.1%。结论 外周血miRNA-126a表达降低对DM合并AS患者的CI具有良好的诊断价值。 Abstract:Objective To explore the relationship between serum miRNA-126a, miRNA-130b levels and cognitive impairment (CI) in patients with diabetes mellitus (DM) complicated with acute stroke (AS). Methods A retrospective analysis was conducted on 70 DM patients with AS admitted to Wuhan First Hospital from January 2019 to December 2021. Patients were divided into CI group (41 cases) and non-CI group (29 cases) based on the occurrence of CI. Real-time fluorescence quantitative PCR was used to detect the relative expression levels of miRNA-126a and miRNA-130b in peripheral blood. Results Compared with non-CI group, the CI group showed increased albumin (P < 0.05) and decreased levels of miRNA-126a and miRNA-130b (P < 0.05). Logistic regression analysis showed that albumin (OR = 19.045, 95%CI = 2.001~181.230), miRNA-126a(OR = 200.603, 95%CI = 15.663~ 2569.162 ), miRNA-130b (OR = 11.770, 95%CI = 1.966~70.474) were related factors affecting CI occurrence in DM patients with AS. ROC curve analysis showed that peripheral blood miRNA-126a had the highest AUC (0.958) for diagnosing CI in DM patients with AS, with a sensitivity of 97.6% and specificity of 89.7%. The AUC for miRNA-130b (0.669) was lower, with a sensitivity of 73.2% and specificity of 62.1%.Conclusion Decreased expression of peripheral blood miRNA-126a has good diagnostic value for CI in DM patients with AS. -
Key words:
- Diabetes /
- Acute stroke /
- Peripheral blood /
- Cognitive impairment /
- microRNAs
-
表 1 CI组和非CI组的人口统计学和临床特征[($\bar x \pm s $)/n (%)]
Table 1. Demographic and clinical characteristics of CI and non-CI group [($\bar x \pm s $)/n (%)]
特征 非CI组(n = 29) CI组(n = 41) t/χ2 P 年龄(岁) 62.07 ± 15.10 68.32 ± 11.63 2.771 0.068 BMI(kg/m2) 21.37 ± 2.39 22.85 ± 3.21 2.691 0.073 NIHSS 3.72 ± 5.71 3.44 ± 3.50 0.259 0.797 男性 14(48.3) 22(53.7) 0.197 0.657 高血压 23(79.3) 31(75.6) 0.132 0.716 高脂血症 11(37.9) 16(39.0) 0.009 0.926 吸烟 13(44.8) 15(36.6) 0.481 0.488 冠心病 4(13.8) 4(9.8) 0.273 0.601 AS类型 1.611 0.204 脑梗塞 26(89.7) 32(78.0) 脑出血 3(10.3) 8(22.0) AS位置 0.214 0.643 幕下 5(17.2) 3(7.3) 皮下 22(75.9) 30(73.2) 皮质 2(6.9) 8(19.5) 实验室指标 白蛋白(g/dL) 3.52 ± 0.36 3.70 ± 0.32 2.267 0.027* 血糖(mg/dL) 120.10 ± 50.12 119.98 ± 55.98 0.010 0.992 总胆固醇(mg/dL) 161.79 ± 41.89 165.80 ± 36.16 1.584 0.115 甘油三酯(mg/dL) 109.76 ± 44.10 91.22 ± 48.69 1.631 0.108 HbA1c(%) 6.86 ± 2.56 6.44 ± 2.71 0.661 0.511 CRP(mg/dL) 1.91 ± 4.88 0.82 ± 2.45 1.229 0.223 miRNA-126a 1.17 ± 0.06 0.99 ± 0.08 183.2 <0.001* miRNA-130b 1.13 ± 0.41 0.78 ± 0.21 24.40 <0.001* *P < 0.05。 表 2 DM合并AS患者CI影响因素的Logistic回归分析
Table 2. Logistic regression analysis of influencing factors for CI in DM patients with AS
因素 B 标准误差 Wald χ2 P OR 95%CI 白蛋白 2.947 1.149 6.572 0.010* 19.045 2.001~181.230 miRNA-126a 5.301 1.301 16.603 <0.001* 200.603 15.663~ 2569.162 miRNA-130b 2.466 0.913 7.290 0.007* 11.770 1.966~70.474 常量 −4.820 1.329 13.164 <0.001* 0.008 *P < 0.05。 表 3 外周血miRNA-126a和miRNA-130b在糖尿病合并AS患者脑梗死诊断中的ROC特征
Table 3. Characteristics of peripheral blood miRNA-126a and miRNA-130b in cerebral infarction diagnosis of patients with diabetes mellitus complicated with AS
指标 AUC 截止值 P 95%CI 特异度(%) 灵敏度(%) miRNA-126a 0.958 1.108 0.000* 0.905~1.000 89.7 97.6 miRNA-130b 0.669 0.894 0.017* 0.533~0.805 62.1 73.2 *P < 0.05。 -
[1] Mosenzon O, Cheng A Y Y, Rabinstein A A, et al. Diabetes and stroke: What are the connections?[J]. J Stroke, 2023, 25(1): 26-38. doi: 10.5853/jos.2022.02306 [2] Lee K P, Chen J S, Wang C Y. Association between diabetes mellitus and post-stroke cognitive impairment[J]. J Diabetes Investig, 2023, 14(1): 6-11. doi: 10.1111/jdi.13914 [3] Xue B, Qu Y, Zhang X, et al. miRNA-126a-3p participates in hippocampal memory via Alzheimer’s disease-related proteins[J]. Cerebral Cortex, 2022, 32(21): 4763-4781. doi: 10.1093/cercor/bhab515 [4] Venkat P, Cui C, Chopp M, et al. MiR-126 mediates brain endothelial cell exosome treatment–induced neurorestorative effects after stroke in type 2 diabetes mellitus mice[J]. Stroke, 2019, 50(10): 2865-2874. doi: 10.1161/STROKEAHA.119.025371 [5] Qi Z, Liu R, Ju H, et al. microRNA-130b-3p attenuates septic cardiomyopathy by regulating the AMPK/mTOR signaling pathways and directly targeting ACSL4 against ferroptosis[J]. Int J Biol Sci, 2023, 19(13): 4223-4241. doi: 10.7150/ijbs.82287 [6] Aldous E K, Toor S M, Parray A, et al. Identification of novel circulating miRNAs in patients with acute ischemic stroke[J]. Int J Mol Sci, 2022, 23(6): 3387. doi: 10.3390/ijms23063387 [7] 汪凯, 董强, 郁金泰, 等. 卒中后认知障碍管理专家共识2021[J]. 中国卒中杂志, 2021, 16(4): 376-389. doi: 10.3969/j.issn.1673-5765.2021.04.011 [8] Maida C D, Daidone M, Pacinella G, et al. Diabetes and ischemic stroke: An old and new relationship an overview of the close interaction between these diseases[J]. Int J Mol Sci, 2022, 23(4): 2397. doi: 10.3390/ijms23042397 [9] Saceleanu V M, Toader C, Ples H, et al. Integrative approaches in acute ischemic stroke: From symptom recognition to future innovations[J]. Biomedicines, 2023, 11(10): 2617. doi: 10.3390/biomedicines11102617 [10] Mierzejewski B, Ciemerych M A, Streminska W, et al. miRNA-126a plays important role in myoblast and endothelial cell interaction[J]. Sci Rep, 2023, 13(1): 15046. doi: 10.1038/s41598-023-41626-z [11] Yu P, Venkat P, Chopp M, et al. Role of microRNA-126 in vascular cognitive impairment in mice[J]. J Cereb Blood Flow Metab, 2019, 39(12): 2497-2511. doi: 10.1177/0271678X18800593 [12] Kaundal R K, Datusalia A K, Sharma S S. Posttranscriptional regulation of Nrf2 through miRNAs and their role in Alzheimer's disease[J]. Pharmacol Res, 2022, 175: 106018. doi: 10.1016/j.phrs.2021.106018 [13] Karuga F F, Jaromirska J, Malicki M, et al. The role of microRNAs in pathophysiology and diagnostics of metabolic complications in obstructive sleep apnea patients[J]. Front Mol Neurosci, 2023, 16: 1208886. doi: 10.3389/fnmol.2023.1208886 [14] Wu J J, Weng S C, Liang C K, et al. Effects of kidney function, serum albumin and hemoglobin on dementia severity in the oldest old people with newly diagnosed Alzheimer’ s disease in a residential aged care facility: A cross-sectional study[J]. BMC Geriatr, 2020, 20(1): 391. doi: 10.1186/s12877-020-01789-0 [15] Shen J, Amari N, Zack R, et al. Plasma MIA, CRP, and albumin predict cognitive decline in Parkinson's disease[J]. Ann Neurol, 2022, 92(2): 255-269. doi: 10.1002/ana.26410 [16] Dimache A M, Șalaru D L, Sascău R, et al. The role of high triglycerides level in predicting cognitive impairment: A review of current evidence[J]. Nutrients, 2021, 13(6): 2118. doi: 10.3390/nu13062118 [17] Antal B, McMahon L P, Sultan S F, et al. Type 2 diabetes mellitus accelerates brain aging and cognitive decline: Complementary findings from UK Biobank and meta-analyses[J]. eLife, 2022, 11: e73138. doi: 10.7554/eLife.73138 [18] Chow Y Y, Verdonschot M, McEvoy C T, et al. Associations between depression and cognition, mild cognitive impairment and dementia in persons with diabetes mellitus: A systematic review and meta-analysis[J]. Diabetes Res Clin Pract, 2022, 185: 109227. doi: 10.1016/j.diabres.2022.109227 [19] Sluiman A J, McLachlan S, Forster R B, et al. Higher baseline inflammatory marker levels predict greater cognitive decline in older people with type 2 diabetes: Year 10 follow-up of the edinburgh type 2 diabetes study[J]. Diabetologia, 2022, 65(3): 467-476. doi: 10.1007/s00125-021-05634-w -






 下载:
下载: