Effects of ACBT Technique Combined with Resistance Breathing Training on Patients with AECOPD
-
摘要:
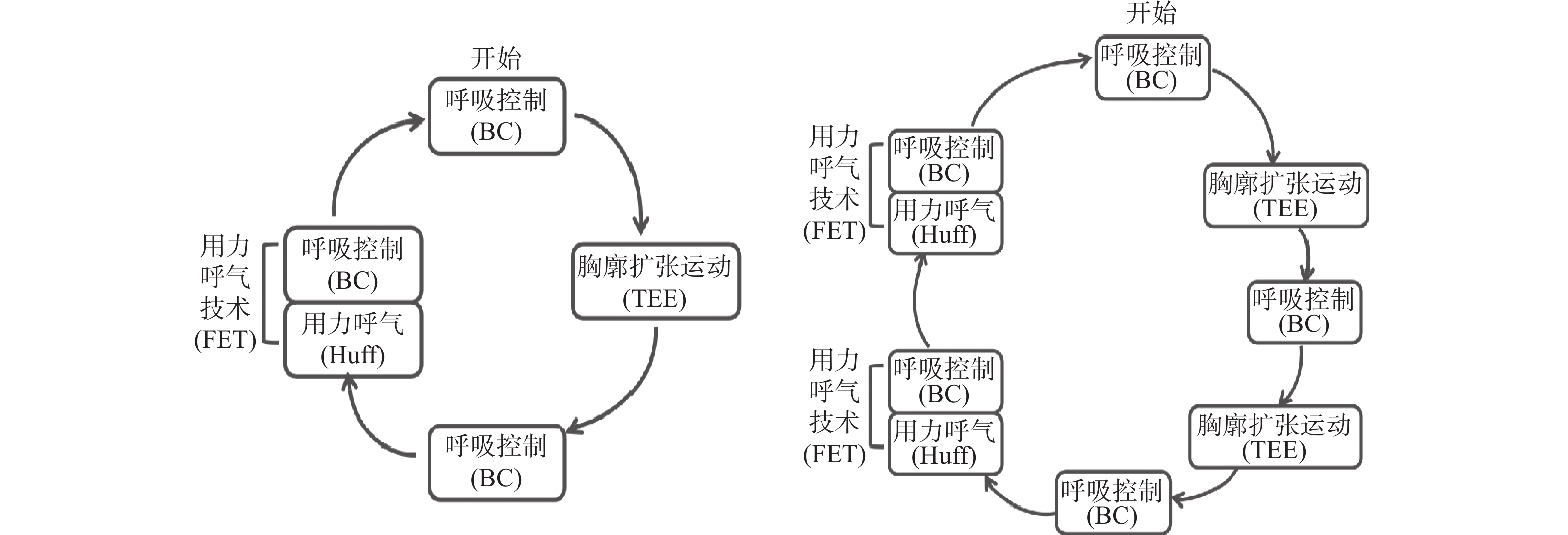
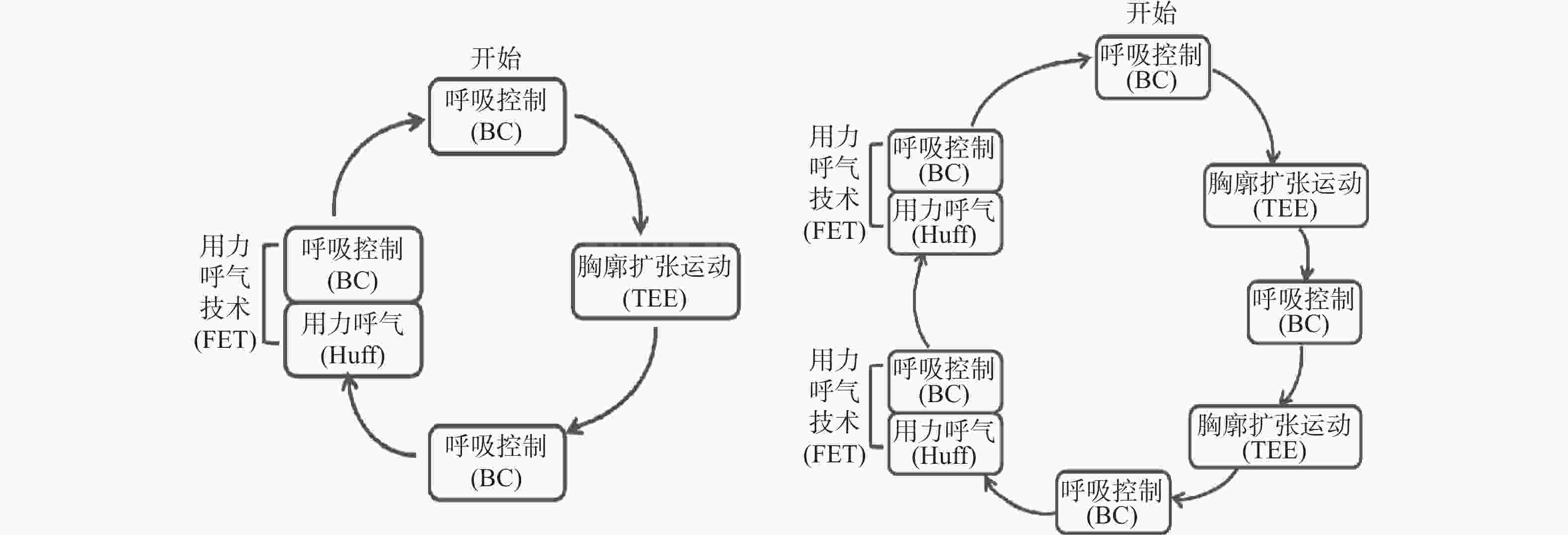
目的 探讨主动呼吸循环技术(ACBT)联合抗阻呼吸训练对慢性阻塞性肺疾病急性加重期(AECOPD)患者的肺功能和运动能力的影响。 方法 选取2024年1月至2024年5月昆明某三甲医院老年医学科住院的AECOPD患者60例作为研究对象。采用随机数列方式,将患者分成两组,每组30例。对照组接受常规肺康复护理,观察组实施ACBT技术联合抗阻呼吸训练,出院后4周收集患者的肺功能指标、改良的英国医学委员会呼吸困难量表(mMRC)评分、6MWT距离、CAT量表评价干预效果。 结果 进行干预后,观察组的肺功能、mMRC得分、6MWT以及CAT量表的指标均比干预前有显著提升,且均优于对照组(P < 0.05)。 结论 ACBT技术联合抗阻呼吸训练能更有效促进AECOPD患者排出痰液,降低呼吸肌疲劳,增加活动耐力,改善呼吸困难程度及肺功能。 -
关键词:
- 慢性阻塞性肺疾病急性加重期 /
- 主动呼吸循环技术 /
- 抗阻呼吸训练
Abstract:Objective To investigate the effects of active respiratory circulation technique (ACBT) combined with resistance breathing training on pulmonary function and exercise capacity in patients with acute exacerbations of chronic obstructive pulmonary disease (AECOPD). Methods A total of 60 hospitalized AECOPD patients from the Geriatrics Department of a tertiary hospital in Kunming were selected as research subjects from January to May 2024. Patients were randomly divided into two groups, with 30 patients in each group. The control group received conventional pulmonary rehabilitation nursing, and the observation group received ACBT combined with resistance breathing training. Pulmonary function indicators, modified British Medical Council(mMRC) dyspnea scores, 6-minute walk test (6MWT) distances, and the COPD Assessment Test (CAT) scores were collected 4 weeks after discharge to evaluate the intervention's effectiveness. Results After the intervention, the observation group showed significant improvements in lung function, mMRC scores, 6MWT distances, and CAT scores compared to pre-intervention levels, and all were superior to the control group (P < 0.05). Conclusion ACBT combined with resistance breathing training can more effectively promote sputum clearance, reduce respiratory muscle fatigue, increase exercise endurance, and improve dyspnea severity and lung function in AECOPD patients. -
表 1 两组患者基线资料比较(n = 60,$\bar x \pm s $)
Table 1. Comparison of baseline data between two patient groups (n = 60,$\bar x \pm s $)
组别 对照组 观察组 χ2/t P n 30 30 性别(男/女) 1911 2218 0.039 0.083 年龄(岁) 61.67 ± 2.96 62.00 ± 3.17 0.473 0.638 病程(年) 10.21 ± 2.35 10.21 ± 2.32 3.567 0.887 医疗保险(医保/自费) 2515 2713 0.144 0.704 COPD分级(Ⅱ级/Ⅲ级) 1614 1812 0.274 0.639 表 2 两组患者FEV1/FVC比较[(%),($\bar x \pm s $)]
Table 2. Comparison of FEV1/FVC between the two groups [(%),($\bar x \pm s $)]
组别 干预前 干预后 t P 对照组 52.85 ± 4.85 59.73 ± 6.09 −2.457 0.017 观察组 53.72 ± 5.13 64.92 ± 5.47 −2.339 0.023 t 0.791 3.768 P 0.432 0.003* *P < 0.05。 表 3 两组患者FEV1比较[L,($\bar x \pm s $)]
Table 3. Comparison of FEV1 between the two groups [L,($\bar x \pm s $)]
组别 干预前 干预后 t P 对照组 1.02 ± 0.16 1.21 ± 0.18 −2.244 0.029 观察组 1.06 ± 0.14 1.39 ± 0.16 −1.089 0.037* t 1.044 2.64 P 0.301 0.013* *P < 0.05。 表 4 两组患者mMRC评分比较($\bar x \pm s $)
Table 4. Comparison of mMRC between the two groups ($\bar x \pm s $)
组别 干预前 干预后 t P 对照组 3.43 ± 0.67 2.82 ± 0.65 3.516 0.016 观察组 3.50 ± 0.62 2.03 ± 0.68 6.026 0.001 t 0.791 −4.55 P 0.432 0.001* *P < 0.05。 表 5 两组患者6MWT距离比较[($\bar x \pm s $),m]
Table 5. Comparison of 6-minute walk distance between the two groups [($\bar x \pm s $),m]
组别 干预前 干预后 t P 对照组 244.87 ± 37.53 258.65 ± 34.95 −1.569 0.022 观察组 245.63 ± 60.92 289.89 ± 34.77 −5.024 0.001 t 0.085 3.412 P 0.932 0.001* *P < 0.05。 表 6 两组患者CAT评分比较($\bar x \pm s $)
Table 6. Comparison of CAT scores between the two groups ($\bar x \pm s $)
组别 干预前 干预后 t P 对照组 22.75 ± 9.76 19.48 ± 8.29 −2.731 0.029* 观察组 21.50 ± 8.95 15.85 ± 9.18 3.149 0.001* t 0.538 3.687 P 0.667 0.008* *P < 0.05。 -
[1] Global strategy for the diagnosis,management,and prevention of chronic obstructive pulmonary disease(2024 report)[EB/OL]. (2022-11-14) [2023-01-15]. [2] Fang L, Gao P, Bao H, et al. Chronic obstructive pulmonary disease in China: A nationwide prevalence study[J]. Lancet Respir Med,2018,6(6):421-430. [3] Xu J X,Ji Z L,Zhang P,et al. Disease burden of COPD in the Chinese population: A systematic review[J]. Therapeutic Advances in Respiratory Disease,2023,17: 17534666231218899. [4] Hartl S,Lopez-Campos J L,Pozo-Rodriguez F,et al. Risk of death and readmission of hospital-admitted COPD exacerbations: European COPD audit[J]. Eur Respir J,2016,47(1):113-121. [5] 潘铭. 拍背联合体外振动排痰方式对慢性阻塞性肺疾病急性加重期并发结核病患者的临床护理效果分析[J]. 中国防痨杂志,2024,46(S1):206-209. doi: 10.3969/j.issn.1000-6621.2024.z1.062 [6] Song J,Liu Z Z,Huang J,et al. Effects of aerobic exercise,traditional Chinese exercises,and meditation on depressive symptoms of college student: A meta-analysis of randomized controlled trials[J]. Medicine (Baltimore),2021,100(1):e23819. [7] Hoffman M,Assis M G,Augusto V M,et al. The effects of inspiratory muscle training based on the perceptions of patients with advanced lung disease: A qualitative study[J]. Braz J Phys Ther,2018,22(3):215-221. [8] 陈典,隆寰宇,李姝润,等. 2024年GOLD慢性阻塞性肺疾病诊断、治疗、管理及预防全球策略更新要点解读[J]. 中国全科医学,2024,27(13):1533-1543+1567. [9] 朱蕾,陈荣昌. 成人常规肺功能测定规范中国专家共识[J]. 临床肺科杂志,2022,27(11):1621-1633. [10] 刘思峰,张维亮,杨英杰,等. 一套更具可操作性的老年人能力评估体系[J]. 中国老年学杂志,2022,42(6):1475-1478. doi: 10.3969/j.issn.1005-9202.2022.06.056 [11] 李春阳,王佳佳,卫梦雨,等. 慢性阻塞性肺疾病急性加重期患者报告结局测评工具研究现状[J]. 中国全科医学,2024,27(31):3896-3904. [12] Sunjaya A,Poulos L,Reddel H,et al. Qualitative validation of the modified Medical Research Council (mMRC) dyspnoea scale as a patient-reported measure of breathlessness severity[J]. Respir Med,2022,203:106984. doi: 10.1016/j.rmed.2022.106984 [13] 高露青. 呼吸困难测评工具的研究进展[J]. 现代临床护理,2023,22(10):86-94. doi: 10.3969/j.issn.1671-8283.2023.10.014 [14] 时延伟, 张二明, 郭伟安, 等. CAT评分对慢性阻塞性肺疾病患者病情及疗效的评估价值[J]. 基层医学论坛,2021,25(2):152-155. [15] 倪莺媛,李莎莎,刘晓静,等. 老年人功能能力测评工具研究进展[J]. 护理研究,2023,37(4):655-659. [16] 中华医学会,中华医学会杂志社,中华医学会全科医学分会,等. 中国慢性阻塞性肺疾病基层诊疗与管理指南(2024年)[J]. 中华全科医师杂志,2024,23:793-812. [17] 梁振宇,王凤燕,陈子正,等. 2023年GOLD慢性阻塞性肺疾病诊断、管理及预防全球策略更新要点解读[J]. 中国全科医学,2023,26(11):1287-1298. [18] 张灵,孙程程,蒋水平,等. 主动呼吸循环技术联合常规肺康复运动训练对COPD康复期患者心率变异性和肺功能的影响[J]. 西部医学,2022,34(1):74-78. doi: 10.3969/j.issn.1672-3511.2022.01.014 [19] 党辉,陈军,杨菲菲,等. ACBT联合HRR对稳定期COPD肺功能及运动能力的影响[J]. 中华肺部疾病杂志(电子版),2023,16(5):667-669. [20] 魏玮,白海鹏,甄静. ACBT方案联合渐进弹力抗阻运动对老年肌少症合并慢性阻塞性肺疾病患者肺功能、动脉血气及运动耐力的影响[J]. 检验医学与临床,2024,21(12):1801-1805+1810. doi: 10.3969/j.issn.1672-9455.2024.12.026 [21] 周兆斌,郭帅,黄璐璐,等. 主动呼吸循环技术对老年肺部手术患者肺功能和血清细胞因子水平的影响[J]. 中国老年学杂志,2023,43(19):4680-4683. doi: 10.3969/j.issn.1005-9202.2023.19.021 [22] 江尚燕,韩江英,王云云,等. 辅助缩唇呼吸训练工具在慢性阻塞性肺疾病患者居家肺功能康复中的设计及应用[J]. 中国康复医学杂志,2024,39(6):821-827. doi: 10.3969/j.issn.1001-1242.2024.06.009 [23] 高志君,赵珂,代萌,等. 不同自主呼吸训练方法对区域性肺通气影响的对比研究[J]. 中国康复医学杂志,2024,39(5):634-640. doi: 10.3969/j.issn.1001-1242.2024.05.004 [24] 吴琪,季梅丽,张蓉,等. 缩唇腹式呼吸训练联合弹力带抗阻运动对慢性心力衰竭患者运动耐力、心肺功能及生活质量的影响[J]. 现代生物医学进展,2023,23(7):1279-1282+1373. [25] 刘国英,王宇华. 抗阻呼吸训练对慢性阻塞性肺疾病患者肺功能、运动耐力和生活质量的影响[J]. 海南医学,2021,32(20):2634-2637. doi: 10.3969/j.issn.1003-6350.2021.20.013 [26] 王明枫,罗世林,黎必亮,等. 主动循环呼吸训练联合肺功能康复对肺癌术后患者肺功能的影响[J]. 肿瘤预防与治疗,2023,36(7):590-594. doi: 10.3969/j.issn.1674-0904.2023.07.007 -





 下载:
下载: