|
[1]
|
Yoshii S R,Mizushima N. Autophagy machinery in the context of mammalian mitophagy[J]. Biochimica et Biophysica Acta (BBA) - Molecular Cell Research,2015,1853(10):2797-2801. doi: 10.1016/j.bbamcr.2015.01.013
|
|
[2]
|
Gan Z Y,Komander D,Callegari S. Reassessing kinetin’ s effect on PINK1 and mitophagy[J]. Autophagy,2024,20(11):2596-2597. doi: 10.1080/15548627.2024.2395144
|
|
[3]
|
Lu X Y,Zhu L Y,Zhu H,et al. Cyclometalated iridium(III)-lonidamine conjugates: Mitochondrial targeting and pyroptosis induction[J]. Journal of Inorganic Biochemistry,2025,266:112852. doi: 10.1016/j.jinorgbio.2025.112852
|
|
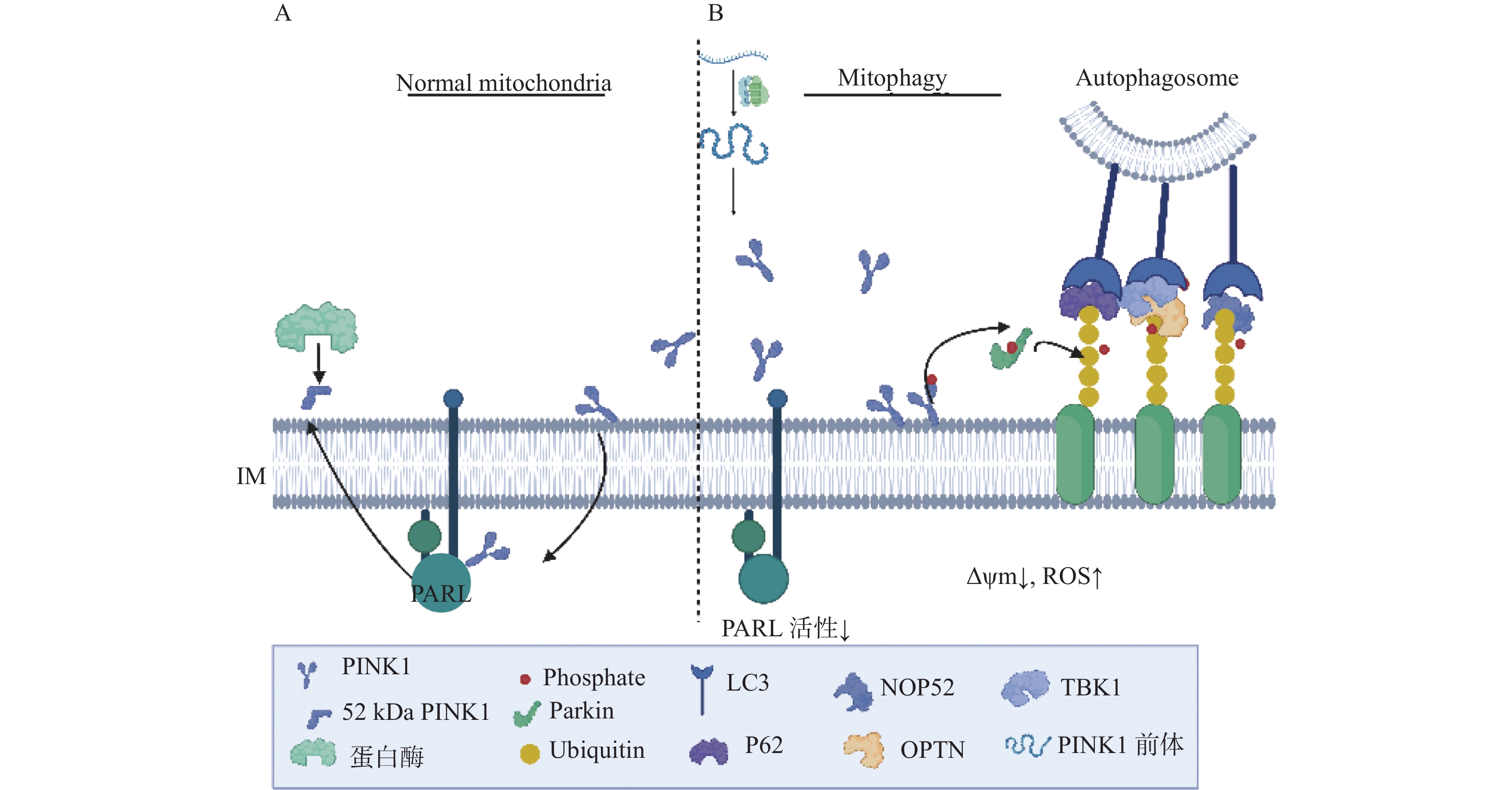
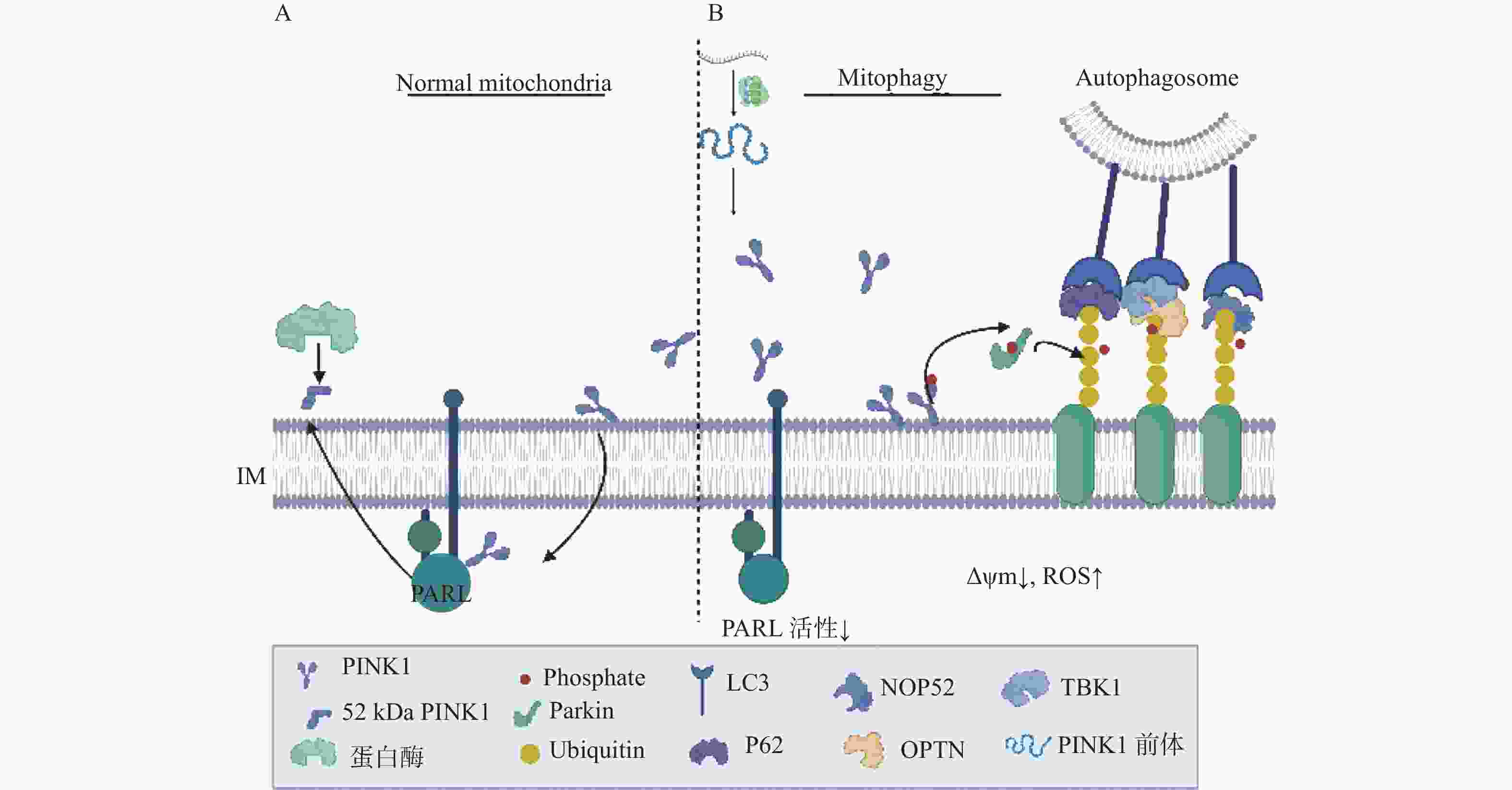
[4]
|
Zarkovic N. Roles and functions of ROS and RNS in cellular physiology and pathology[J]. Cells,2020,9(3):767. doi: 10.3390/cells9030767
|
|
[5]
|
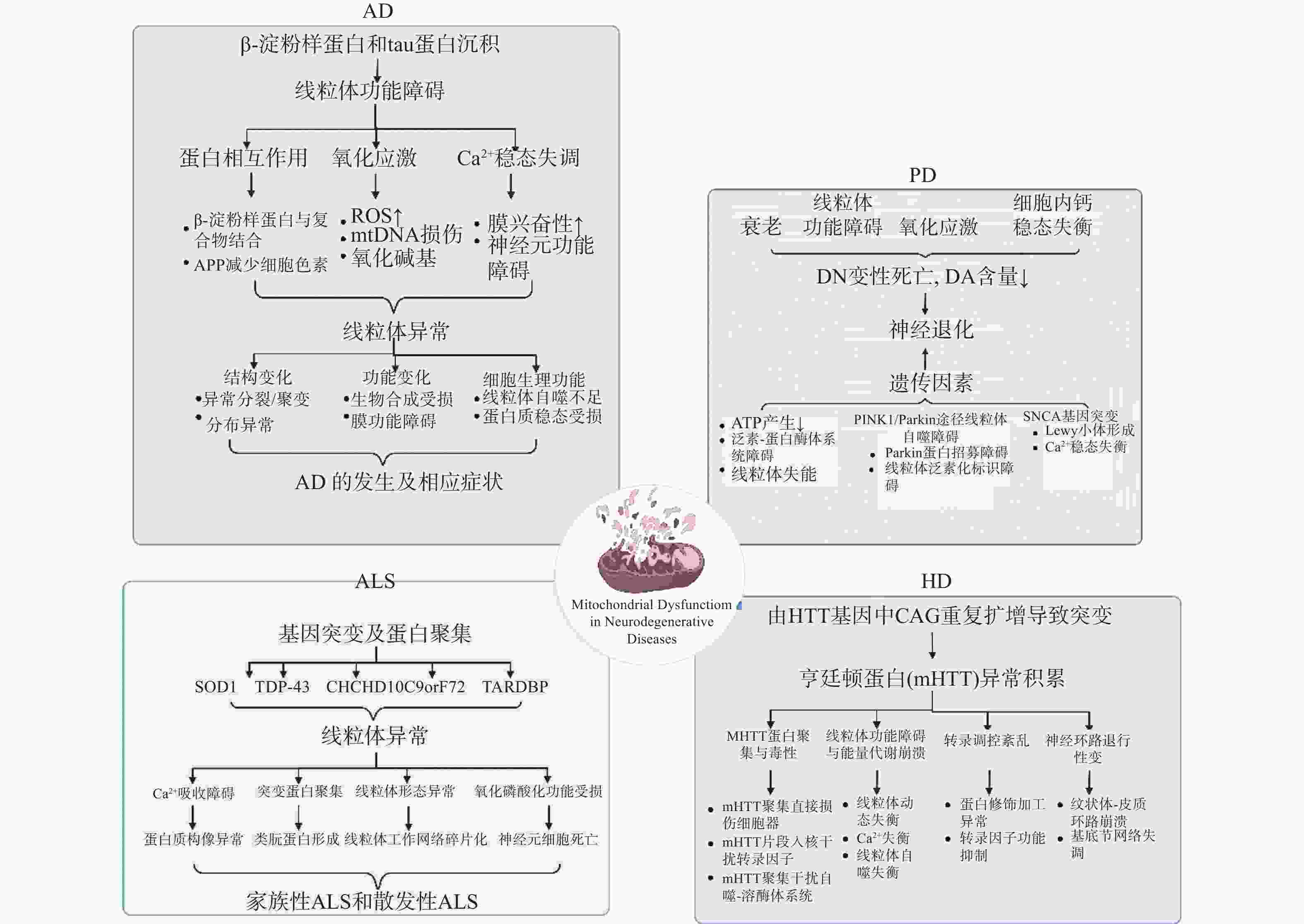
Li Y,Zhang W,Zhang Q,et al. Oxidative stress of mitophagy in neurodegenerative diseases: Mechanism and potential therapeutic targets[J]. Archives of Biochemistry and Biophysics,2025,764:110283. doi: 10.1016/j.abb.2024.110283
|
|
[6]
|
Burda R,Burda J,Morochovič R. Ischemic tolerance-a way to reduce the extent of ischemia-reperfusion damage[J]. Cells,2023,12(6):884. doi: 10.3390/cells12060884
|
|
[7]
|
Zhu J,Xu N,Lin H,et al. Remote ischemic preconditioning plays a neuroprotective role in cerebral ischemia-reperfusion mice by inhibiting mitophagy[J]. Heliyon,2024,10(20):e39076. doi: 10.1016/j.heliyon.2024.e39076
|
|
[8]
|
Mao Z,Tian L,Liu J,et al. Ligustilide ameliorates hippocampal neuronal injury after cerebral ischemia reperfusion through activating PINK1/Parkin-dependent mitophagy[J]. Phytomedicine,2022,101:154111. doi: 10.1016/j.phymed.2022.154111
|
|
[9]
|
Li X,Guan L,Liu Z,et al. Ubiquitination of ATAD3A by TRIM25 exacerbates cerebral ischemia-reperfusion injury via regulating PINK1/Parkin signaling pathway-mediated mitophagy[J]. Free Radical Biology and Medicine,2024,224:757-769. doi: 10.1016/j.freeradbiomed.2024.09.029
|
|
[10]
|
Xiao B,Cui Y,Li B,et al. ROS antagonizes the protection of Parkin-mediated mitophagy against aluminum-induced liver inflammatory injury in mice[J]. Food and Chemical Toxicology,2022,165:113126. doi: 10.1016/j.fct.2022.113126
|
|
[11]
|
Fan P,Xie X H,Chen C H,et al. Molecular regulation mechanisms and interactions between reactive oxygen species and mitophagy[J]. DNA and Cell Biology,2019,38(1):10-22. doi: 10.1089/dna.2018.4348
|
|
[12]
|
Tang C,He L,Liu J,et al. Mitophagy: Basic mechanism and potential role in kidney diseases[J]. Kidney Diseases,2015,1(1):71-79. doi: 10.1159/000381510
|
|
[13]
|
Wen J,Pan T,Li H,et al. Role of mitophagy in the hallmarks of aging[J]. Journal of Biomedical Research,2022,37(1):1-14.
|
|
[14]
|
Tintos-Hernández J A,Santana A,Keller K N,et al. Lysosomal dysfunction impairs mitochondrial quality control and is associated with neurodegeneration in TBCK encephaloneuronopathy[J]. Brain Communications,2021,3(4):fcab215. doi: 10.1093/braincomms/fcab215
|
|
[15]
|
Tang M,Rong D,Gao X,et al. A positive feedback loop between SMAD3 and PINK1 in regulation of mitophagy[J]. Cell Discovery,2025,11(1):22. doi: 10.1038/s41421-025-00774-4
|
|
[16]
|
Jin S M,Youle R J. PINK1- and Parkin-mediated mitophagy at a glance[J]. Journal of Cell Science,2012,125(4):795-799. doi: 10.1242/jcs.093849
|
|
[17]
|
Cheng J,Wei L,Li M. Progress in regulation of mitochondrial dynamics and mitochondrial autophagy[J]. Sheng Li Xue Bao: (Acta Physiologica Sinica),2020,72(4):475-487.
|
|
[18]
|
Hu T,Wu C,Jian W,et al. Effect of PINK1 and Parkin gene silencing on sodium arsenite-induced mitophagy in normal rat liver cells (BRL-3A)[J]. Toxicology Research,2022,11(1):52-59. doi: 10.1093/toxres/tfab110
|
|
[19]
|
Kanki T,Furukawa K,Yamashita S. Mitophagy in yeast: Molecular mechanisms and physiological role[J]. Biochimica et Biophysica Acta (BBA) - Molecular Cell Research,2015,1853(10):2756-2765. doi: 10.1016/j.bbamcr.2015.01.005
|
|
[20]
|
Wang Y,Shen J,Chen Y,et al. PINK1 protects against oxidative stress induced senescence of human nucleus pulposus cells via regulating mitophagy[J]. Biochemical and Biophysical Research Communications,2018,504(2):406-414. doi: 10.1016/j.bbrc.2018.06.031
|
|
[21]
|
Bowling J L,Skolfield M C,Riley W A,et al. Temporal integration of mitochondrial stress signals by the PINK1: Parkin pathway[J]. BMC Molecular and Cell Biology,2019,20(1):33. doi: 10.1186/s12860-019-0220-5
|
|
[22]
|
Gao J,Qin S,Jiang C. Parkin-induced ubiquitination of Mff promotes its association with p62/SQSTM1 during mitochondrial depolarization[J]. Acta Biochimica et Biophysica Sinica,2015,47(7):522-529. doi: 10.1093/abbs/gmv044
|
|
[23]
|
Jayatunga D P W,Hone E,Bharadwaj P,et al. Targeting mitophagy in Alzheimer’ s disease[J]. Journal of Alzheimer’ s Disease,2020,78(4):1273-1297. doi: 10.3233/JAD-191258
|
|
[24]
|
Ashok B S,Ajith T A,Sivanesan S. Hypoxia-inducible factors as neuroprotective agent in Alzheimer’ s disease[J]. Clinical and Experimental Pharmacology and Physiology,2017,44(3):327-334. doi: 10.1111/1440-1681.12717
|
|
[25]
|
Hassan W,Noreen H,Rehman S,et al. Association of oxidative stress with neurological disorders[J]. Current Neuropharmacology,2022,20(6):1046-1072. doi: 10.2174/1570159X19666211111141246
|
|
[26]
|
George A J,Gordon L,Beissbarth T,et al. A serial analysis of gene expression profile of the Alzheimer’ s disease Tg2576 mouse model[J]. Neurotoxicity Research,2010,17(4):360-379. doi: 10.1007/s12640-009-9112-3
|
|
[27]
|
Mart í n-Maestro P,Gargini R,Garc í a E,et al. Mitophagy failure in APP and tau overexpression model of Alzheimer’ s disease[J]. Journal of Alzheimer’ s Disease,2019,70(2):525-540. doi: 10.3233/JAD-190086
|
|
[28]
|
Zeng K,Yu X,Mahaman Y A R,et al. Defective mitophagy and the etiopathogenesis of Alzheimer’ s disease[J]. Translational Neurodegeneration,2022,11(1):32. doi: 10.1186/s40035-022-00305-1
|
|
[29]
|
Quinn P M J,Moreira P I,Ambrósio A F,et al. PINK1/PARKIN signalling in neurodegeneration and neuroinflammation[J]. Acta Neuropathologica Communications,2020,8(1):189. doi: 10.1186/s40478-020-01062-w
|
|
[30]
|
Du F,Yu Q,Yan S S. PINK1 activation attenuates impaired neuronal-like differentiation and synaptogenesis and mitochondrial dysfunction in Alzheimer’ s disease trans-mitochondrial cybrid cells[J]. Journal of Alzheimer’ s Disease,2021,81(4):1749-1761. doi: 10.3233/JAD-210095
|
|
[31]
|
Wang X juan,Qi L,Cheng Y fang,et al. PINK1 overexpression prevents forskolin-induced tau hyperphosphorylation and oxidative stress in a rat model of Alzheimer’ s disease[J]. Acta Pharmacologica Sinica,2022,43(8):1916-1927. doi: 10.1038/s41401-021-00810-5
|
|
[32]
|
Dhapola R,Kumari S,Sharma P,et al. Advancements in autophagy perturbations in Alzheimer’ s disease: Molecular aspects and therapeutics[J]. Brain Research,2025,1851:149494. doi: 10.1016/j.brainres.2025.149494
|
|
[33]
|
Tarakad A,Jankovic J. Recent advances in understanding and treatment of Parkinson’ s disease[J]. Faculty Reviews,2020,9:6.
|
|
[34]
|
Rango M,Dossi G,Squarcina L,et al. Brain mitochondrial impairment in early-onset Parkinson’ s disease with or without PINK1 mutation[J]. Movement Disorders,2020,35(3):504-507. doi: 10.1002/mds.27946
|
|
[35]
|
Kazlauskaite A,Muqit M M K. PINK1 and Parkin – mitochondrial interplay between phosphorylation and ubiquitylation in Parkinson’ s disease[J]. The FEBS Journal,2015,282(2):215-223. doi: 10.1111/febs.13127
|
|
[36]
|
Li M X,Mu D Z. Mitophagy and nervous system disease[J]. Zhongguo Dang Dai Er Ke Za Zhi = Chinese Journal of Contemporary Pediatrics,2017,19(6):724-729.
|
|
[37]
|
沈金峰,胡芳,王福珍,等. 大蒜素调控PINK1/Parkin介导的线粒体自噬改善大鼠尿毒症心肌损伤[J]. 广州中医药大学学报,2025,2(42):448-454.
|
|
[38]
|
Rogers R S,Tungtur S,Tanaka T,et al. Impaired mitophagy plays a role in denervation of neuromuscular junctions in ALS mice[J]. Frontiers in Neuroscience,2017,11:473. doi: 10.3389/fnins.2017.00473
|
|
[39]
|
Granatiero V,Manfredi G. Mitochondrial transport and turnover in the pathogenesis of amyotrophic lateral sclerosis[J]. Biology,2019,8(2):36. doi: 10.3390/biology8020036
|
|
[40]
|
Zhang H,Gao C,Yang D,et al. Urolithin a improves motor dysfunction induced by copper exposure in SOD1G93A transgenic mice via activation of mitophagy[J]. Molecular Neurobiology,2024,62(6):6922-6937
|
|
[41]
|
Gatto E M,Rojas N G,Persi G,et al. Huntington disease: Advances in the understanding of its mechanisms[J]. Clinical Parkinsonism & Related Disorders,2020,3:100056.
|
|
[42]
|
Liu T,Wetzel L,Zhu Z,et al. Disruption of mitophagy flux through the PARL-PINK1 pathway by CHCHD10 mutations or CHCHD10 depletion[J]. Cells,2023,12(24):2781. doi: 10.3390/cells12242781
|
|
[43]
|
Joshi D C,Chavan M B,Gurow K,et al. The role of mitochondrial dysfunction in Huntington’ s disease: Implications for therapeutic targeting[J]. Biomedicine & Pharmacotherapy,2025,183:117827.
|
|
[44]
|
Khalil B,El Fissi N,Aouane A,et al. PINK1-induced mitophagy promotes neuroprotection in Huntington’ s disease[J]. Cell Death & Disease,2015,6(1):e1617.
|
|
[45]
|
Liang Z,Zhao S,Liu Y,et al. The promise of mitochondria in the treatment of glioblastoma: A brief review[J]. Discover Oncology,2025,16(1):142. doi: 10.1007/s12672-025-01891-y
|
|
[46]
|
Yao N,Wang C,Hu N,et al. Inhibition of PINK1/Parkin-dependent mitophagy sensitizes multidrug-resistant cancer cells to B5G1,a new betulinic acid analog[J]. Cell Death & Disease,2019,10(3):232.
|





 下载:
下载: