Epidemiological Characteristics of Respiratory Virus Infections in Kunming Region during 2023-2024
-
摘要:
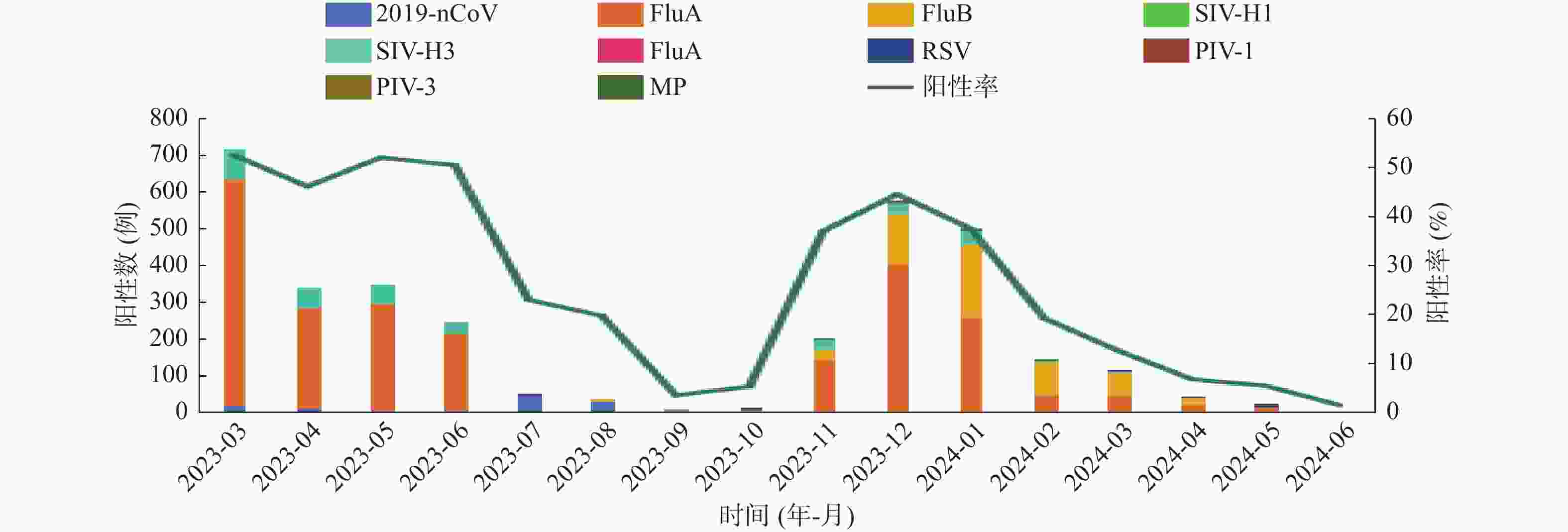
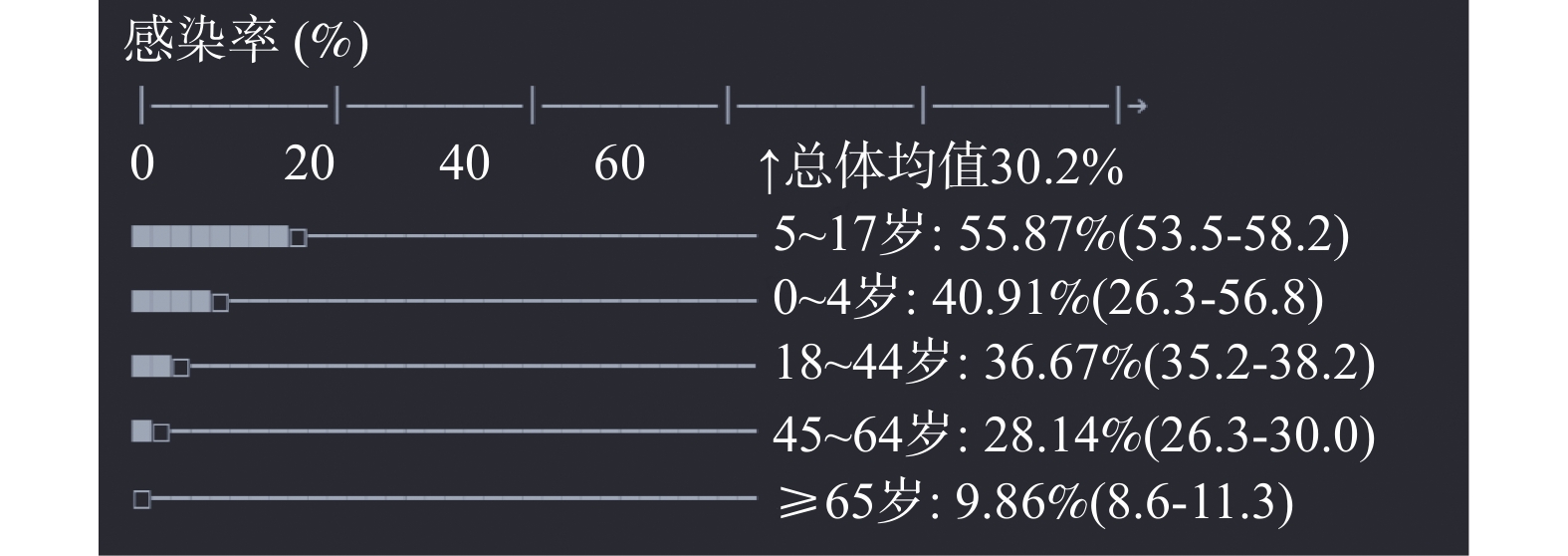
目的 分析2023—2024年昆明地区呼吸道病毒感染的流行病学特征,探讨不同病毒种类的检出率及其在不同时间段和不同年龄层的分布变化规律。 方法 回顾性收集2023年3月至2024年6月期间,因急性呼吸道感染至昆明市第三人民医院就诊的患者的鼻咽拭子或痰液样本共计 10354 例。通过实时荧光定量聚合酶链反应(real-time fluorescent quantitative polymerase chain reaction,RT-qPCR)技术,对样本中的多种病原体进行检测。随后,对临床实验室的检测结果进行了回顾性分析,统计各类呼吸道病毒的整体检出率、多重感染现象、性别差异、年龄分布、季节性变化、感染部位差异以及不同月份的感染情况。结果 在检测 10354 例患者的呼吸道样本中,检出病原体感染3368 例,检出率为32.53%(3368 /10354 )。有204例患者呈现≥2种病原体的混合感染,混合检出率为(6.06%,204/3368 )。女性单一检出率显著高于男性(P < 0.001),男性多重检出率显著高于女性(P < 0.05),提示男性合并感染风险可能更高。在不同年龄组的比较中,5~18岁组的病毒检出率最高为55.87%。FluA、FluB及SIV-H3在不同疾病类型的呼吸道病毒检出率中存在显著差异(P < 0.05)。2023年3月位居首位,检出率为(54.27%,5619 /10354 ),其中甲型流感病毒(FluA)和季节性流感病毒H3亚型(SIV-H3)为检出率最高的病原体。结论 昆明地区急性呼吸道感染(ARI)病例中感染的病毒以FluA、FluB和SIV-H3为主要病原体,该地区病毒流行特征与患者年龄阶段、季节变化以及感染部位等因素紧密相关。 -
关键词:
- 呼吸道感染 /
- 病毒 /
- 流行病学特征 /
- 实时荧光定量 PCR
Abstract:Objective Analyze the epidemiological characteristics of respiratory virus infections in Kunming area during 2023-2024, and explore the detection rates of different virus types and their distribution patterns across different time periods and age groups. Methods A total of 10354 nasopharyngeal swab or sputum samples were retrospectively collected from patients with acute respiratory infections who visited the Third People's Hospital of Kunming City between March 2023 and June 2024. Multiple pathogens were detected using real-time fluorescent quantitative polymerase chain reaction (RT-qPCR) technology. A retrospective analysis was then conducted on the clinical laboratory detection results, statistically analyzing the overall detection rates of various respiratory viruses, multiple infection phenomena, gender differences, age distribution, seasonal variations, infection site differences, and monthly infection situations.Results Among the 10354 patient respiratory samples tested,3368 pathogen infections were detected, with a detection rate of 32.53% (3368 /10354 ). 204 patients presented with mixed infections of ≥2 pathogens, with a mixed detection rate of 6.06%(204/3368 ). The single detection rate for females was significantly higher than males (P < 0.001), and the multiple infection detection rate for males is significantly higher than females (P < 0.05), indicating that males may have a higher risk of concurrent infections. Among different age groups, the virus detection rate was highest in the 5-18 years age group at 55.87%. Significant differences were observed in the detection rates of FluA, FluB, and SIV-H3 across different disease types (P < 0.05). In March 2023, the detection rate was highest at 54.27% (5619 /10354 ), with Influenza A virus (FluA) and seasonal influenza H3 subtype (SIV-H3) being the most detected pathogens.Conclusion In acute respiratory infection (ARI) cases in the Kunming area, FluA, FluB, and SIV-H3 were the primary viral pathogens, with the region's viral epidemic characteristics closely related to patient age stages, seasonal changes, and infection site factors. -
表 1 病原体总检出状况
Table 1. Pathogen detection overall status
病原体 检出例数(n) 检出率(%) 2019-nCoV 131 1.27 FluA 2324 22.45 FluB 548 5.29 SIV-H1 17 0.16 SIV-H3 266 2.57 Adv 13 0.13 RSV 13 0.13 PIV-1 5 0.05 PIV-3 28 0.27 MP 23 0.22 合计 3368 32.53 表 2 病原体混合感染检出情况
Table 2. Detection of mixed pathogen infections
混合病原体 检出例数(n) 检出率(%) 2019-nCoV+FluA 6 0.18 FluA+FluB 4 0.12 FluA+SIV-H1 6 0.18 FluA+SIV-H3 175 5.20 SIV-H1+SIV-H3 6 0.18 Adv+PIV-3 1 0.03 FluA+SIV-H1+SIV-H3 6 0.18 合计 204 6.06 表 3 不同性别病原体检出率[n(%)]
Table 3. Pathogen detection rates by gender [n (%)]
性别 n 病原体感染 单一病原体感染 ≥2种病原体感染 男 5685 1838(32.33) 1721 (30.27 )117(2.06) 女 4669 1530 (32.77 )1443 (30.91 )87(1.86) χ2 0.225 0.485 0.503 P 0.635 0.486 0.478 表 4 不同年龄病原体检出率[n(%)]
Table 4. Pathogen detection rates by different age groups [n (%)]
年龄组(岁) n 病原体感染 单一病原体感染 ≥2种病原体感染 0~ 44 18(40.91) 7(15.91) 11(25.00 ) 5~ 1754 980(55.87) 882(50.29)# 98(5.59) 18~ 3993 1464 (36.67)1407 (35.24)△57(1.43) 45~ 2495 702(28.14) 677(27.13) 25(1.00) ≥65 2068 204(9.86 ) 191(9.23)▲ 13(0.63) χ2 2033.485 1975.747 133.451 P <0.001* <0.001* <0.001* 趋势检验χ2 1142.6 985.3 158.2 趋势检验P <0.001* 0.001* 0.001* 0~5岁组与5~18岁组比较,#P < 0.001;5~18岁组与18~45岁组比较,△P < 0.01;45~65岁组与 ≥65岁组比较,▲P < 0.001;*P < 0.05。 表 5 不同季节病原体检出情况[n(%)]
Table 5. Pathogen detection in different seasons [n (%)]
季节 n 病原体阳性
例数(n)2019-nCoV FluA FluB SIV-H1 SIV-H3 Adv RSV PIV-1 PIV-3 MP 春季
(3~5)3265 1228 (37.61)53(1.62) 925(28.33) 45(1.38) 7(0.21) 213(6.52) 0(0) 0(0) 0(0) 0(0) 0(0) 夏季
(6~8)600 87(14.50) 24(4.00) 98(16.33) 11(1.83) 8(1.33) 1(0.17) 0(0) 1(0.17) 0(0 ) 0(0 ) 0(0) 秋季
(9~11)3396 1089 (32.07)43(1.27) 882(25.97) 316(9.31) 0(0) 47(1.38) 5(0.15) 10(0.29) 3(0.10) 15(0.44) 18(0.53) 冬季
(12~2)3093 964(31.17) 11(0.36) 419(13.55) 176(5.69) 2(0.06) 5(0.16) 8(0.26) 2(0.06) 2(0.06) 13(0.42) 5(0.16) χ2 944.078 32.511 806.317 422.642 - 449.850 - - - - - P <0.001* <0.001* <0.001* <0.001* 0.169 <0.001* 0.581 0.005* 1.000 0.851 0.011* *P < 0.05。 表 6 季节性病原体分布特征总结
Table 6. Summary of seasonal pathogen distribution characteristics
季节 总检测量 主要病原体分布(前三位) 春季(3~5月) 3265 FluA(28.33)>SIV-H3(6.52)>2019-nCoV(1.62) 夏季(6~8月) 600 FluA(16.33)> 2019-nCoV(4.00)>FluB(1.83) 秋季(9~11月) 3396 FluA(25.97)>FluB(9.31)>SIV-H3(1.38) 冬季(12~2月) 3093 FluA(13.55)>FluB(5.69)> PIV-3(0.42) 表 7 呼吸道病毒季节性(检出率%)
Table 7. Respiratory virus seasonal heatmap (data format: detection rate%)
病毒类型 春季(3~5月) 夏季(6~8月) 秋季(9~11月) 冬季(12~2月) 当前季节提示 FluA 28.33 16.33 25.97 13.55 ● 2025年4月高发预警FluB 1.38 1.83 9.31 5.69 ● 秋季需加强监测2019-nCoV 1.62 4.00 1.27 0.36 ● 夏季反弹风险RSV 0 0.17 0.29 0.06 ● 低水平流行MP 0 0 0.53 0.16 ● 秋季儿科重点关注表 8 不同感染部位病原体检出状况[n(%)]
Table 8. Pathogen detection status in different infection sites [n (%)]
感染部位 n 病原体
阳性例数2019-nCoV FluA FluB SIV-H1 SIV-H3 Adv RSV PIV-1 PIV-3 MP 上呼
吸道6594 2126 (32.24)101(1.53) 1665 (25.25)391(5.93) 12(0.18) 168(2.55) 9(0.14) 8(0.12) 3(0.04) 17(0.26) 19(0.29) 下呼
吸道3760 1242 (33.03)30(0.80) 659(17.53) 157(4.18) 5(0.13) 98(2.61) 4(0.11) 5(0.13) 2(0.05) 11(0.29) 4(0.11) χ2 232.024 38.481 435.472 99.920 - 18.421 - - - - - P <0.001* <0.001* <0.001* <0.001* 0.143 <0.001* 0.267 0.581 1.000 0.345 0.003* *P < 0.05。 -
[1] Heinonen S, Jartti T, Garcia C, et al. Rhinovirus detection in symptomatic and asymptomatic children: Value of host transcriptome analysis[J]. Am J Respir Crit Care Med, 2016, 193(7): 772-782. doi: 10.1164/rccm.201504-0749OC [2] Zhang N, Wang L, Deng X, et al. Recent advances in the detection of respiratory virus infection in humans[J]. J Med Virol, 2020, 92(4): 408-417. doi: 10.1002/jmv.25674 [3] World Health Organization. The top 10 causes of death[EB/OL]. (2020-12-09)[2021-08-26]. https://www.who.int/news-room/factsheets/detail/the-top-10-causes-of-death. [4] Milinovich G J, Williams G M, Clements A C, et al. Internet-based surveillance systems for monitoring emerging infectious diseases[J]. Lancet Infect Dis, 2014, 14(2): 160-168. doi: 10.1016/S1473-3099(13)70244-5 [5] Islam M A, Hasan M N, Ahammed T, et al. Association of household fuel with acute respiratory infection under-five years children in Bangladesh[J]. Front Public Health, 2022, 10(4): 985445. [6] Kalil A C, Metersky M L, Klompas M, et al. Management of adults with hospital-acquired and ventilator- associated pneumonia: 2016 clinical practice guidelines by the infectious diseases Society of America and the American Thoracic Society[J]. Clin Infect Dis, 2016, 63(5): e61-e111. doi: 10.1093/cid/ciw353 [7] Abed Y, Boivin G. Treatment of respiratory virus infections[J]. Antiviral Res, 2006, 70(2): 1-16. doi: 10.1016/j.antiviral.2006.01.006 [8] Gandhi L, Maisnam D, Rathore D, et al. Respiratory illness virus infections with special emphasis on COVID-19[J]. Eur J Med Res, 2022, 27(1): 236. doi: 10.1186/s40001-022-00874-x [9] Grief S N. Upper respiratory infections[J]. Prim Care, 2013, 40(3): 757-770. doi: 10.1016/j.pop.2013.06.004 [10] Walter J M, Wunderink R G. Testing for respiratory viruses in adults with severe lower respiratory infection[J]. Chest, 2018, 154(5): 1213-1222. doi: 10.1016/j.chest.2018.06.003 [11] 中国疾病预防控制局. 2021年全国法定传染病疫情概况 [EB/OL]. (2022-12-03)[2022-08-11]. http://www.nhc.gov.cn/jkj/s3578/202204/4fd88a291d914abf8f7a91f6333567e1.shtml. [12] 宋晓岩. 防止常见季节性呼吸道病毒疾病在医院内传播的措施[J]. 中国感染控制杂志, 2023, 22(9): 999-1002. doi: 10.12138/j.issn.1671-9638.20233815 [13] 张煜轩, 瞿介明. 呼吸感染性疾病诊治年度进展2024[J]. 中华结核和呼吸杂志, 2025, 48(2): 149-153. doi: 10.3760/cma.j.cn112147-20241218-00744 [14] 魏柯雯, 马仲慧, 龚成, 等. 2015-2019年北京市房山区哨点医院急性呼吸道感染疾病流行特征及影响因素分析[J]. 预防医学情报杂志, 2022, 38(1): 35-39+44. doi: 10.3969/j.issn.1006-4028.2022.1.yfyxqbzz202201008 [15] 王中浩, 杨岚, 吴思颖, 等. 2017-2023年四川省呼吸道病毒感染的流行病学特征分析[J]. 中华微生物学和免疫学杂志, 2024, 44(7): 573-579. [16] 王紫怡, 翁坚, 王红珠, 等. 2020-2021年浙江省台州市急性呼吸道感染病原学研究[J]. 上海预防医学, 2022, 34(7): 638-641+649. [17] Xu B, Wang J F, Li Z J, et al. Seasonal association between viral causes of hospitalised acute lower respiratory infections and meteorological factors in China: A retrospective study[ J]. Lancet Planet Health, 2021, 5(3): e154-e163. [18] Sato M, Takashita E, Katayose M, et al. Clinical and virologic impacts of respiratory viral co-infections in children with influenza[J]. Pediatr Infect Dis J, 2023, 42(8): e268-e273. doi: 10.1097/INF.0000000000003940 [19] 关亚柯, 周正元, 梅国勇, 等. 2022-2023年常熟市急性呼吸道感染病例常见病毒病原谱系分析[J]. 中华实验和临床病毒学杂志, 2024, 38(3): 252-257. [20] 周丽敏, 王希峰, 郑天驰, 等. 2015年-2021年北京市大兴区严重急性呼吸道感染病例流感病毒检测结果分析[J]. 中国卫生检验杂志, 2022, 32(14): 1718-1721. [21] 季路, 陶芳芳, 王琳, 等. 2019-2021年上海市杨浦区成人严重急性呼吸道感染住院病例病原学特征分析[J]. 上海预防医学, 2022, 34(8): 774-779. [22] Taylor S, Lopez P, Weckx L, et al. Respiratory viruses and influenza‑like illness: Epidemiology and outcomes in children aged 6 months to 10 years in a multi‑country population sample[J]. J Infect, 2017, 74(1): 29-41. doi: 10.1016/j.jinf.2016.09.003 -






 下载:
下载: