Analysis of Oral Microbial Community Structure in Schizophrenia Patients in Baoshan City
-
摘要:
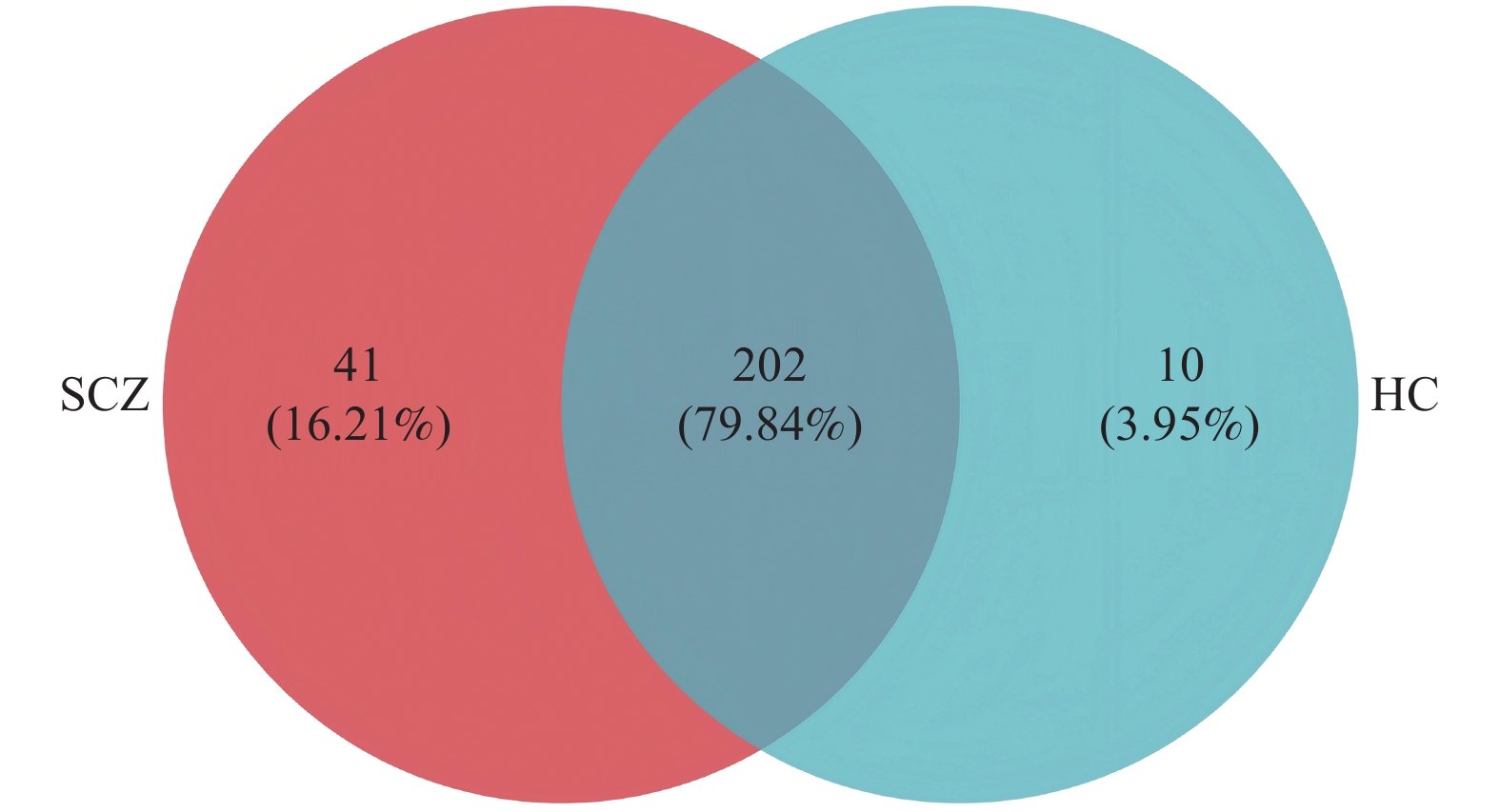
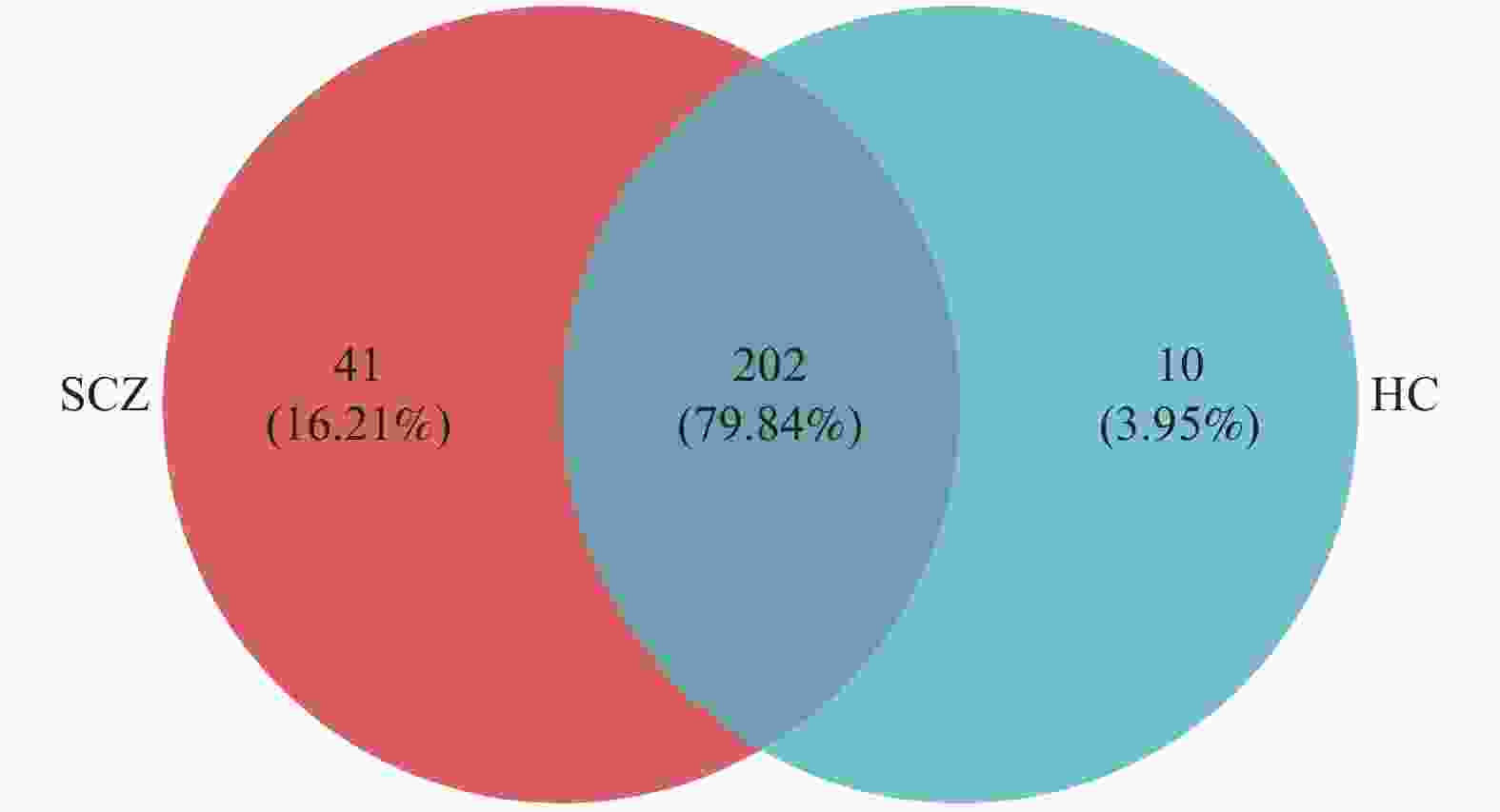
目的 分析保山市精神分裂症患者和健康人之间口腔卫生及口腔微生物间的差异。 方法 选择保山市第三人民医院26名精神分裂症患者作为病例组,按年龄、体质指数匹配的26名健康人作为健康对照组,收集人口学资料、体格指标及口腔状况,采集52名研究对象唾液样本并采用16S rDNA基因测序分析,比较精神分裂症患者和健康人之间口腔卫生及口腔微生物间的差异。 结果 病例组和健康对照组的口腔微生物群落丰富度差异具有统计学意义(P < 0.05),病例组所含物种种类高于健康对照组;属水平上,除病例组的Fusobacterium和健康对照组的Actinomyces,两组排名前5的优势菌种一致;物种差异分析结果显示在病例组中Fusobacterium和Campylobacter均高于健康对照组(P < 0.05)。 结论 精神分裂症患者口腔的部分优势菌种向产生硫化氢的硫酸盐还原菌属转变,过量的硫化氢或多硫化物的产生可能会损害线粒体的能量代谢。 Abstract:Objective To analyze the differences in oral hygiene and oral microbiota between the patients with schizophrenia and healthy individuals in Baoshan City. Methods 26 patients with schizophrenia from Baoshan Third People's Hospital were selected as the SCZ group and 26 healthy individuals matched by age and BMI as the HC (Healthy control) group. Demographic data, physical indicators, and oral conditions were collected. Saliva samples from 52 subjects were collected and 16S rDNA gene sequencing was used to compare the differences in oral hygiene and oral microbiota between the patients with schizophrenia and the healthy individuals. Results The difference in oral microbial community richness between the SCZ group and the HC group was statistically significant (P < 0.05), with the SCZ group containing higher species than the HC group; at the genus level, except for Fusobacterium in the SCZ group and Actinomyces in the HC group, the top 5 dominant bacterial species in both groups were consistent; the results of species difference analysis showed that Fusobacterium and Campylobacter in the SCZ group were higher than those in the HC group (P < 0.05). Conclusion The partial dominant bacterial species in the oral cavity of the patients with schizophrenia have changed to sulfate-reducing bacteria that produce hydrogen sulfide. Excessive production of hydrogen sulfide or polysulfide may damage the energy metabolism of mitochondria. -
Key words:
- Oral microbiota /
- Schizophrenia /
- Oral hygiene
-
表 1 研究对象一般资料及口腔卫生状况对比
Table 1. General information of study subjects and comparison of oral hygiene status
变量 SCZ HC χ2/t P 性别(n) 男 10 13 0.702 0.402 女 16 13 文化程度(n) 小学及以下 7 7 1.727 0.422 初中 13 9 高中及以上 6 10 刷牙是否会牙龈出血(n) 很少或不出血 16 20 1.444 0.229 有时或经常出血 10 6 婚姻状况(n) 已婚 6 20 15.077 <0.001* 其他 20 6 口腔卫生状况得分 1.42 ± 0.90 0.54 ± 0.65 4.063 <0.001* 和HC组相比,*P<0.05。 表 2 SCZ与HC人群唾液菌群的Alpha多样性指数比较
Table 2. Alpha diversity index comparison of oral microbiota between schizophrenia patients and healthy control
指数 HC SCZ P ace 389.27 ± 73.099 427.76 ± 72.398 0.101 chao 386.35 ± 72.254 424.91 ± 68.711 0.071 shannon 3.463 ± 0.333 3.645 ± 0.406 0.098 simpson 0.071 ± 0.023 0.074 ± 0.032 0.876 sobs 334.12 ± 60.165 376.69 ± 65.685 0.047* 和HC组相比,*P < 0.05。 -
[1] 侯明如, 王军, 薛建华, 等. 精神分裂症患者再入院危险因素分析与风险预测模型构建[J]. 现代预防医学, 2024, 51(5): 797-802+835. [2] 谢国念, 李艳红, 李明亮. 精神分裂症糖脂代谢紊乱与睡眠障碍关系的研究进展[J]. 神经疾病与精神卫生, 2024, 24(2): 133-139. doi: 10.3969/j.issn.1009-6574.2024.02.010 [3] 蒋明珠, 丁志山. 精神分裂症诊断相关血清标志物研究进展[J]. 心理月刊, 2025, 20(3): 237-240. [4] 熊雨婷, 潘已汇, 兰红, 等. 口腔微生物组的致病机制及影响因素研究进展[J]. 同济大学学报(医学版), 2025, 46(1): 125-131. [5] 钱泉, 刘银辉. 口腔微生物在牙周健康中的作用研究进展[J]. 中国微生态学杂志, 2025, 37(2): 228-232+239. [6] Wirginia K, Paulina K, Beata B, et al. The association of the oral microbiota with the effects of acid stress induced by an increase of brain lactate in schizophrenia patients[J]. Biomedicines, 2023, 11(2): 240. doi: 10.3390/biomedicines11020240 [7] Jakleen J L, Enrica P, Sabrina T, et al. Gut and oral microbiome modulate molecular and clinical markers of schizophrenia-related symptoms: A transdiagnostic, multilevel pilot study[J]. Psychiatry Research, 2023, 326: 115279. [8] Wang J, Gao B. Mechanisms and potential clinical implications of oral microbiome in oral squamous cell carcinoma[J]. Current Oncology, 2023, 31(1): 168-182. doi: 10.3390/curroncol31010011 [9] 张树伟, 李玉超, 潘亚萍. 口腔微生物及宿主细胞氨基酸代谢与口腔疾病相关性研究进展[J]. 四川大学学报(医学版), 2022, 53(2): 181-187. doi: 10.12182/20220360302 [10] 管晓枫, 胡欣怡, 陆峥. 精神分裂症诊断标准更新与分类变化[J]. 重庆医科大学学报, 2021, 46(7): 760-763. [11] Huang H, Yang N, Chen M M, et al. Altered oral health and microbiota in drug-free patients with schizophrenia[J]. BMC Psychiatry, 2025, 25(1): 274. doi: 10.1186/s12888-025-06633-6 [12] Zongxin L, Yiwen C, Xia L, et al. Altered oral microbiota and immune dysfunction in Chinese elderly patients with schizophrenia: A cross-sectional study[J]. Translational Psychiatry, 2023, 13(1): 383. doi: 10.1038/s41398-023-02682-1 [13] Ying Q, Lihua X, Gaoping C, et al. Salivary microbiome profiling reveals a dysbiotic schizophrenia-associated microbiota[J]. npj Schizophrenia, 2021, 7(1): 51. doi: 10.1038/s41537-021-00180-1 [14] Sasahira M, Matsumoto H, Go T T, et al. The relationship between bacterial flora in saliva and esophageal mucus and endoscopic severity in patients with eosinophilic esophagitis[J]. International Journal of Molecular Sciences, 2025, 26(7): 3026. doi: 10.3390/ijms26073026 [15] 任欢, 乔新, 王峥, 等. 牙龈卟啉单胞菌与阿尔茨海默病相关性致病机制[J]. 微生物学通报, 2024, 51(11): 4359-4369. [16] 李语晨, 刘媛, 陈峰, 等. 口腔菌群与阿尔茨海默症的关系[J]. 四川大学学报(医学版), 2022, 53(2): 194-200. doi: 10.12182/20220360304 [17] 孔金玉, 刘怡文, 钱梦凡, 等. 牙龈卟啉单胞菌感染在食管鳞癌中的作用及机制研究[J]. 安徽医科大学学报, 2024, 59(4): 715-720. [18] 戴柯, 戴周丽, 刘荣场, 等. 牙龈卟啉单胞菌在非酒精性脂肪肝病进展中的作用[J]. 口腔医学, 2024, 44(2): 152-155. [19] Kushkevych I, Coufalová M, Vítězová M, et al. Sulfate-reducing bacteria of the oral cavity and their relation with periodontitis—recent advances[J]. Journal of Clinical Medicine, 2020, 9(8): 2347. doi: 10.3390/jcm9082347 [20] 周桂娟, 唐小卿. 硫化氢在中枢神经系统重大疾病防治中的研究进展[J]. 中国科学: 生命科学, 2023, 53(10): 1397-1423. [21] Song X R, Ma Y X, Zhou T T, et al. Excessive hydrogen sulfide-induced activation of NMDA receptors in the colon participates in anxiety- and compulsive-like behaviors in a rodent model of hemorrhagic shock and resuscitation[J]. International Immunopharmacology, 2024, 142(PB): 113255. [22] Katheron I, Salma G, E RM, et al. A role for endothelial NMDA receptors in the pathophysiology of schizophrenia.[J]. Schizophrenia research, 2020, 249: 63-73. [23] Du X Z, Hu W, Liu M Q, et al. Excess hydrogen sulfide and polysulfides production underlies a schizophrenia pathophysiology[J]. CNS Neuroscience & Therapeutics, 2025, 31(2): e70278. [24] Masayuki I, Tetsuo O, Manabu T, et al. Hydrogen Sulfide Alleviates Schizophrenia- Like Behavior Through Regulating Apoptosis by S-Sulfhydrylation Modification[J]. EMBO molecular medicine, 2019, 11(12): e10695. doi: 10.15252/emmm.201910695 [25] Deepali A, Adarsh K, Manjunath C B, et al. Oral health perception and plight of patients of schizophrenia[J]. International Journal of Dental Hygiene, 2020, 19(1): 121-126. [26] Sun X N, Zhou J B, Li N. Poor Oral Health in Patients with Schizophrenia: A Meta-Analysis of Case-Control Studies[J]. The Psychiatric Quarterly, 2020, 92(prepublish): 1-11. [27] Qin X Y, Pan C Y, Cai Q Q, et al. Assessing the effect of interaction between gut microbiome and inflammatory bowel disease on the risks of depression[J]. Brain, Behavior, & Immunity - Health, 2022, 26: 100557. [28] Button S K , Ioannidis A P J , Mokrysz C , et al. Erratum: Power failure: why small sample size undermines the reliability of neuroscience[J]. Nature Reviews Neuroscience, 2013, 14(6): 451-451. [29] Urien L, Jauregizar N, Lertxundi U, et al. Medication impact on oral health in schizophreni[J]. Medicina Oral, Patologia Oral Y Cirugia Bucal, 2024, 29(1): e51-e57. -





 下载:
下载: