The Prognostic Value of Uterine Artery Blood Flow Combined with Serum Factors for Preeclampsia in Mid-pregnancy
-
摘要:
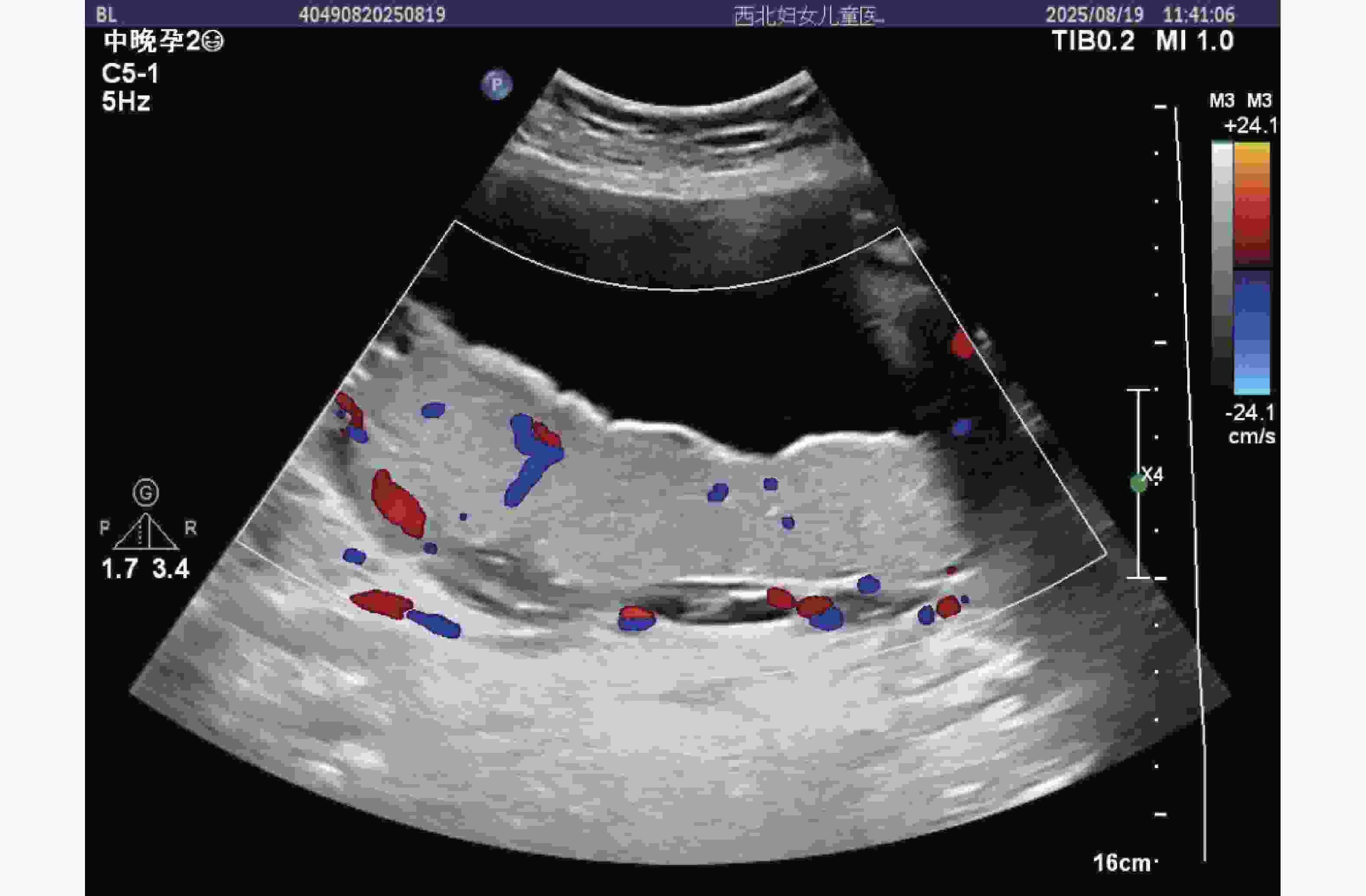
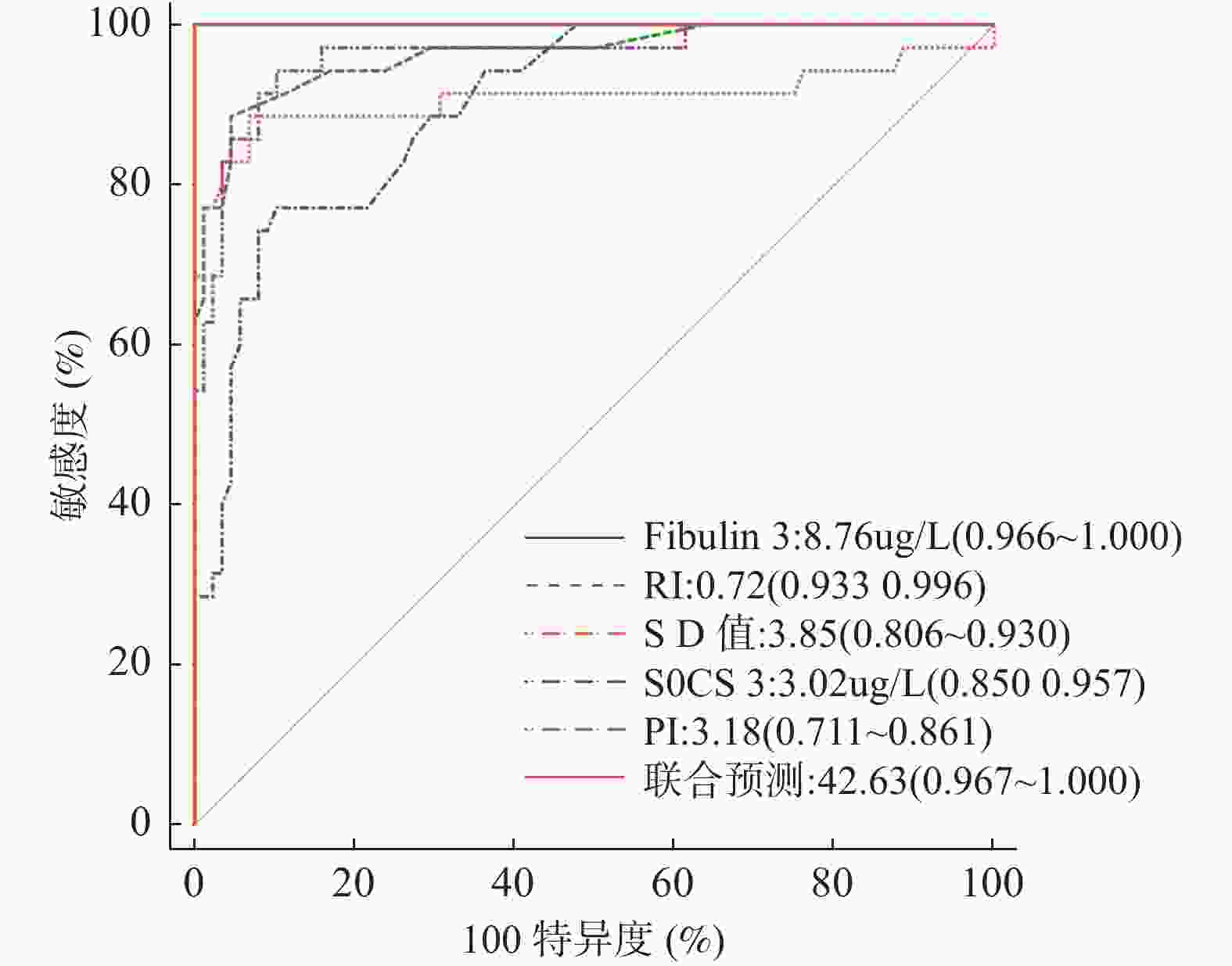
目的 探讨子宫动脉血流多普勒超声联合血清细胞因子信号抑制因子 3(suppressor of cytokine signaling 3,SOCS-3)、纤维蛋白3(Fibulin-3)在孕中期子痫前期孕妇妊娠结局预测中的价值。 方法 采用回顾性分析法,采集西北妇女儿童医院医学超声中心在2022年1月-2024年12月期间接收的123例孕中期子痫前期孕妇作为病例组;另择取105例健康常规检查孕中期孕妇作为正常组,采用彩色多普勒超声检测子宫动脉血流参数,包括搏动指数(pulsatility index,PI)、阻力指数(resistance index,RI)和收缩期峰值流速与舒张末期流速比值(systolic peak velocity to end-diastolic velocity ratio,S/D);运用酶联免疫吸附试验(enzyme-linked immunosorbent assay,ELISA)检测血清 SOCS-3、Fibulin-3 水平。通过统计学分析评估各指标单独及联合检测对子痫前期妊娠结局的预测效能,计算曲线下面积(area under the curve,AUC)、敏感性和特异性。 结果 病例组孕妇子宫动脉血流 PI、RI、S/D 值及 Fibulin-3 水平均高于正常组(P < 0.05),血清 SOCS-3 水平显著低于正常组(P < 0.05)。妊娠中期子痫前期孕妇中,共发生早产 3 例、胎儿生长受限 5 例、胎盘早剥 10 例、子痫 7 例、产后出血 10 例,不良妊娠结局合计 35 例。单因素分析显示,PI、RI、S/D 值及血清 SOCS-3、Fibulin-3 水平均为妊娠不良结局的影响因素(P < 0.05);Logistic 回归分析证实,Fibulin-3 升高、RI 升高、S/D 值升高、SOCS-3降低、PI 升高是不良妊娠结局的独立危险因素(P < 0.05)。构建联合预测模型(回归方程:Fibulin-3×4.767+RI×1.735+S/D 值×2.286-SOCS-3×10.402+PI×1.044),其 ROC 曲线下面积(AUC)为 0.998,特异度 96.59%,敏感度 100.00%,显著优于各单项指标(Fibulin-3 AUC 0.996、RI AUC 0.977、S/D 值 AUC 0.877、SOCS-3 AUC 0.914、PI AUC 0.794,P < 0.05)。 结论 子宫动脉血流参数与血清 SOCS-3、Fibulin-3 水平相结合,能显著提升孕中期子痫前期孕妇不良妊娠结局的预测准确性。 Abstract:Objective To explore the value of uterine artery blood flow Doppler ultrasound combined with serum suppressor of cytokine signaling 3 (SOCS-3) and Fibulin-3 in predicting the pregnancy outcome of preeclampsia pregnant women in the second trimester Method A retrospective analysis method was adopted. The clinical baseline data of 123 pregnant women with preeclampsia in the second trimester who were received by the Medical Ultrasound Center of Northwest Women's and Children's Hospital from January 2022 to December 2024 were collected as the case group. Another 105 pregnant women in the second trimester who underwent routine health examinations were selected as the normal group. The uterine artery blood flow parameters were detected by color Doppler ultrasound. Including the pulsatility index (PI) and the resistance index RI and the ratio of systolic peak velocity to end-diastolic velocity (S/D); The levels of serum SOCS-3 and Fibulin-3 were detected by enzyme-linked immunosorbent assay (ELISA). the predictive efficacy of individual and combined detection of each index for the pregnancy outcome of preeclampsia was evaluated through statistical analysis, and the area under the curve (AUC), sensitivity and specificity were calculated. Result The PI, RI, S/D values of uterine artery blood flow and the level of Fibulin-3 in the case group of pregnant women were all higher than those in the normal group (P < 0.05), while the level of serum SOCS-3 was significantly lower than that in the normal group (P < 0.05). Among pregnant women with preeclampsia in the second trimester of pregnancy, there were 3 cases of premature birth, 5 cases of fetal growth restriction, 10 cases of placental abruption, 7 cases of eclampsia, 10 cases of postpartum hemorrhage, and a total of 35 cases of adverse pregnancy outcomes. Univariate analysis showed that PI, RI, S/D values and serum levels of SOCS-3 and Fibulin-3 were all influencing factors of adverse pregnancy outcomes (P < 0.05); Logistic regression analysis confirmed that Fibulin-3, RI, S/D value, decreased SOCS-3, and elevated PI were independent risk factors for adverse pregnancy outcomes (P < 0.05). Construct a joint prediction model (regression equation:) (Fibulin-3×4.767+RI×1.735+S/D value ×2.286-SOCS-3×10.402+PI×1.044), the area under the ROC curve (AUC) was 0.998, the specificity was 96.59%, and the sensitivity was 100.00% It was significantly superior to each individual indicator (Fibulin-3 AUC 0.996, RI AUC 0.977, S/D value AUC 0.877, SOCS-3 AUC 0.914, PI AUC 0.794, P < 0.05). Conclusion The combination of uterine artery blood flow parameters and the levels of SOCS-3 and Fibulin-3 in serum has a predictive value that significantly exceeds the limitations of a single indicator, greatly improving the accuracy of predicting adverse pregnancy outcomes in pregnant women with preeclampsia. It provides a new evaluation method for the early prediction of pregnancy outcomes in pregnant women with preeclampsia in the second trimester. -
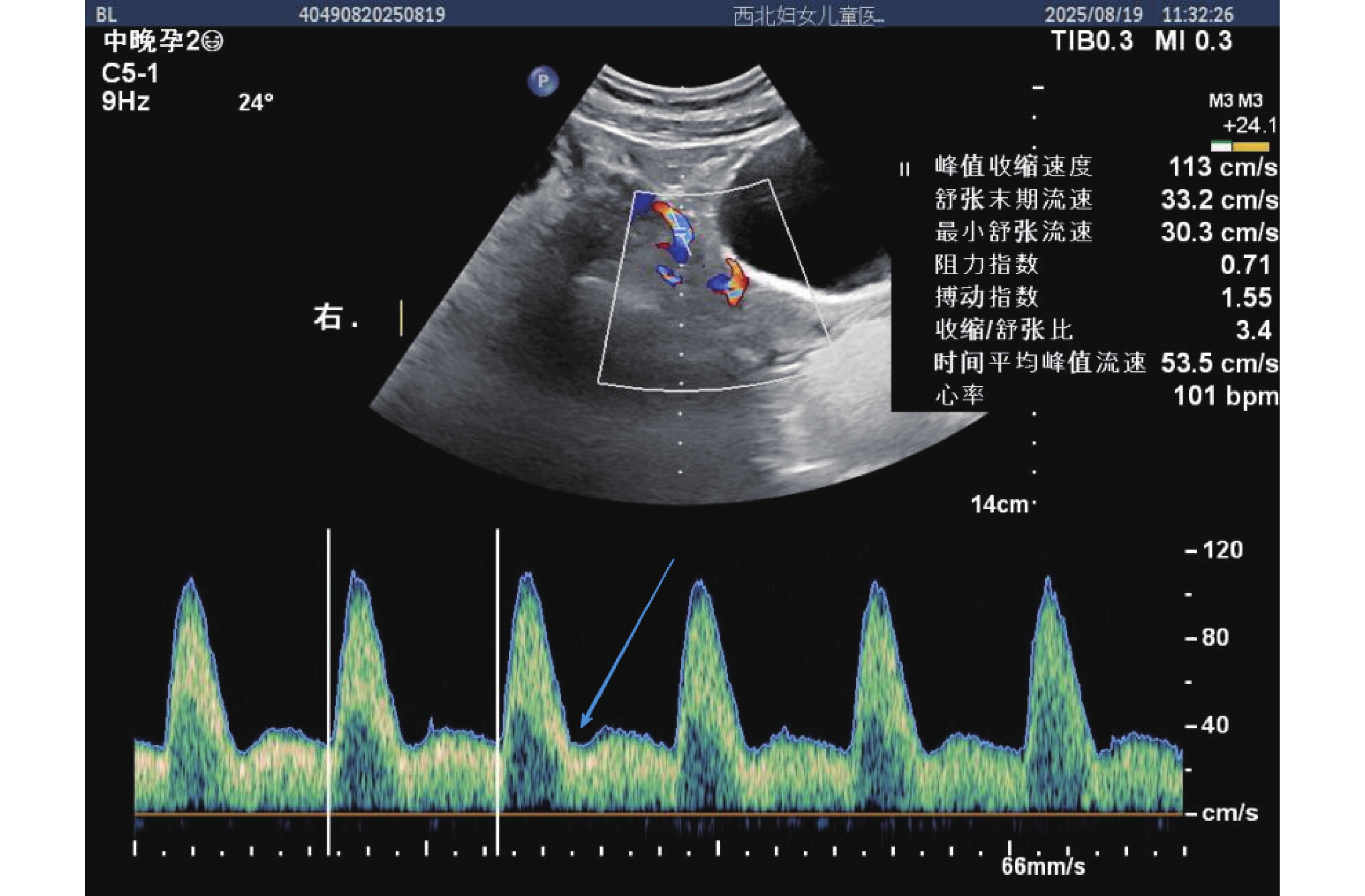
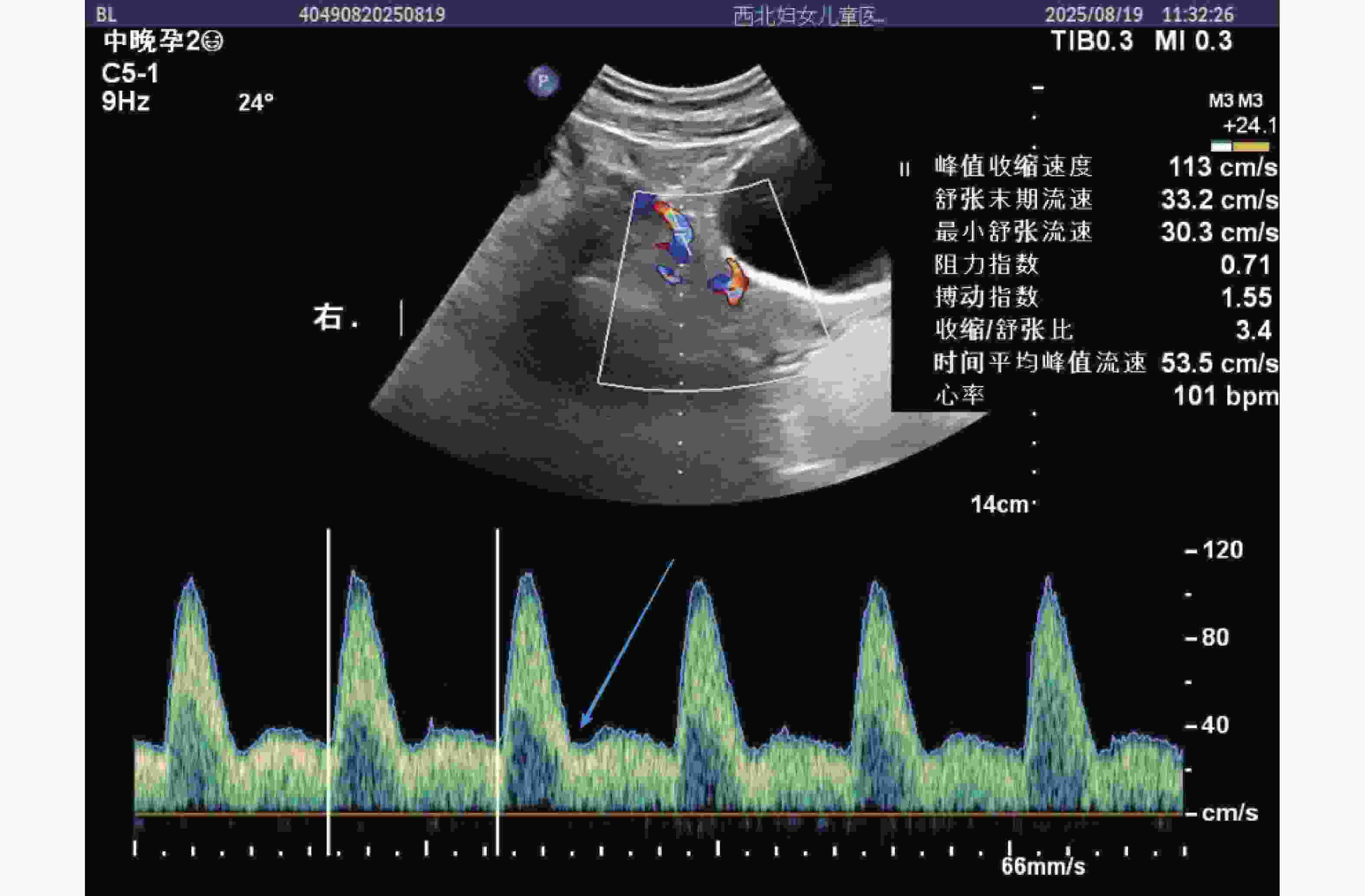
图 1 病例组(孕中期子痫前期孕妇)子宫动脉血流频谱图
注:图中红色圆点标注为 PI(搏动指数,1.55)、RI(阻力指数,0.71)、S/D(收缩 / 舒张比,3.4)测量点,蓝色箭头指示有舒张期切迹,峰值收缩速度113 cm/s,舒张末期流速 33.2 cm/s,反映子宫动脉血流阻力较高,符合子痫前期血流动力学特征。
Figure 1. shows the uterine artery blood flow spectrum of the case group (pregnant women with preeclampsia in the second trimester of pregnancy)
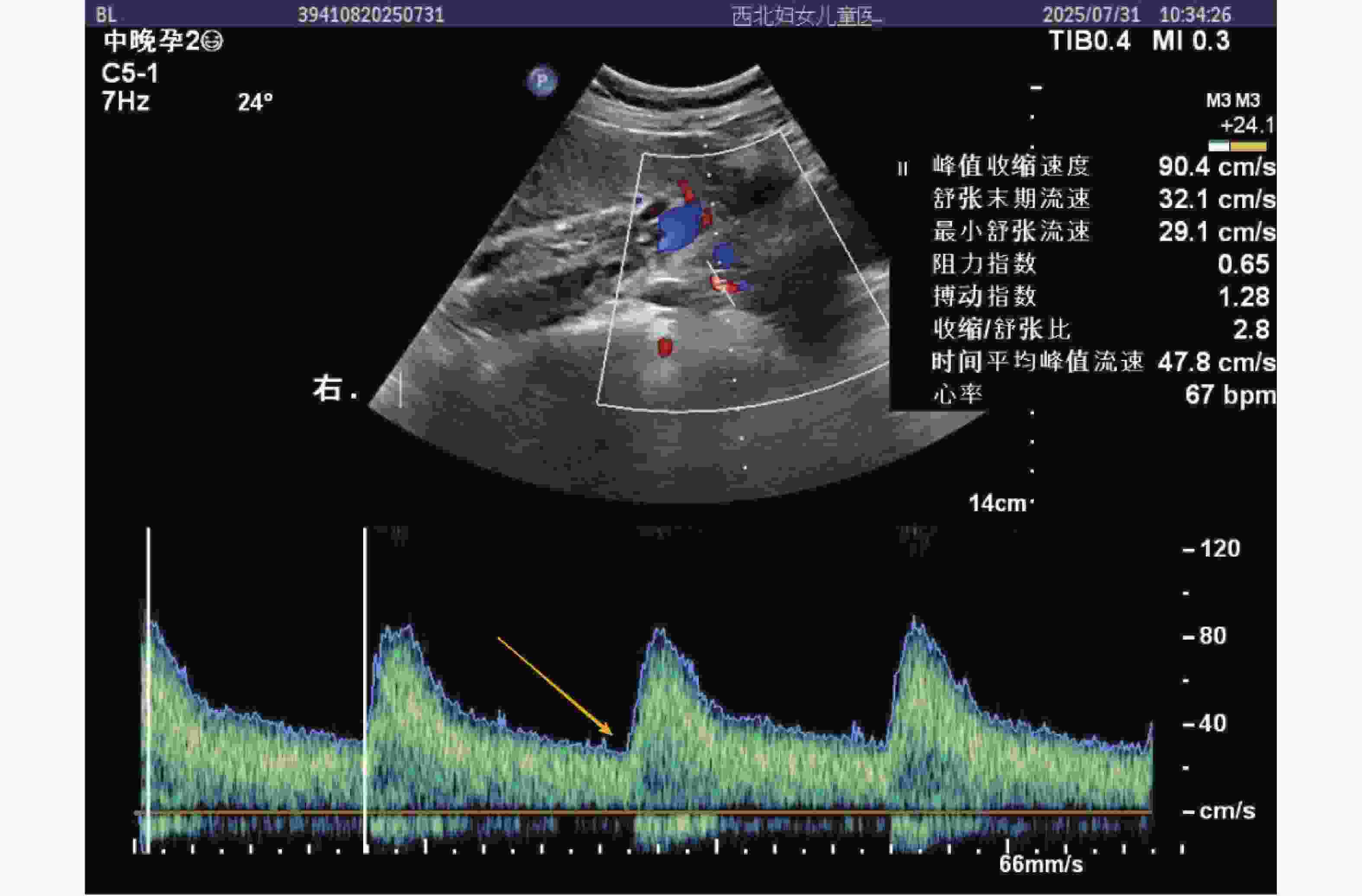
图 2 正常组(健康常规检查孕中期孕妇)子宫动脉血流频谱图
注:图中红色圆点标注 PI(1.28)、RI(0.65)、S/D(2.8)测量点,黄色箭头指示舒张期流速平稳段(无切迹),峰值收缩速度 90.4 cm/s,舒张末期流速 32.1 cm/s,血流阻力较低,符合正常孕中期子宫动脉血流特征,时间平均峰值流速 47.8 cm/s,提示胎盘灌注充足。
Figure 2. shows the uterine artery blood flow spectrum of the normal group (pregnant women in the second trimester of pregnancy undergoing routine health check-ups)
表 1 两组孕妇一般基线资料对比($\bar x \pm s $)
Table 1. Comparison of general baseline data between the two groups of pregnant women ($\bar x \pm s $)
组别 病例组(n = 123) 正常组(n = 105) t P 年龄(岁) 26.71 ± 3.55 26.62 ± 4.39 0.171 0.864 孕周(周) 20.45 ± 3.72 20.38 ± 3.73 0.002 0.998 BMI(kg/m2) 23.86 ± 2.43 23.92 ± 2.67 0.178 0.859 表 2 两组孕妇子宫动脉血流参数、血清指标对比($\bar x \pm s $)
Table 2. Comparison of uterine artery blood flow parameters and serum indexes between the two groups of pregnant women($\bar x \pm s $)
组别 病例组(n = 123) 正常组(n = 105) t P PI 3.38 ± 1.44 2.58 ± 0.38 5.529 <0.001** RI 0.77 ± 0.02 0.58 ± 0.09 22.772 <0.001** S/D 值 4.44 ± 1.52 3.39 ± 0.13 7.054 <0.001** SOCS-3(μg/L) 2.73 ± 0.26 3.42 ± 0.52 12.945 <0.001** Fibulin-3(μg/L) 10.54 ± 1.33 5.74 ± 1.47 25.875 <0.001** **P < 0.001。 表 3 妊娠中期子痫前期孕妇妊娠不良结局情况(%)
Table 3. Pregnancy adverse outcome of preeclampsia patients in the middle of pregnancy (%)
妊娠不良结局 n 占比(%) 早产 3 8.57 胎儿生长受限 5 14.59 胎盘早剥 10 28.57 子痫 7 20.00 产后出血 10 28.57 合计 35 100.00 表 4 妊娠中期子痫前期孕妇妊娠结局的单因素分析[n(%)/($\bar x \pm s $)]
Table 4. Univariate analysis of pregnancy outcomes in women with preeclampsia in the second trimester [n(%)/($\bar x \pm s $)]
指标 不良组(n = 35) 良好组(n = 88) t/χ2 P 年龄(岁) 26.49 ± 3.42 26.53 ± 3.36 0.059 0.953 孕周(周) 20.33 ± 4.48 20.34 ± 4.63 0.011 0.991 BMI(kg/m2) 23.96 ± 1.52 23.89 ± 1.42 0.242 0.809 收缩压(mmHg) 155.62 ± 2.38 155.85 ± 2.44 0.475 0.636 舒张压(mmHg) 98.59 ± 1.44 98.61 ± 1.38 0.072 0.943 产次n(%) 1次 15(42.86) 50(56.82) 1.959 0.162 ≥2次 20(57.14) 38(43.18) PI 4.92 ± 1.29 3.26 ± 1.02 7.534 <0.001** RI 0.92 ± 0.07 0.75 ± 0.06 13.509 <0.001** S/D 值 5.86 ± 1.21 4.35 ± 0.41 10.357 <0.001 SOCS-3(μg/L) 2.58 ± 0.18 2.92 ± 0.16 10.258 <0.001** Fibulin-3(μg/L) 12.45 ± 1.33 8.21 ± 1.24 16.760 <0.001** Cr(μmol/L) 88.47 ± 6.77 88.62 ± 7.09 0.107 0.915 铁蛋白(μg/L) 104.33 ± 12.37 105.46 ± 15.46 0.386 0.700 FPG(mmol/L) 4.65 ± 1.81 4.56 ± 1.83 0.247 0.805 LDL-C(mmol/L) 2.36 ± 1.26 2.56 ± 1.52 0.689 0.492 HCT(%) 40.42 ± 2.33 40.63 ± 2.47 0.432 0.666 HB(g/L) 139.34 ± 5.23 139.64 ± 5.35 0.282 0.778 Lac(mmol/L) 1.02 ± 0.26 1.03 ± 0.18 0.243 0.808 ALT(U/L) 22.45 ± 1.36 22.33 ± 1.72 0.369 0.713 AST(U/L) 30.55 ± 2.63 30.98 ± 2.38 0.877 0.382 尿蛋白(g/24 h) 0.31 ± 0.05 0.30 ± 0.04 1.163 0.247 BMI:体质量指数;Cr:肌酐;FPG:空腹血糖;LDL-C:低密度脂蛋白胆固醇;HCT:红细胞压积;HB:血红蛋白;Lac:乳酸;ALT:丙氨酸氨基转移酶;AST:天冬氨酸氨基转移酶;PI:搏动指数;RI:阻力指数;S/D 值:收缩期峰值流速与舒张末期流速比值;SOCS-3:细胞因子信号抑制因子 3;Fibulin-3:纤维蛋白 3;**P < 0.001。 表 5 变量赋值
Table 5. Variable Assignment
变量 编码 赋值方式 因变量 妊娠结局 Y 良好=0;不良=1 自变量 Fibulin-3 X1 原始数据代入 RI X2 原始数据代入 S/D值 X3 原始数据代入 SOCS-3 X4 原始数据代入 PI X5 原始数据代入 表 6 妊娠中期子痫前期孕妇妊娠不良结局发生的Logistic分析
Table 6. Logistic analysis of adverse pregnancy outcomes in women with preeclampsia during mid-pregnancy
影响因素 β SE Waldχ2 值 P OR 95%CI 下限 上限 Fibulin-3升高 4.767 1.738 7.522 0.006* 117.524 3.897 354.402 RI升高 1.735 0.484 12.826 <0.001** 5.667 2.193 14.642 S/D 值升高 2.286 0.423 29.195 <0.001 9.840 4.293 22.553 SOCS-3降低 −10.402 1.882 30.560 <0.001** 0.585 0.303 0.928 PI升高 1.044 0.220 22.464 <0.001** 2.842 1.845 4.377 常数项 −37.863 6.128 38.756 <0.001** − − − **P < 0.001;*P < 0.05 -
[1] Hauspurg A, Jeyabalan A. Postpartum preeclampsia or eclampsia: Defining its place and management among the hypertensive disorders of pregnancy[J]. Am J Obstet Gynecol, 2022, 226(2): S1211-S1221. doi: 10.1016/j.ajog.2020.10.027 [2] Rosenberg E A, Seely E W. Update on preeclampsia and hypertensive disorders of pregnancy[J]. Endocrinol Metab Clin N Am, 2024, 53(3): 377-389. doi: 10.1016/j.ecl.2024.05.012 [3] Sakowicz A, Bralewska M, Rybak-Krzyszkowska M, et al. New ideas for the prevention and treatment of preeclampsia and their molecular inspirations[J]. Int J Mol Sci, 2023, 24(15): 12100. doi: 10.3390/ijms241512100 [4] Tyrmi J S, Kaartokallio T, Lokki AI, et al; FINNPEC study group, finnGen project, and the estonian biobank research team. genetic risk factors associated with preeclampsia and hypertensive disorders of pregnancy[J]. JAMA Cardiol, 2023, 8(7): 674-683. doi: 10.1001/jamacardio.2023.1312 [5] 赵晓爽, 胡玉博, 朱林凤. 血清PLGF、IGF-1及sFLT-1水平对子痫前期孕妇妊娠结局的预测价值[J]. 川北医学院学报, 2023, 38(8): 1078-1081. [6] 王泽华. 妇产科学(第9版)[M]. 人民卫生出版社, 2018.07. 36-39. [7] Tucker M J, Berg C J, Callaghan W M, et al. The black-white disparity in pregnancy-related mortality from 5 conditions: Differences in prevalence and case-fatality rates[J]. Am J Public Health, 2007, 97(2): 247-251. doi: 10.2105/AJPH.2005.072975 [8] 许琳, 王茹, 张忠霞, 等. 基于血清外泌体miRNA-517建立子痫前期不良妊娠结局预测模型及验证[J]. 中国计划生育和妇产科, 2024, 16(11): 49-53. [9] 肖颜丹, 林琴, 林美玲, 等. 子宫动脉血流参数联合血清VEGFR2、sEng对子痫前期患者胎儿生长受限的预测价值[J]. 现代生物医学进展, 2025, 25(1): 168-173. doi: 10.13241/j.cnki.pmb.2025.01.024 [10] Yagel S, Cohen S M, Admati I, et al. Expert review: Preeclampsia type I and type II[J]. Am J Obstet Gynecol MFM, 2023, 5(12): 101203. doi: 10.1016/j.ajogmf.2023.101203 [11] Miller E C, Wilczek A, Bello N A, et al. Pregnancy, preeclampsia and maternal aging: From epidemiology to functional genomics[J]. Ageing Res Rev, 2022, 73: 101535. doi: 10.1016/j.arr.2021.101535 [12] Donel S, Novri D A, Hamidy Y, et al. Effectiveness of nifedipine, labetalol, and hydralazine as emergency antihypertension in severe preeclampsia: A randomized control trial[J]. F1000Research, 2023, 11: 1287. [13] Francisco C, Gamito M, Reddy M, et al. Screening for preeclampsia in twin pregnancies[J]. Best Pract Res Clin Obstet Gynaecol, 2022, 84: 55-65. doi: 10.1016/j.bpobgyn.2022.03.008 [14] Chiang Y T, Seow K M, Chen K H. The pathophysiological, genetic, and hormonal changes in preeclampsia: A systematic review of the molecular mechanisms[J]. Int J Mol Sci, 2024, 25(8): 4532. doi: 10.3390/ijms25084532 [15] Dennis A T, Xin A, Farber M K. Perioperative management of patients with preeclampsia: A comprehensive review[J]. Anesthesiology, 2025, 142(2): 378-402. doi: 10.1097/ALN.0000000000005296 [16] Roberts J M. Preeclampsia epidemiology(ies) and pathophysiology(ies)[J]. Best Pract Res Clin Obstet Gynaecol, 2024, 94: 102480. doi: 10.1016/j.bpobgyn.2024.102480 [17] Dennis A T, Xin A, Farber M K. Perioperative management of patients with preeclampsia: A comprehensive review[J]. Anesthesiology, 2025, 142(2): 378-402. doi: 10.1097/ALN.0000000000005296 [18] Chen Y, Ou Z, Pang M, et al. Extracellular vesicles derived from Akkermansia muciniphila promote placentation and mitigate preeclampsia in a mouse model[J]. J Extracellular Vesicle, 2023, 12(5): 12328. doi: 10.1002/jev2.12328 [19] Wang Y, Li B, Zhao Y. Inflammation in preeclampsia: Genetic biomarkers, mechanisms, and therapeutic strategies[J]. Front Immunol, 2022, 13: 883404. doi: 10.3389/fimmu.2022.883404 [20] 王伟丽, 刘宁, 李婉, 等. 高表达miR-431对子痫前期孕妇的诊断价值及不良妊娠结局的预测[J]. 现代妇产科进展, 2024, 33(12): 910-914. doi: 10.13283/j.cnki.xdfckjz.2024.12.031 [21] 管亚丽, 杨辰敏. 孕晚期脐动脉超声检测联合MBPS预测子痫前期孕产妇不良围生儿结局价值[J]. 中国计划生育学杂志, 2023, 31(8): 1995-1999. [22] Ghesquiere L, Guerby P, Marchant I, et al. Comparing aspirin 75 to 81 Mg vs 150 to 162 Mg for prevention of preterm preeclampsia: Systematic review and meta-analysis[J]. Am J Obstet Gynecol MFM, 2023, 5(7): 101000. doi: 10.1016/j.ajogmf.2023.101000 -





 下载:
下载: