Clinical Features and Prognosis of Acute Macular Neuroretinopathy Associated with Novel Coronavirus Infection
-
摘要:
目的 观察新型冠状病毒感染(COVID-19)相关急性黄斑神经视网膜病变(AMN)患者的临床特征及预后。 方法 回顾性临床研究。选取2022年12月至2023年2月就诊于云南大学附属医院眼科确诊为COVID-19相关AMN的13例患者资料,以及2020年至2023年在PubMed和Web of Science数据库中发表的13篇病例报道以及病例系列研究共41例患者的病例资料,分析其临床、眼科影像学及预后结果。 结果 临床病例组共13例25只眼纳入研究,平均年龄(30.23±6.02)岁,其中女性10例。文献病例组共41例72只眼,平均年龄为(30.12±13.24)岁,其中女性患者31例。(1)COVID-19症状/诊断与眼科症状之间的持续时间:临床病例组为3(2.0,4.0)d,文献病例组为2(0.75,5.0)d;(2)临床特点:临床病例组中12例(92.31%)为双眼发病。文献病例组中 31例(75.61%)为双眼发病。两组症状均以视物暗点为主,其次为视力下降;(3)辅助检查:临床病例组中13例患者光学相干断层扫描(OCT)均可见椭圆体带(EZ)和/或嵌合体带(IZ)断裂,伴外丛状层(OPL)、外核层(ONL)强反射,近红外照相(NIR)均显示黄斑中心凹周围低反射楔形病灶,部分患者光学相干断层扫描血管成像(OCTA)均可观察到深层毛细血管层(DCP)及脉络膜毛细血管层(CC)血流减少,7例伴有棉绒斑的患者同时存在浅层毛细血管层(SCP)血流减少,文献病例组中33例患者OCT可见EZ和/或IZ断裂;(4)治疗及预后:13例患者中11例予以口服糖皮质激素治疗,2例予以观察,1年后视力提高者23只眼,1例患者仍存在视野缺损,1例在治疗过程中发生视网膜静脉阻塞继发黄斑水肿,1例外核层(ONL)及外丛状层(OPL)出现低反射信号。 结论 COVID-19相关AMN发病年龄稍大,多双眼发病,症状以视物暗点为主,多伴视力下降,NIR示中心凹周围低反射楔形病灶,OCT示EZ和/或IZ断裂为主,OCTA示DCP及CC层血流密度降低。COVID-19相关AMN视力预后良好,但需警惕视网膜静脉阻塞等并发症的发生。 -
关键词:
- SARS-CoV-2 /
- COVID-19 /
- 急性黄斑区神经视网膜病变 /
- 临床特征 /
- 预后
Abstract:Objective To Observe the clinical characteristics and prognosis of patients with the acute macular neuroretinopathy (AMN) associated with novel coronavirus infection(COVID-19). Methods The data of 13 patients diagnosed with COVID-19-associated AMN attending the Department of Ophthalmology of the Affiliated Hospital of Yunnan University from December 2022 to February 2023, as well as 13 case reports in PubMed and Web of Science databases from 2020 to 2023 and a case series study totaling 41 patients were retrospectively selected and analyzed for their ophthalmic imaging and prognostic outcomes in clinic. Results A total of 13 cases with 25 eyes in the clinical case group were included in the study with a mean age of 30.23±6.02 years, of which 10 were females. The literature case group consisted of 41 cases and 72 eyes with a mean age of 30.12±13.24 years, including 31 female patients. (1) Duration between COVID-19 symptoms/diagnosis and ophthalmic symptoms: 3(2.0, 4.0) days in the clinical case group and 2 (0.75, 5.0) days in the literature case group. (2) Clinical characteristics: 12 (92.31%) of the clinical case group had the binocular onset and the literature case group, 31 (75.61%) had the binocular onset. The symptoms in both groups were mainly dark spots in vision, followed by decreased visual acuity. (3) Ancillary examinations: optical coherence tomography (OCT) showed the ellipsoid zone (EZ) and/or chimeric zone (IZ) breaks with strong reflections in the outer plexiform layer (OPL) and outer nuclear layer (ONL) in 13 patients in the clinical case group, and the near-infrared photography (NIR) showed the low-reflective wedge-shaped foci around the center of the macula, and some patients' optical coherence tomography angiography (OCTA) showed deep capillary lesions, and some patients' OCTA showed low reflectivity. Reduced blood flow in the deep capillary layer (DCP) and choroidal capillary layer (CC) was observed in all patients, 7 patients with cotton-wool spots also had the reduced blood flow in the superficial capillary layer (SCP), and 33 patients in the case group in the literature had the visible EZ and/or IZ breaks on OCT. (4) Treatment and prognosis: 11 out of 13 patients were treated with oral glucocorticoids, 2 were under the observation. After year, the condition of 23 patients had been improved, 1 case had visual field defects, 1 case had retinal vein occlusion secondary to macular edema, and 1 case had a hyporeflective signal in the outer nuclear layer (ONL) and outer plexiform layer (OPL). Conclusion The age of onset of AMN related to COVID-19 is slightly older, with more cases involving both eyes. The main symptom is visual field scotoma, often accompanied by decreased vision. Near-infrared imaging shows low-reflective wedge-shaped lesions around the fovea, and OCT shows mainly disruption of the EZ and/or IZ. OCTA shows decreased blood flow density in the DCP and CC layers. The visual prognosis of AMN related to COVID-19 is good, but vigilance is needed for the occurrence of complications such as retinal vein occlusion -
Key words:
- SARS-CoV-2 /
- COVID-19 /
- Acute macular neuroretinopathy /
- Clinical features /
- Prognosis
-
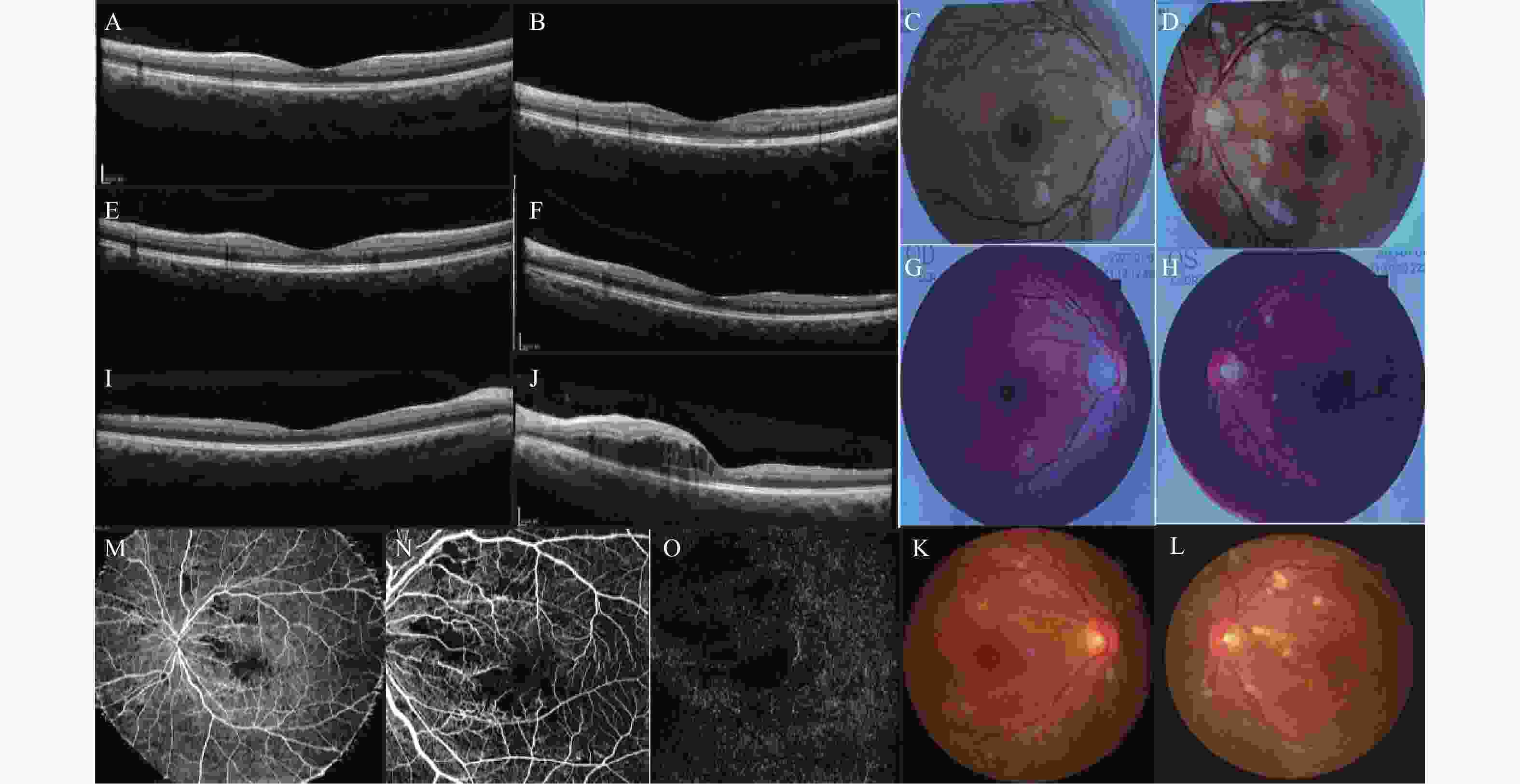
图 1 患者治疗前后相关检查对比(病例1)
A:患者初诊时与治疗后1月双眼超广角眼底照相对比,眼底照相显示黄斑区均可见棕褐色楔形病灶,尖端指向中心,并可见棉绒斑(红色箭头),棉绒斑大约在1个月左右消失;B:初诊时右眼OCT与治疗后1月后对比,初诊时可见OPL及ONL高反射,并且黄斑区EZ及IZ明显断裂(红色箭头),1月后OCT仍可见IZ断裂,ONL变薄;C:初诊时右眼近红外照相(NIR);D:初诊时右眼OCTA的DCP;E:初诊时右眼OCTA的CC,可见与NIR病变共定位处DCP及CC血流减少;F:初诊时左眼视野检查,可见中心暗点;G:1年后左眼视野检查示中心暗点,此时视力VOD:0.9,VOS:0.5,双眼视力均明显提升,但左眼仍存在中心暗点。
Figure 1. Comparison of relevant examinations before and after treatment of the patient(Case1)
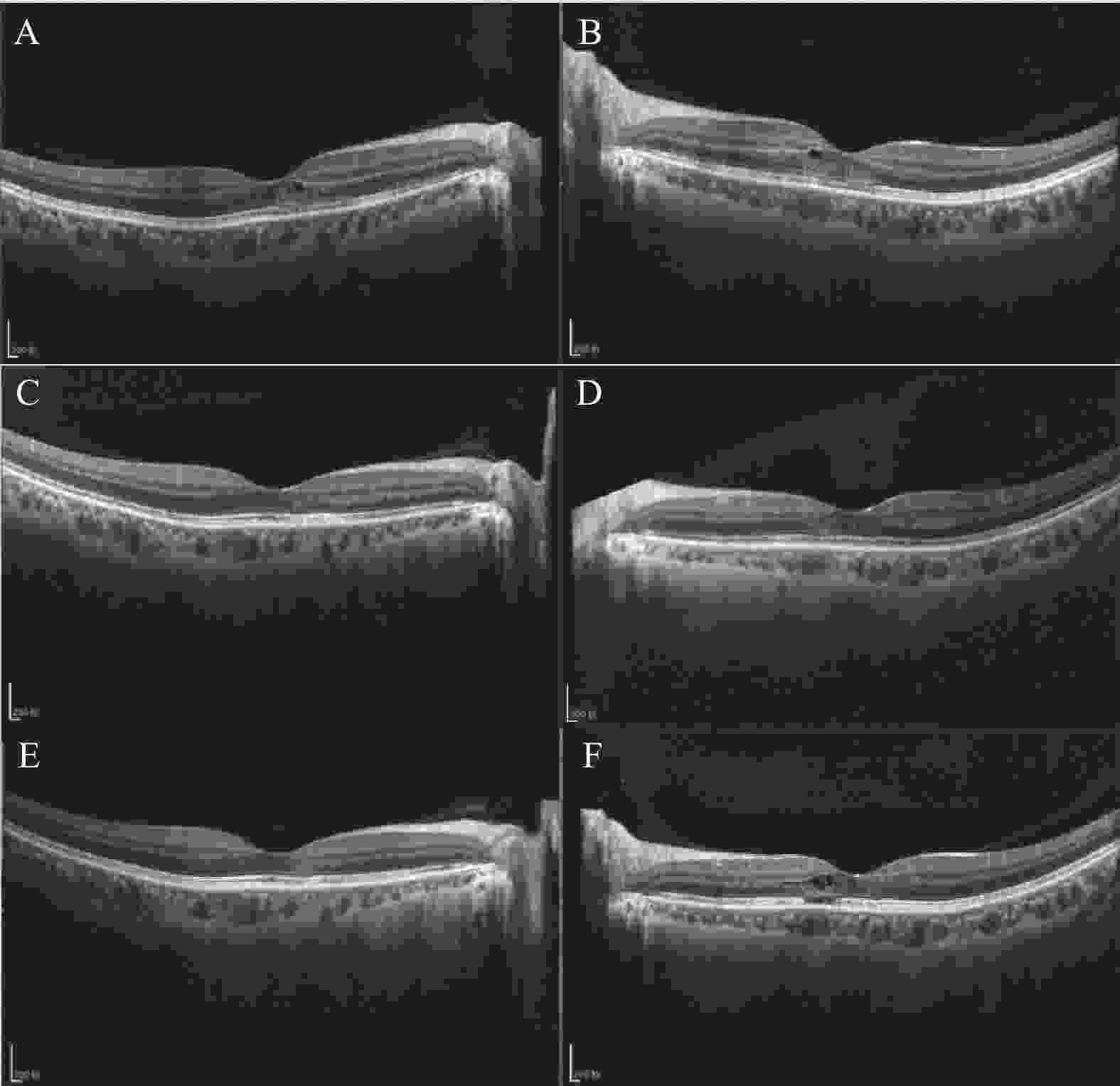
图 2 患者治疗前后相关检查对比(病例6)
A~B:患者初诊时双眼OCT,可见OPL及ONL高反射信号,EZ及IZ部分缺失断裂;C~D:初诊时外院眼底照相,黄斑区可见棕褐色楔形病灶,并可见大量棉绒斑;E~F:口服激素治疗1月后双眼OCT,双眼视力OD:0.8,OS:0.6,双眼OCT可见ONL及OPL高反射减少,ONL变薄;G~H:治疗1月后双眼眼底照相,可见棉绒斑明显减少;I:1年后右眼OCT,未见明显异常;J:1年后左眼OCT,可见黄斑囊样水肿;K~L:1年后双眼眼底照相,可见左眼散在点片状出血及棉绒斑,1年后双眼视力OD:1.0,OS:0.12;M:左眼广角OCTA,黄斑区及视盘鼻侧可见无灌注区;N:SCP;O:DCP,均可见黄斑区无灌注。
Figure 2. Comparison of relevant examinations before and after treatment of the patient(Case6)
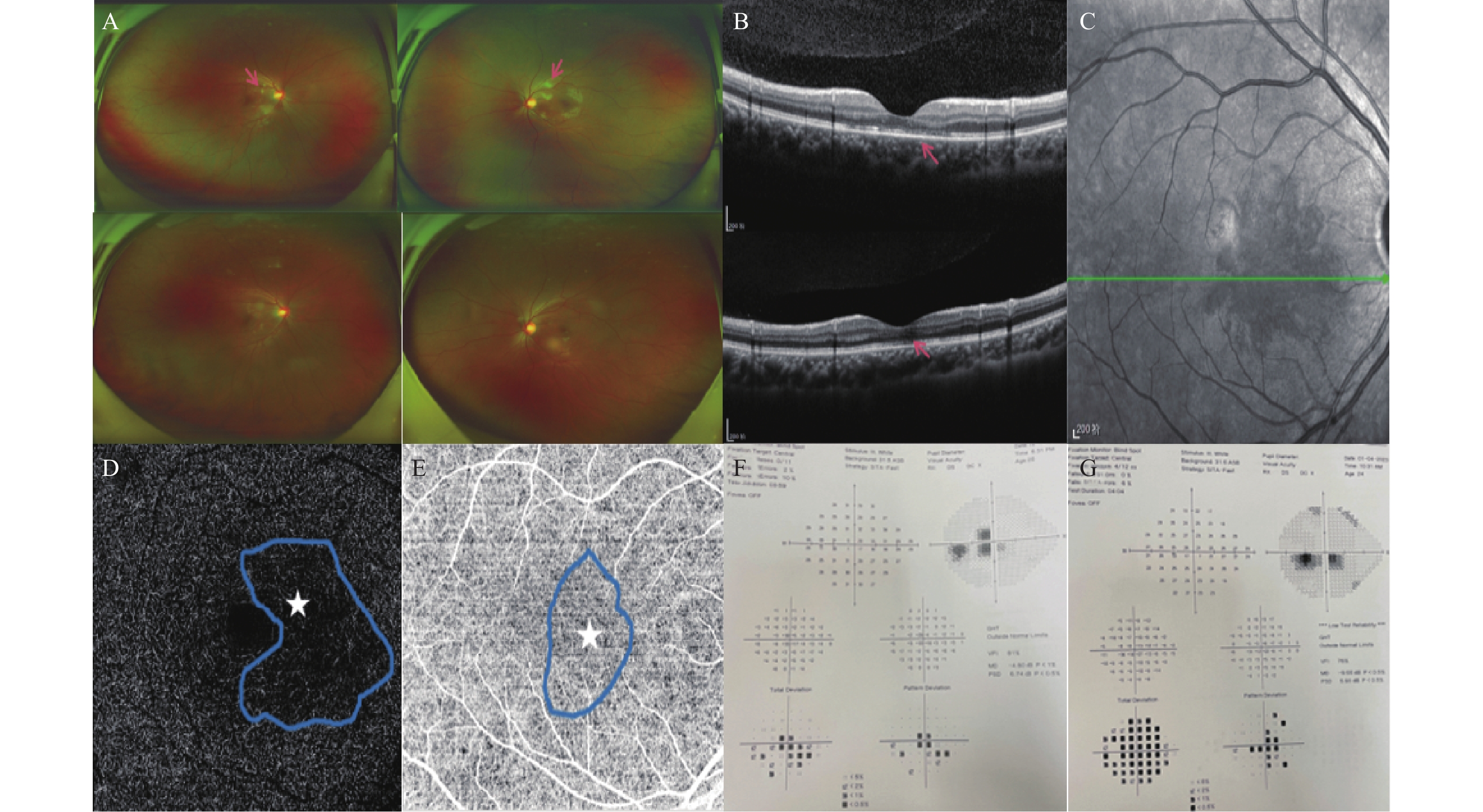
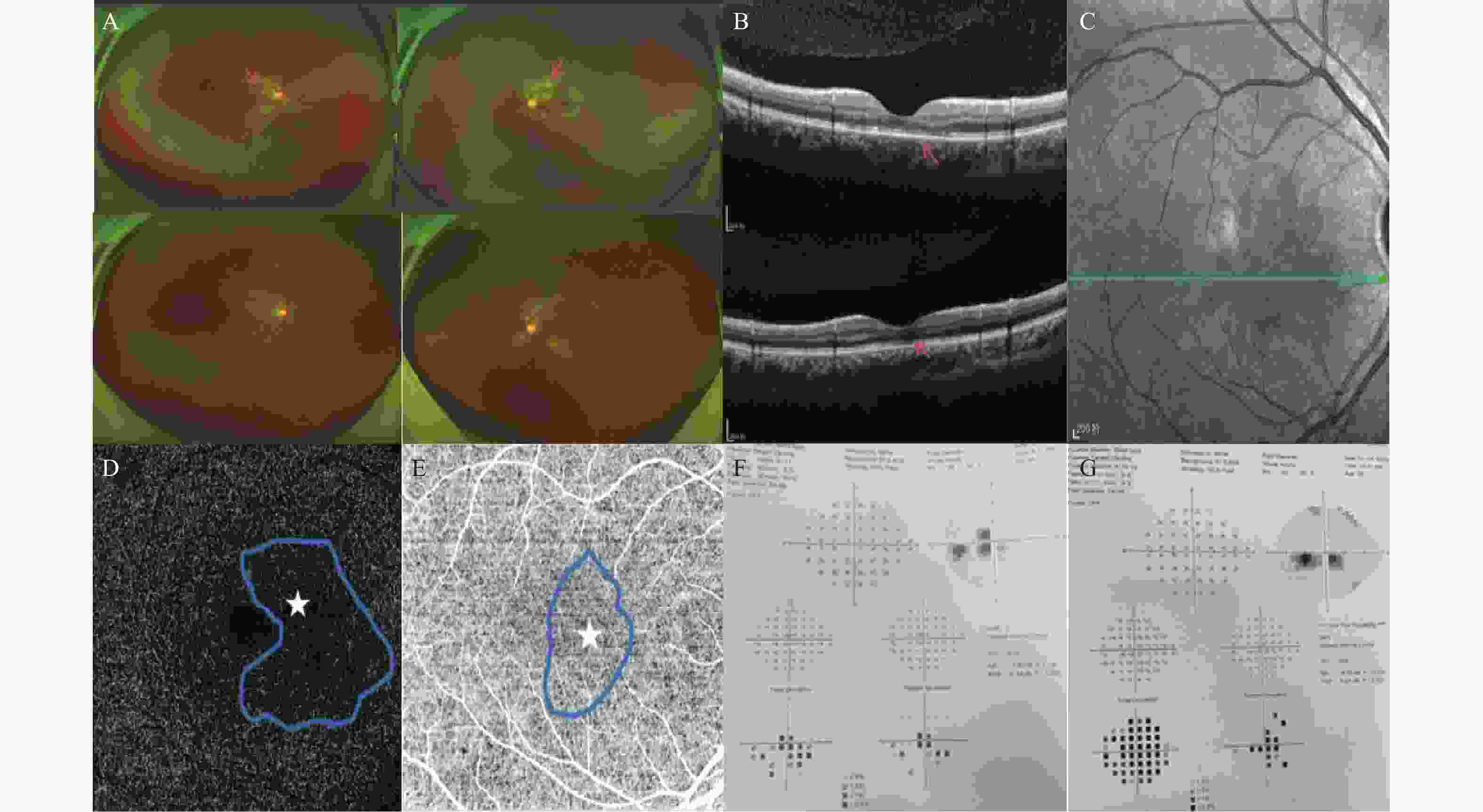
图 3 治疗前后OCT对比(病例4)
A:初诊时右眼OCT;B:左眼OCT,可见双眼OPL及ONL出现低反射信号(囊腔),中心凹下可见ONL及OPL高反射信号,EZ及IZ不连续;C~D:治疗1月后双眼OCT,可见囊腔消失,OPL、ONL高反射信号逐渐减弱,此时双眼视力较前提升,OD:0.4,OS:0.1;E~F:治疗1年后双眼OCT,双眼视力OD:0.6,OS:0.5,OCT表现示ONL变薄,右眼IZ仍部分缺失,左眼可见黄斑区ONL及OPL可见低反射信号(囊腔),与初诊时低反射信号(囊腔)位置一致,EZ及IZ部分明显缺失。
Figure 3. OCT comparison before and after treatment (Case4)
表 1 13例AMN患者资料
Table 1. Information on 13 patients with AMN
病例 性别/
年龄(岁)眼别 视物暗点
和(或)视
力下降其他(如视物变形、视野缺损等) BCVA
(OD/OS)确诊至出现
眼部症状的
时间(d)ONL与OPL
高反射EZ/IZ断裂 NIR示黄斑中心凹周围低反射楔形病灶 OCTA
示DCP
血流减少初诊 随访 初诊 随访 初诊 随访 初诊 随访 初诊 随访 初诊 随访 1 男/25 双眼 有 有 有 有 CF/CF 0.9/0.5 1 有 无 有 有 有 无 有 2 女/35 双眼 有 无 无 无 0.04/0.04 0.6/0.6 4 有 无 有 有 有 无 有 3 女/27 双眼 有 无 无 无 0.3/0.5 1.0/1.0 3 有 无 有 无 有 无 有 4 女/45岁 双眼 有 无 无 无 CF/CF 0.6/0.5 4 有 无 有 有 有 无 有 5 男/34岁 双眼 有 无 无 无 0.02/CF 0.8/0.8 2 有 无 有 无 有 无 有 6 男/25岁 双眼 有 有 无 有 0.08/0.1 1.0/0.12 2 有 无 有 有 有 无 有 7 女/27岁 右眼 有 无 无 无 0.6/0.8 1.0/0.8 5 无 无 有 无 有 无 有 8 女/31岁 双眼 有 无 无 无 0.2/0.2 1.0/0.9 3 有 无 有 无 有 无 有 9 女/35岁 双眼 有 无 无 无 0.4/0.8 0.9/1.0 10 有 无 有 无 有 无 有 10 女/23岁 双眼 有 无 无 无 CF/CF 0.6/0.6 2 有 无 有 有 有 无 有 11 女/25岁 双眼 有 无 无 无 0.3/0.3 0.8/0.8 5 有 无 有 无 有 无 有 12 女/30岁 双眼 有 无 无 无 0.02/0.02 0.8/1.0 2 有 无 有 无 有 无 有 13 女/31岁 双眼 有 无 无 无 0.04/0.04 1.0/0.8 1 有 无 有 无 有 无 有 表 2 文献病例组的与新型冠状病毒感染相关AMN病例资料
Table 2. Information on AMN cases associated with novel coronavirus infections from literature case groups
序号 文献 性别/年龄(岁) 眼别 症状 初诊BCVA
(OD/OS)确诊COVID至出现
眼部症状的时间ONL与OPL
高反射EZ/IZ
断裂1 El Matri K,et al[10]. 女/75 双眼 旁中心暗点 NR 1月 有 有 2 Virgo J,et al[5]. 男/32 右眼 旁中心暗点 1.0/NR 16 d 有 有 3 Macé T,et al[11]. 女/39 双眼 旁中心暗点 1.0/1.0 2 d 有 无 4 Capuano V,et al[12]. 女/37 双眼 旁中心暗点 1.0/1.0 NR 有 有 5 Giacuzzo C,et al[13]. 女/23 双眼 旁中心暗点 1.0/1.0 1 d 有 有 6 Yılmaz Çebi A,et al[14]. 女/29 双眼 视野缺损、旁中心暗点 0.5/0.7 1 d 有 有 7 Goyal M,et al[15]. 男/32 右眼 旁中心暗点 1.0/NR 4月 有 有 8 Gascon P,et al[16]. 男/53 左眼 视物暗点、视力下降 NLP/0.3 8 d 有 有 9 Mitamura M,et al[17]. 女/24 双眼 视物变形 1.2/1.2 1 d 无 有 10 Aidar MN,et al[18]. 女/71 左眼 视力下降 NR/0.5 14 d 无 有 11 Jalink MB,et al[19]. 女/21 右眼 视物暗点 NR/NR 6周 不规则 无 12 女/29 左眼 视物暗点 NR/NR 5月 细微变化 无 13 Liu YC,et al[20]. 男/19 双眼 视力下降 0.3/0.3 5 d 有 无 14 男/35 双眼 视力下降、视物模糊 0.9/0.3 5 d 有 无 15 女/17 双眼 视力下降 0.05/0.01 4 d 有 无 16 男/28 双眼 视力下降 0.01/0.01 4 d 有 有 17 男/37 双眼 视物暗点 1.0/1.0 2 d 有 无 18 女/42 双眼 视物模糊 0.8/0.7 3 d 有 无 19 女/32 双眼 视力下降、视物模糊 0.4/0.2 4 d 有 无 20 女/42 双眼 视力下降 0.1/0.04 3 d 有 无 21 女/19 双眼 视力下降、视物模糊 1.0/0.02 1 d 有 无 22 女/30 双眼 视力下降、视物模糊 0.2/0.4 2 d 有 无 23 女/49 双眼 视力下降 0.5/0.9 5 d 有 无 24 女/23 双眼 视力下降 0.4/0.2 1 d 有 无 25 男/16 双眼 视力下降 0.05/0.6 2 d 有 无 26 女/30 双眼 视力下降、视物模糊 0.4/0.5 3 d 有 无 27 Dinh RH,et al[21]. 女/24 左眼 视物模糊,暗点 NR/1.0 2 d 视网膜外层结构断裂 无 28 女/11 双眼 视物模糊、红肿、
畏光、暗点0.5/0.4 当天 视网膜外层结构断裂 无 29 女/19 双眼 双眼中央灰色暗点 0.15/0.04 14 d 有 有 30 女/20 双眼 视物模糊、暗点 1.0/1.0 当天 视网膜外层结构断裂 无 31 女/22 双眼 视物暗点、畏光 1.0/0.8 1 d前 有,ONL变薄 有 32 女/32 左眼 视物暗点 NR/1.0 当天 视网膜外层结构断裂 无 33 男/30 右眼 视物暗点 1.0/NR 当天 视网膜外层结构断裂 无 34 女/23 双眼 视物暗点、头痛 1.0/1.0 2 d 视网膜外层结构断裂 无 35 女/41 左眼 视物暗点、头痛 NR/1.0 当天 视网膜外层结构断裂 无 36 男/20 双眼 视物暗点 1.0/1.0 当天 视网膜外层结构断裂 无 37 女/13 双眼 视物暗点、头痛 1.0/1.0 当天 有 有 38 男/32 双眼 视物暗点 1.0/1.0 当天 视网膜外层结构断裂 无 39 女/21 双眼 视物暗点 1.0/1.0 1 d前 视网膜外层结构断裂 无 40 女/21 双眼 视物暗点、呕吐 0.8/0.8 1 d 视网膜外层结构断裂 无 41 女/26 左眼 视物暗点、头痛 NR/1.0 当天 视网膜外层结构断裂 无 NR:未报道;BCVA:最佳矫正视力;OD:右眼;OS:左眼。 -
[1] 周诗银,吴强. 新型冠状病毒肺炎与心血管系统疾病[J]. 心血管病学进展,2021,42(11):982-985. [2] Walinjkar J A,Makhija S C,Sharma H R,et al. Central retinal vein occlusion with COVID-19 infection as the presumptive etiology[J]. Indian J Ophthalmol,2020,68(11):2572-2574. doi: 10.4103/ijo.IJO_2575_20 [3] Sheth J U,Narayanan R,Goyal J,et al. Retinal vein occlusion in COVID-19: A novel entity[J]. Indian J Ophthalmol,2020,68(10):2291-2293. doi: 10.4103/ijo.IJO_2380_20 [4] Pereira L A, Soares L, Nascimento P A, et al. Retinal findings in hospitalised patients with severe COVID-19[J]. Br J Ophthalmol,2022,106(1):102-105. [5] Virgo J,Mohamed M. Paracentral acute middle maculopathy and acute macular neuroretinopathy following SARS-CoV-2 infection[J]. Eye (Lond),2020,34(12):2352-2353. doi: 10.1038/s41433-020-1069-8 [6] Feigl B,Haas A. Optical coherence tomography (OCT) in acute macular neuroretinopathy[J]. Acta Ophthalmol Scand,2000,78(6):714-716. doi: 10.1034/j.1600-0420.2000.078006714.x [7] Sarraf D,Rahimy E,Fawzi A A,et al. Paracentral acute middle maculopathy: A new variant of acute macular neuroretinopathy associated with retinal capillary ischemia[J]. JAMA Ophthalmol,2013,131(10):1275-1287. doi: 10.1001/jamaophthalmol.2013.4056 [8] Lee S Y,Cheng J L,Gehrs K M,et al. Choroidal features of acute macular neuroretinopathy via optical coherence tomography angiography and correlation with serial multimodal imaging[J]. JAMA Ophthalmol,2017,135(11):1177-1183. doi: 10.1001/jamaophthalmol.2017.3790 [9] Fawzi A A,Pappuru R R,Sarraf D,et al. Acute macular neuroretinopathy: Long-term insights revealed by multimodal imaging[J]. Retina,2012,32(8):1500-1513. doi: 10.1097/IAE.0b013e318263d0c3 [10] El Matri K,Werda S,Chebil A,et al. Acute macular outer retinopathy as a presumed manifestation of COVID-19[J]. Journal Francais D'ophtalmologie,2021,44(8):1274-1277. doi: 10.1016/j.jfo.2021.06.002 [11] Macé T,Pipelart V. Acute macular neuroretinopathy and SARS-CoV-2 infection: Case report[J]. Journal Francais D'ophtalmologie,2021,44(9):e519-e521. doi: 10.1016/j.jfo.2021.07.004 [12] Capuano V,Forte P,Sacconi R,et al. Acute macular neuroretinopathy as the first stage of SARS-CoV-2 infection[J]. European Journal of Ophthalmology,2023,33(3):P105-P111. doi: 10.1177/11206721221090697 [13] Giacuzzo C,Eandi C M,Kawasaki A. Bilateral acute macular neuroretinopathy following COVID-19 infection[J]. Acta Ophthalmologica,2022,100(2):e611-e612. [14] Yılmaz Çebi A,Kılıçarslan O,Uçar D. Coincident acute macular neuroretinopathy and paracentral acute middle maculopathy in COVID-19[J]. Turkish Journal of Ophthalmology,2023,53(2):120-123. doi: 10.4274/tjo.galenos.2022.55156 [15] Goyal M,Murthy S I,Annum S. Retinal manifestations in patients following COVID-19 infection: A consecutive case series[J]. Indian Journal of Ophthalmology,2021,69(5):1275-1282. doi: 10.4103/ijo.IJO_403_21 [16] Gascon P, Briantais A, Bertrand E, et al. Covid-19-associated retinopathy: A case report[J]. Ocul Immunol Inflamm,2020,28(8):1293-1297. [17] Mitamura M,Kase S,Hirooka K,et al. Choroidal circulatory and vascular morphological changes in acute macular neuroretinopathy after infection with severe acute respiratory syndrome coronavirus 2: A case report with literature review[J]. In Vivo (Athens,Greece),2023,37(6):2869-2876. doi: 10.21873/invivo.13405 [18] Aidar M N,Gomes T M,de Almeida M Z H,et al. Low visual acuity due to acute macular neuroretinopathy associated with COVID-19: A case report[J]. The American Journal of Case Reports,2021,22(3):e163-e169. [19] Jalink M B, Bronkhorst I H G. A sudden rise of patients with acute macular neuroretinopathy during the COVID-19 pandemic[J]. Case Reports In Ophthalmology,2022,13(1):96-103. [20] Liu Y,Wu B,Wang Y,et al. Clinical and multimodal imaging features of acute macular neuroretinopathy lesions following recent SARS-CoV-2 infection[J]. International Journal of Ophthalmology,2023,16(5):755-761. doi: 10.18240/ijo.2023.05.13 [21] Dinh R H,Tsui E,Wieder M S,et al. Acute macular neuroretinopathy and coronavirus disease 2019[J]. Ophthalmology. Retina,2023,7(2):198-200. doi: 10.1016/j.oret.2022.09.005 [22] Bos P J,Deutman A F. Acute macular neuroretinopathy[J]. Am J Ophthalmol,1975,80(4):573-584. doi: 10.1016/0002-9394(75)90387-6 [23] 熊淑敏, 饶杰, 程琪, 等. 新型冠状病毒感染后急性黄斑神经视网膜病变的多模影像学特征[J]. 眼科新进展,2023,43(9):712-716. doi: 10.1016/j.ajoc.2021.101232 [24] Azar G,Bonnin S,Vasseur V,et al. Did the COVID-19 pandemic increase the incidence of acute macular neuroretinopathy?[J]. J Clin Med,2021,10(21):503-508. [25] Reinhold A,Tzankov A,Matter M S,et al. Ocular pathology and occasionally detectable intraocular severe acute respiratory syndrome coronavirus-2 RNA in five fatal coronavirus disease-19 cases[J]. Ophthalmic Res,2021,64(5):785-792. doi: 10.1159/000514573 [26] Sorgeloos F, Kreit M, Hermant P, et al. Antiviral type I and type III interferon responses in the central nervous system[J]. Viruses,2013,5(3):834-857. doi: 10.3389/fncel.2021.670298 [27] Wang S,Wang J,Hu J,et al. Retinal microvascular impairment in COVID-19 patients: A meta-analysis[J]. Immun Inflamm Dis,2022,10(6):e619-e628. doi: 10.1002/iid3.619 [28] Zhang Y,Xiao M,Zhang S,et al. Coagulopathy and antiphospholipid antibodies in patients with Covid-19[J]. N Engl J Med,2020,382(17):e38-e41. [29] Nakazawa T,Kayama M,Ryu M,et al. Tumor necrosis factor-alpha mediates photoreceptor death in a rodent model of retinal detachment[J]. Invest Ophthalmol Vis Sci,2011,52(3):1384-1391. doi: 10.1167/iovs.10-6509 [30] Ashfaq I,Vrahimi M,Waugh S,et al. Acute macular neuroretinopathy associated with acute influenza virus infection[J]. Ocul Immunol Inflamm,2021,29(2):333-339. doi: 10.1080/09273948.2019.1681470 [31] Munk M R,Jampol L M,Cunha S E,et al. New associations of classic acute macular neuroretinopathy[J]. Br J Ophthalmol,2016,100(3):389-394. doi: 10.1136/bjophthalmol-2015-306845 [32] Bhavsar K,Lin S,Rahimy E,et al. Acute macular neuroretinopathy: A comprehensive review of the literature[J]. Survey of Ophthalmology,2016,61(5):538-565. doi: 10.1016/j.survophthal.2016.03.003 [33] Deschamps R,Vasseur V,Shor N,et al. A new association: Acute macular neuroretinopathy in acute optic neuritis[J]. Acta Ophthalmol,2019,97(5):e753-e756. [34] Akanda M,Gangaputra S,Kodati S,et al. Multimodal imaging in dengue-fever-associated maculopathy[J]. Ocul Immunol Inflamm,2018,26(5):671-676. doi: 10.1080/09273948.2017.1351571 [35] Fekri S, Khorshidifar M, Dehghani M S, et al. Acute macular neuroretinopathy and COVID-19 vaccination: Case report and literature review[J]. J Fr Ophtalmol,2023,46(1):72-82. [36] 陈倩,冯超逸,孙平,等. 西地那非致双眼急性黄斑神经视网膜病变1例[J]. 中国眼耳鼻喉科杂志,2021,21(5):402-404. [37] Munaut C,Lambert V,Noel A,et al. Presence of oestrogen receptor type beta in human retina[J]. Br J Ophthalmol,2001,85(7):877-882. doi: 10.1136/bjo.85.7.877 [38] Centofanti M,Bonini S,Manni G,et al. Do sex and hormonal status influence choroidal circulation?[J]. Br J Ophthalmol,2000,84(7):786-787. doi: 10.1136/bjo.84.7.786 [39] Kavroulaki D,Gugleta K,Kochkorov A,et al. Influence of gender and menopausal status on peripheral and choroidal circulation[J]. Acta Ophthalmol,2010,88(8):850-853. doi: 10.1111/j.1755-3768.2009.01607.x [40] 钟育晟,程湧,赵明威,等. 新型冠状病毒感染相关急性黄斑神经视网膜病变的临床特征[J]. 中华眼底病杂志,2023,3(39):218-222. [41] Premi E,Acampora R,Salmi D,et al. Clinical and diagnostic findings of acute macular neuroretinopathy and paracentral acute middle maculopathy in the COVID-19 era[J]. Ophthalmologica,2023,246(3-4):181-191. doi: 10.1159/000533530 [42] Leung H, Wang J, Rochtchina E, et al. Relationships between age, blood pressure, and retinal vessel diameters in an older population[J]. Invest Ophthalmol Vis Sci,2003,44(7):2900-2904. [43] 曹原,赵玥,杨婷婷,等. 新型冠状病毒相关视网膜病变多模式影像学特征观察[J]. 南京医科大学学报(自然科学版),2023,43(9):1245-1251. [44] Tang J, Li S, Wang Z, et al. Acute macular neuroretinopathy after SARS-CoV-2 infection: An analysis of clinical and multimodal imaging characteristics[J]. Diagnostics (Basel),2023,13(24):3600-3608. -





 下载:
下载: