Efficacy of Multimodal Bronchoscopic Interventions for Benign Central Airway Stenosis and Prognostic Factors: A Retrospective Cohort Study
-
摘要:
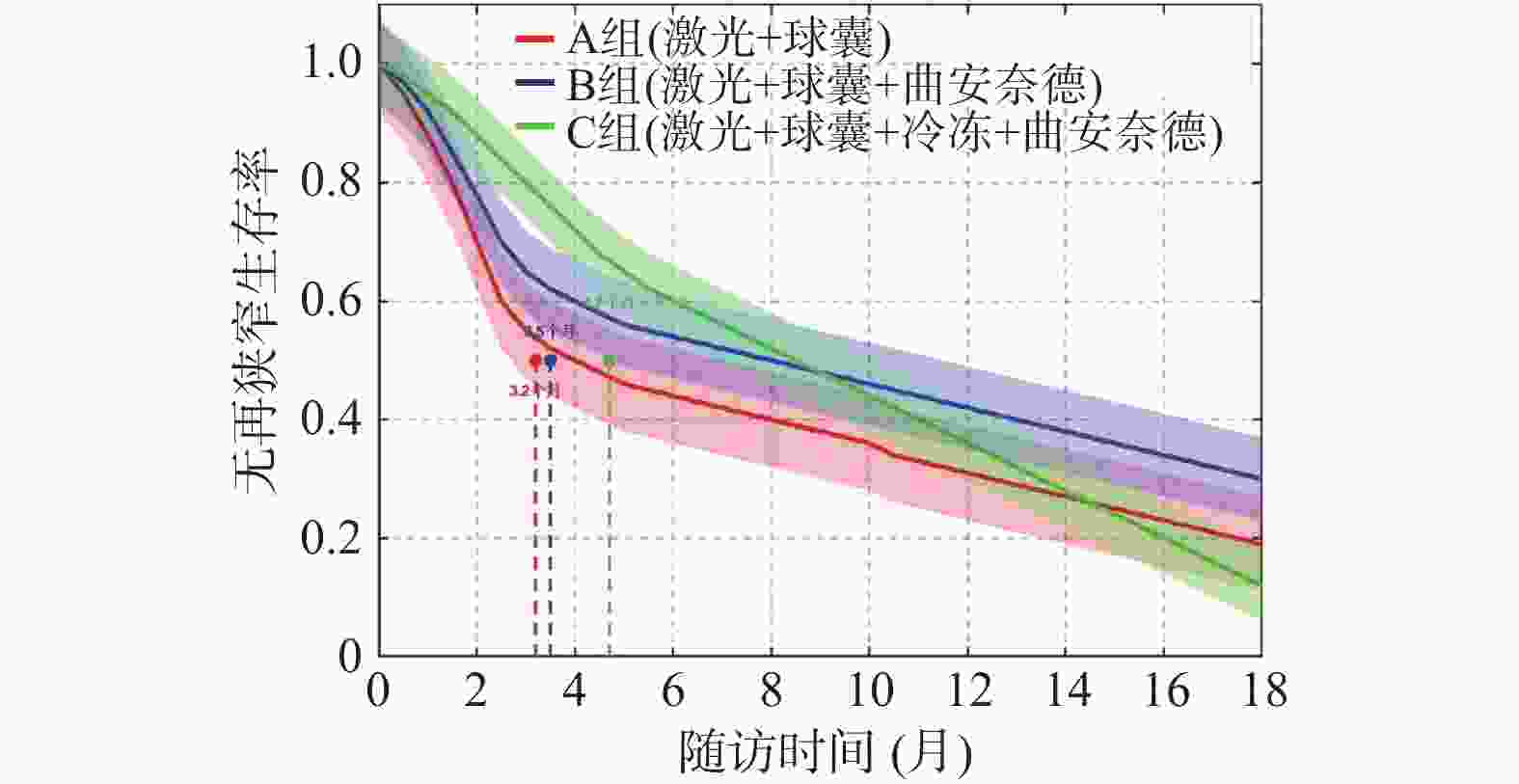
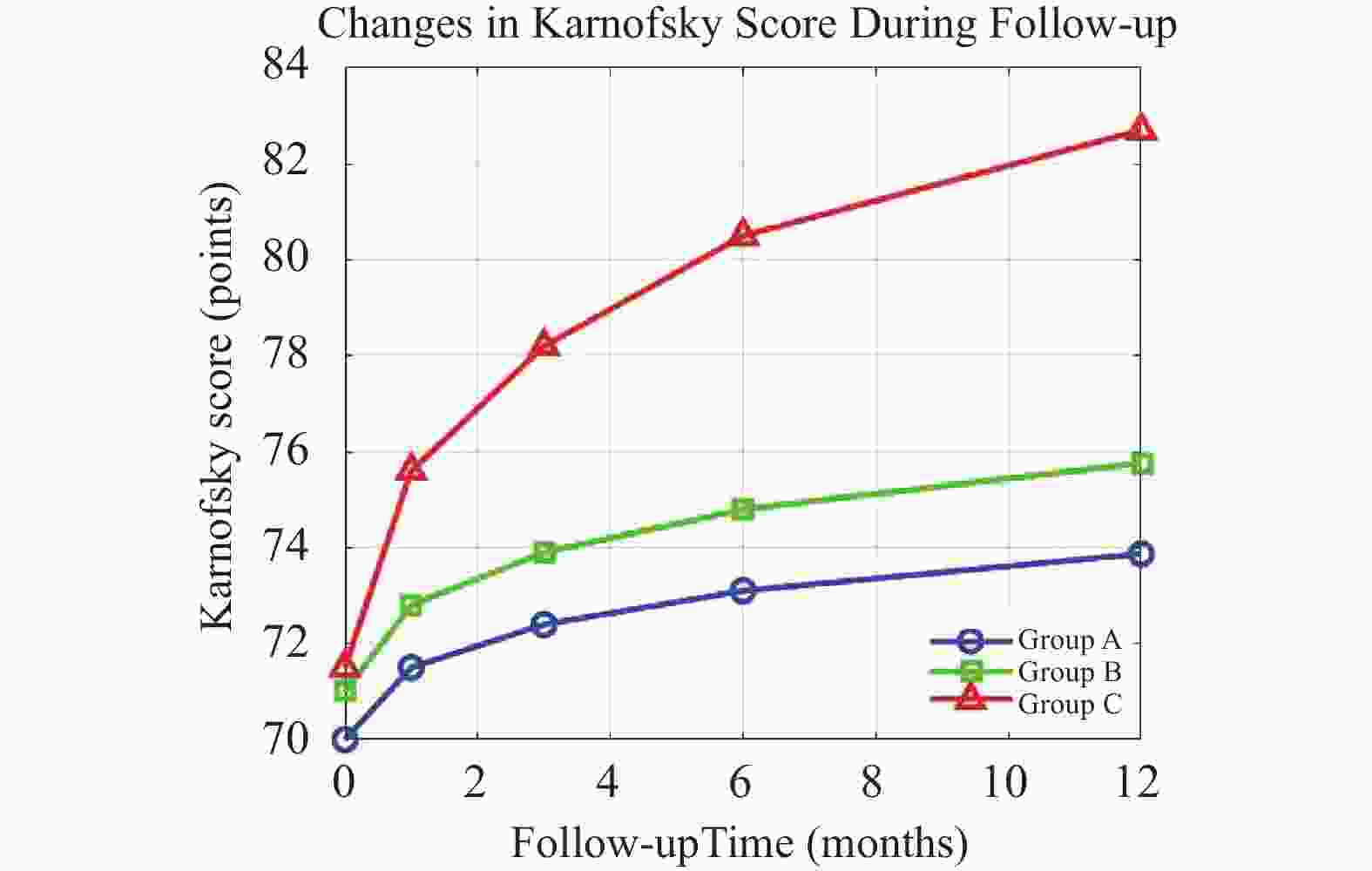
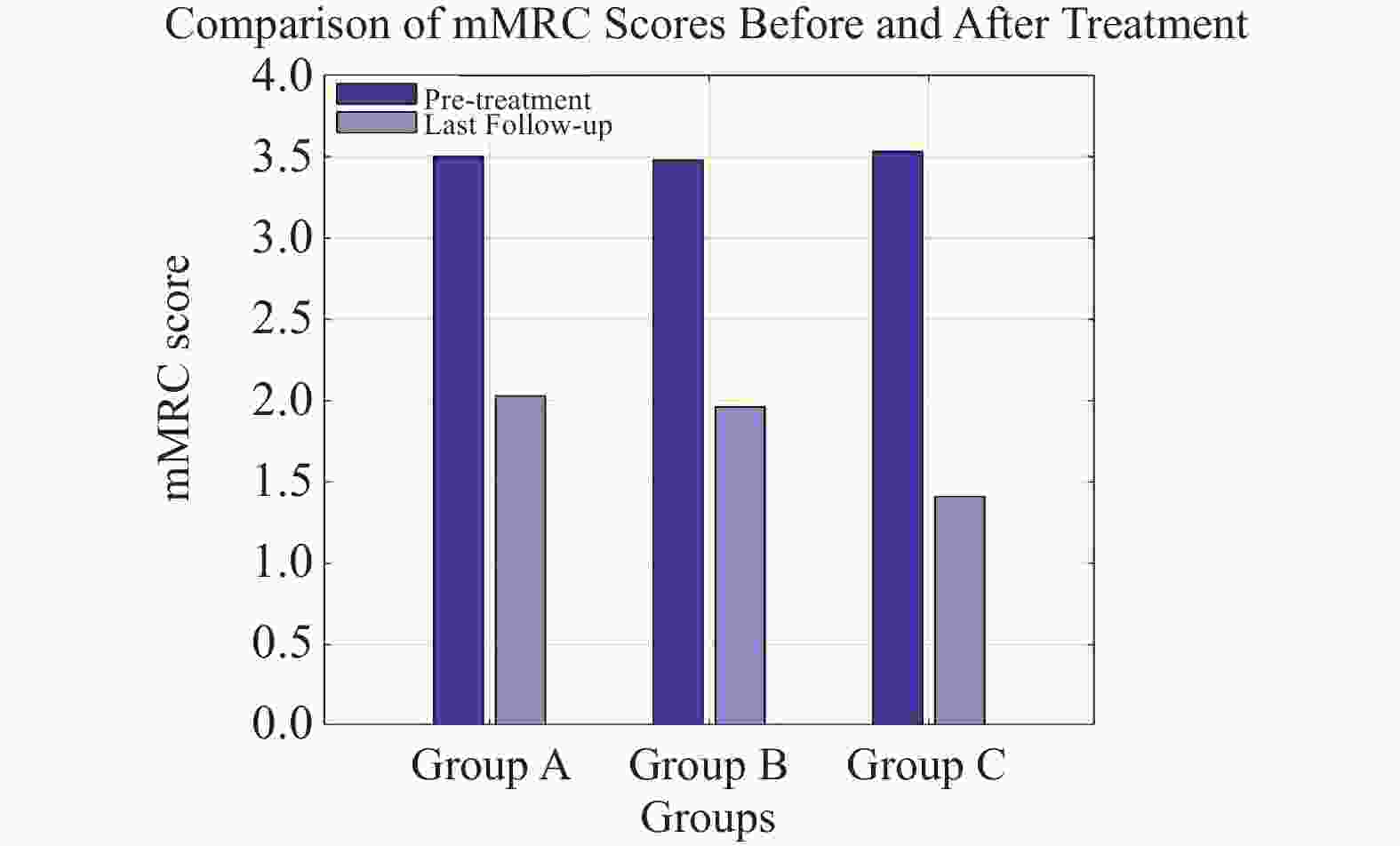
目的 比较三种气管镜介入方案治疗良性中央气道狭窄(benign central airway stenosis,BCAS)的临床疗效,明确预后影响因素。 方法 回顾性纳入昆明医科大学第一附属医院呼吸内镜中心2022年1月至2024年12月接受气管镜下介入治疗的 BCAS 患者101例,按治疗方案分为:A组(Nd:YAG 激光+球囊扩张,n = 31)、B组(Nd:YAG 激光+球囊扩张+曲安奈德,n = 33)、C组(Nd:YAG 激光+球囊扩张+曲安奈德+冷冻治疗,n = 37)。主要观察终点为治疗有效率、再狭窄相关指标(发生率及中位时间)、生活质量及并发症发生率。 结果 C组术后2个月狭窄程度分级(3.05±0.70)显著优于 A 组和B组(P = 0.002),白细胞水平下降更明显;随访12个月,C组治疗总有效率86.49%,高于A组(67.74%)和B组(69.70%)(P < 0.05),首次再狭窄中位时间(4.7 个月)较 A 组(3.2 个月)、B 组(3.5 个月)延长 47.5%(P = 0.020),第 1 秒用力呼气容积(FEV1)改善率(27.8%)及末次随访 Karnofsky 评分(82.7 分)均高于其他两组(P < 0.01)。安全性方面,三组出血发生率无显著差异,但 B组低氧血症发生率较高(21.2%)。亚组分析显示,C 组对气管插管后狭窄患者的治疗有效率(90.00%)显著高于 A 组(63.64%)和 B 组(72.73%)(P = 0.045),而对结核性狭窄患者的优势未达统计学意义(P = 0.089)。多因素 Logistic 回归分析显示,治疗方案是 BCAS 患者预后的独立影响因素(OR = 3.258,95%CI:1.563-6.794,P = 0.002)。 结论 Nd:YAG 激光+球囊扩张+曲安奈德+冷冻治疗的四联方案治疗 BCAS 疗效更优,可提升治疗有效率、延长无再狭窄时间。 Abstract:Objective To compare the clinical efficacy of three bronchoscopic interventional regimens for benign central airway stenosis (BCAS) and identify prognostic factors, so as to provide evidence-based support for individualized treatment. Methods A total of 101 BCAS patients who underwent bronchoscopic interventional therapy at the Respiratory Endoscopy Center of The First Affiliated Hospital of Kunming Medical University from January 2022 to December 2024 were retrospectively enrolled. They were divided into three groups according to the treatment regimen: Group A (Nd:YAG laser + balloon dilation, n = 31), Group B (Nd:YAG laser + balloon dilation + triamcinolone acetonide, n = 33), and Group C (Nd:YAG laser + balloon dilation + triamcinolone acetonide + cryotherapy, n = 37). The primary endpoints included treatment effective rate, restenosis-related indicators (incidence and median time), quality of life, and complication rate. Statistical analyses were performed using SPSS 26.0 and GraphPad Prism 9.0. Results At 2 months after surgery, the stenosis grade in Group C (3.05±0.70) was significantly superior to that in Groups A and B (P = 0.002), with a more obvious decrease in white blood cell count. During the 12-month follow-up, the total effective rate of Group C reached 86.49%, which was significantly higher than that of Group A (67.74%) and Group B (69.70%) (P < 0.05). The median time to first restenosis in Group C (4.7 months) was 47.5% longer than that in Group A (3.2 months) and Group B (3.5 months) (P = 0.020). Both the improvement rate of forced expiratory volume in 1 second (FEV1) (27.8%) and the Karnofsky score at the last follow-up (82.7 points) in Group C were significantly higher than those in the other two groups (P < 0.01). In terms of safety, there was no significant difference in the incidence of bleeding among the three groups, but the incidence of hypoxemia in Group B was relatively higher (21.2%). Subgroup analysis showed that the treatment effective rate of Group C in patients with post-intubation stenosis (90.00%) was significantly higher than that in Group A (63.64%) and Group B (72.73%) (P = 0.045), while the advantage in patients with tuberculous stenosis did not reach statistical significance (P = 0.089). Multivariate Logistic regression analysis revealed that the treatment regimen was an independent prognostic factor for BCAS patients (OR = 3.258, 95%CI: 1.563-6.794, P = 0.002). Conclusion The quadrature therapy regimen integrating Nd:YAG laser ablation, balloon dilation, intralesional triamcinolone acetonide injection, and cryotherapy demonstrates superior clinical efficacy in the management of benign central airway stenosis (BCAS). This multimodal approach significantly enhances the therapeutic response rate and markedly prolongs the restenosis-free interval. -
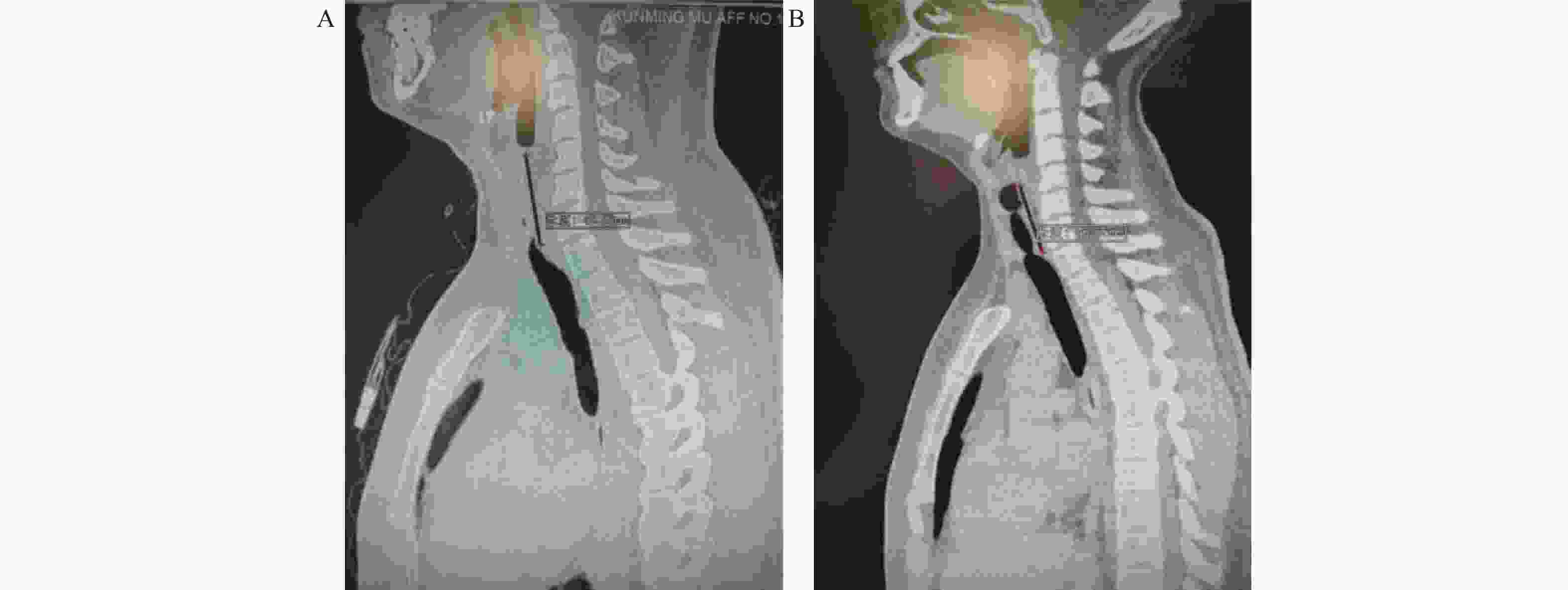
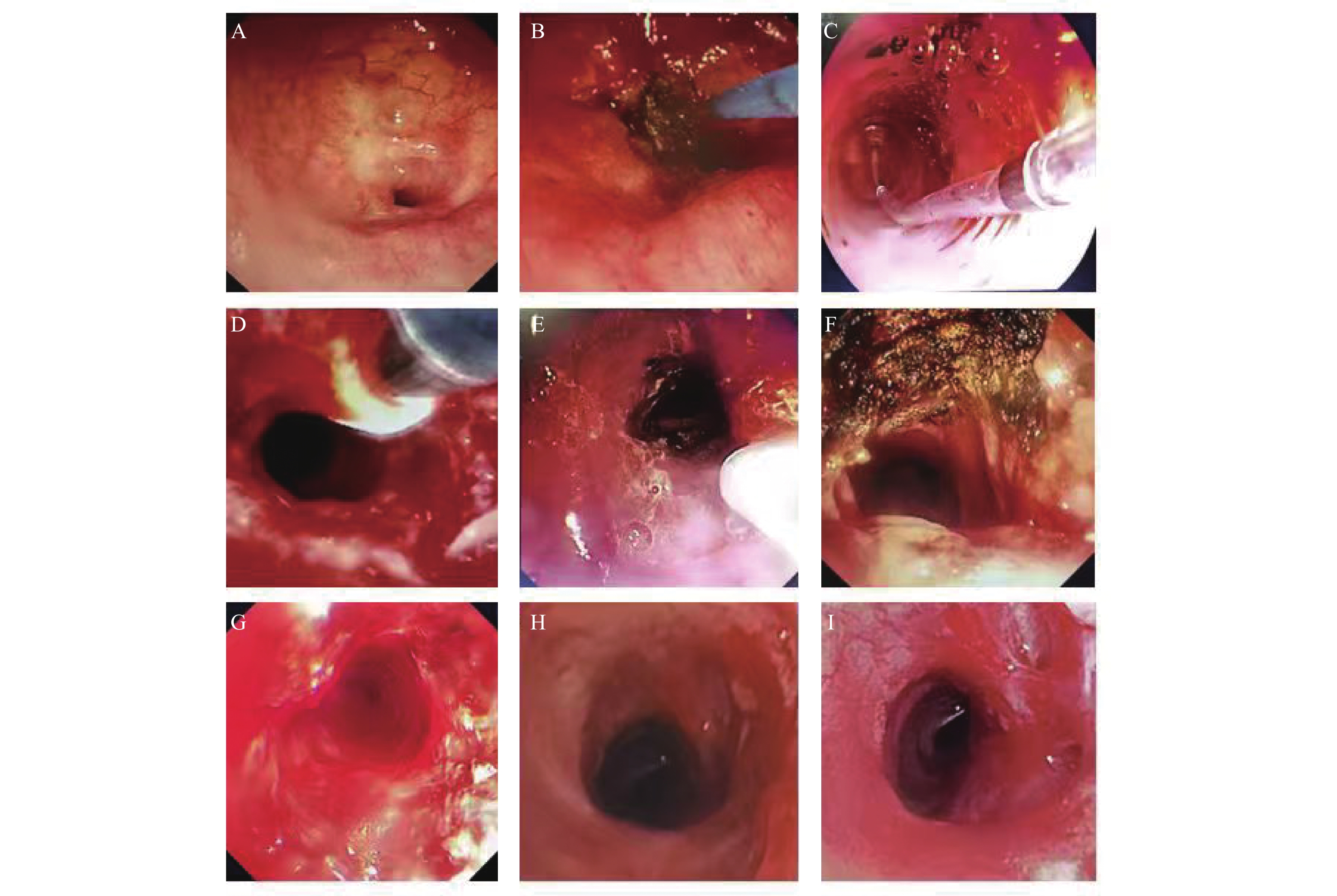
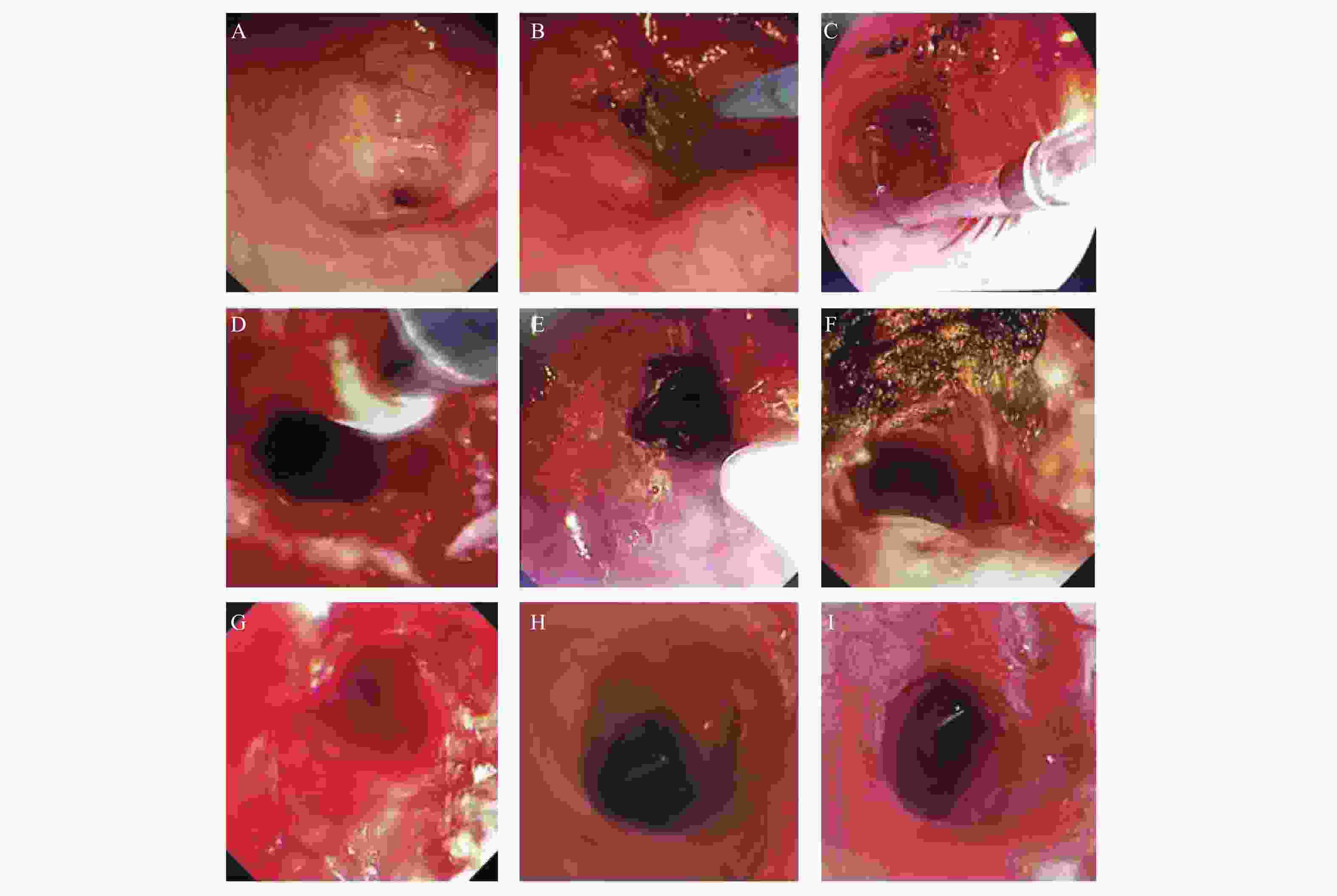
图 1 C组(激光+球囊+冷冻+曲安奈德)典型病例镜下多模式介入治疗及效果
A:C组典型病例治疗前,狭窄程度5级;B:气管镜下激光切除狭窄粘连带;C:球囊扩张狭窄部;D:冷冻治疗狭窄部;E:管腔内喷洒曲安奈德;F:多模式呼吸介入方法联合治疗完成后,狭窄程度1级;G:患者治疗7 d后复查气管镜,狭窄程度2级;H:患者治疗31 d后复查气管镜,狭窄程度3级;I:患者治疗78 d后复查气管镜,狭窄程度3级。
Figure 1. Typical case in group C: schematic illustration of microscopic multimodal interventional therapy and its therapeutic
表 1 三组患者基线特征比较(F/χ2)
Table 1. Comparison of baseline characteristics among the three patient groups (F/χ2)
变量 A(n = 31) B (n = 33) C (n = 37) F/χ2 P 人口学资料 年龄 (岁) 46.35 ± 14.07 46.52 ± 13.88 42.89 ± 16.35 0.666 0.516 性别 0.307 0.858 男 18 (58.06) 18 (54.55) 19 (51.35) 女 13 (41.94) 15 (45.45) 18 (48.65) BMI (kg/m2) 21.91 ± 2.98 22.85 ± 2.87 22.09 ± 3.31 0.784 0.460 吸烟史 0.994 0.608 有 17 (54.84) 15 (45.45) 21 (56.76) 无 14 (45.16) 18 (54.55) 16 (43.24) 合并症 糖尿病 6 (19.35) 1 (3.03) 3 (8.11) 4.978 0.083 自身免疫性疾病 3 (9.68) 2 (6.06) 2 (5.41) 0.509 0.775 狭窄病因 12.339 0.263 气管插管 11 (35.48) 11 (33.33) 20 (54.05) 结核 16 (51.61) 16 (48.48) 15 (40.54) 良性肿瘤 2 (6.45) 5 (15.15) 1 (2.70) 其他 2 (6.45) 1 (3.03) 1 (2.70) 疾病严重程度 术前狭窄程度 (级) 3.71 ± 0.69 4.06 ± 0.66 3.78 ± 0.63 2.576 0.081 术前狭窄长度 (cm) 3.65 ± 1.11 4.06 ± 1.09 3.62 ± 1.01 1.792 0.172 术前白细胞 (109/L) 6.63 ± 2.07 7.16 ± 2.25 8.04 ± 1.94 4.000 0.021* 术前血清白蛋白 (g/L) 38.65 ± 5.90 40.68 ± 5.43 38.75 ± 4.68 1.535 0.221 与激光+球囊组比较,*P < 0.05。 表 2 三组患者临床指标比较[($\bar x \pm s $)/n(%)]
Table 2. Comparison of clinical outcomes among the three patient groups [($\bar x \pm s $)/n(%)]
变量 A(n = 31) B(n = 33) C(n = 37) (χ2/F) P 治疗过程 发生手术并发症 5 (16.13) 12 (36.36) 6 (16.22) 5.148 0.076 放置支架 0 (0.00) 3 (9.09) 3 (8.11) 4.587 0.101 术后使用抗生素 12 (38.71) 15 (45.45) 11 (29.73) 1.860 0.394 术后指标 术后白细胞 (109/L) 7.45 ± 1.89 6.85 ± 1.75 6.32 ± 1.66 3.765 0.032* 治疗后复查气管镜时间间隔 (d) 58.13 ± 12.41 60.24 ± 10.43 61.35 ± 9.81 0.754 0.473 与激光+球囊组比较,*P < 0.05。 表 3 三组患者治疗效果比较[n(%)]
Table 3. Comparison of therapeutic efficacy among the three groups [n(%)]
组别 n 总有效率 χ2 P A组(激光+球囊) 31 21(67.74) 6.378 0.041* B组(激光+球囊+曲安奈德) 33 23(69.70) C组(激光+球囊+冷冻+曲安奈德) 39 32(86.49)* 与A组和B组比较,*P < 0.05。 表 4 三组患者治疗复查后狭窄程度比较($\bar x \pm s $)
Table 4. Comparison of Stenosis Severity Among Three Patient Groups at Post-treatment Follow-up ($\bar x \pm s $)
组别 n 狭窄程度(级) F P A组(激光+球囊) 31 3.68 ± 0.75 8.308 <0.001* B组(激光+球囊+曲安奈德) 33 3.64 ± 0.70 C组(激光+球囊+冷冻+曲安奈德) 37 3.05 ± 0.70 与A组和B组比较,*P < 0.01。 表 5 三组患者治疗前后主要临床指标变化比较($\bar x \pm s $)
Table 5. Comparative changes in primary clinical parameters across three patient groups pre- and post-treatment ($\bar x \pm s $)
指标 A组(n = 31) B组(n = 33) C组(n = 37) F P mMRC评分降低值(分) 1.48 ± 0.63 1.52 ± 0.62 2.11 ± 0.57 12.764 <0.001* Karnofsky评分提高值(分) 14.52 ± 5.93 15.15 ± 5.76 21.76 ± 6.35 16.233 <0.001* A组和B组比较,*P < 0.01。 表 6 影响气管镜介入治疗效果的多因素Logistic回归分析
Table 6. Multivariable logistic regression analysis of factors influencing therapeutic efficacy of bronchoscopic intervention
变量 β SE Wald χ2 P OR 95%CI 治疗方案(以A组为参照) B组 0.427 0.318 1.802 0.179 1.533 0.822-2.859 C组 1.181 0.376 9.862 0.002* 3.258 1.563-6.794 狭窄程度 −0.614 0.257 5.704 0.017* 0.541 0.327-0.895 病程时间(月) −0.203 0.086 5.577 0.018* 0.816 0.689-0.965 合并糖尿病(0=否,1=是) −0.839 0.441 3.621 0.057 0.432 0.182-1.025 合并自身免疫性疾病(0=否,1=是) −0.911 0.489 3.473 0.062 0.402 0.154-1.049 *P < 0.05。 表 7 不同病因亚组治疗总有效率比较
Table 7. Comparison of total treatment efficacy rates among different etiology subgroups
狭窄病因亚组 治疗分组 亚组内样本量(n) 总有效率(%) χ2 P 气管插管相关狭窄(n = 42) A 组 11 63.64 6.21 0.045* B 组 11 72.73 C 组 20 90.00 结核相关狭窄 (n = 47) A 组 16 68.75 4.842 0.089 B 组 16 68.75 C 组 15 86.67 *P < 0.05。 表 8 三组患者并发症发生情况及CTCAE分级
Table 8. Complication profiles and CTCAE grading across three patient groups
并发症类型 A组(n = 31) B组(n = 33) C组(n = 37) χ2 P 总并发症发生率 5(16.13) 12(36.36) 6(16.22) 5.148 0.076 出血 3(9.68) 4(12.12) 4(10.81) 0.184 0.912 低氧血症 3(9.68) 7(21.21)* 3(8.11) 6.087 0.048* −1级 2(6.45) 2(6.06) 2(5.41) 0.220 0.896 −2级 1(3.23) 4(12.12)* 1(2.70) 6.253 0.043* −≥3级 0(0.00) 1(3.03) 0(0.00) 2.525 0.109 术后感染 2(6.45) 3(9.09) 2(5.41) 1.261 0.533 气胸/纵隔气肿 0(0.00) 1(3.03) 0(0.00) 2.525 0.314 *P < 0.05 -
[1] 中华医学会呼吸病学分会. 良性气道狭窄介入诊治共识[J]. 中华结核和呼吸杂志, 2017, 40(6): 408-418. [2] 许承非, 陈逸霖, 石荟, 等. 良性气道狭窄的分子机制研究进展[J]. 中国呼吸与危重监护杂志, 2024, 23(4): 300-304. [3] Wahidi M M, Lamb C, Murgu S, et al. American Association for Bronchology and Interventional Pulmonology (AABIP) Guidelines for the Management of Benign Central Airway Stenosis[J]. Chest, 2024, 165(3): e67-e99. [4] 王德宠, 李金泉, 何元兵. 良性中央型气道狭窄介入治疗的现状与研究进展[J]. 江苏医药, 2024, 50(01): 94-97. doi: 10.19460/j.cnki.0253-3685.2024.01.021 [5] Patel A J, Budacan A M, Kumar S, et al. Management of benign airway stenosis- predictors of tracheal resection[J]. J Thorac Dis, 2024, 16(11): 7640-7650. doi: 10.21037/jtd-24-727 [6] Fiorelli A, Pecoraro A, Failla G, et al. Endoscopic management of benign airway stenosis in coronavirus disease 2019 patients[J]. Thorac Cardiovasc Surg, 2024, 72(4): 320-325. doi: 10.1055/a-2075-8109 [7] Ye Y S, Chen D F, Liu M, et al. Autologous airway basal cell transplantation alleviates airway epithelium defect in recurrent benign tracheal stenosis[J]. Stem Cells Transl Med, 2023, 12(12): 838-848. doi: 10.1093/stcltm/szad062 [8] Wei J, Qin S, Li W, et al. Analysis of clinical characteristics of 617 patients with benign airway stenosis[J]. Front Med, 2023, 10: 1202309. doi: 10.3389/fmed.2023.1202309 [9] Ravikumar N, Ho E, Wagh A, et al. The role of bronchoscopy in the multidisciplinary approach to benign tracheal stenosis[J]. J Thorac Dis, 2023, 15(7): 3998-4015. doi: 10.21037/jtd-22-1734 [10] 郑梦梦, 卢立锦, 周知, 等. 1 例良性气道狭窄病人行气管硬镜下硅酮支架植入术的护理[J]. 循证护理, 2024, 10(12): 2278-2280. [11] 苏江, 翁涛平, 张先明. 硅酮支架治疗三种常见良性中心气道狭窄的对照研究 [J]. 中国呼吸与危重监护杂志, 2024, 23 (4): 231-236. [12] Ratwani A P, Lentz R J, Chen H, et al. Spray cryotherapy for benign large airway stenosis: A multicenter retrospective cohort study of safety and practice patterns[J]. J Bronchol Interv Pulmonol, 2024, 31(1): 63-69. doi: 10.1097/LBR.0000000000000930 [13] Rusakov M A, Parshin V D, Simonova M S, et al. Airway stenting in patients with complex benign tracheobronchial stenosis[J]. Khirurgiia (Mosk), 2022(11): 5-12. [14] Fiorelli A, Messina G, Bove M, et al. Ultrasound for assessment and follow-up of airway stenosis[J]. Ann Thorac Surg, 2022, 113(5): 1624-1633. doi: 10.1016/j.athoracsur.2021.05.056 [15] Wei J, Chen Y, Feng T, et al. miR-34c-5p inhibited fibroblast proliferation, differentiation and epithelial-mesenchymal transition in benign airway stenosis via MDMX/p53 pathway[J]. Funct Integr Genom, 2024, 24(2): 37. doi: 10.1007/s10142-024-01317-y [16] Cheng Z, Chen Z, Yang S, et al. Comparison of clinical efficacy of different bronchoscopic interventions in benign airway stenosis: a systematic review and network meta-analysis. Journal of Thoracic Disease, 2021, 13(11): 6411-6423. [17] Bertino G, Pedretti F, Mauramati S, et al. Recurrent laryngeal papillomatosis: multimodal therapeutic strategies. Literature review and multicentre retrospective study[J]. Acta Otorhinolaryngol Ital., 2023, 43(Suppl 1): S111-S122. [18] Wang R, Cheng J, Zhang Y, et al. Analysis of risk factors for benign central airway stenosis after COVID-19 infection[J]. Eur J Med Res, 2024, 29(1): 624. doi: 10.1186/s40001-024-02216-5 [19] Ratwani A P, Lentz R J, Chen H, et al. Spray Cryotherapy for Benign Large Airway Stenosis: A Multicenter Retrospective Cohort Study of Safety and Practice Patterns[J]. J Bronchology Interv Pulmonol, 2024, 31(1): 63-69. [20] He J, Yu M, Li X, et al. Local Triamcinolone Acetonide Injection Combined with Conventional Interventional Methods in the Treatment of Benign Central Airway Stenosis: A Meta-analysis of Efficacy and Safety[J]. Journal of Thoracic Disease, 2021, 20(10): 726-733. [21] Lei X, Meng Y, Wang X, et al. The Role of Local Steroid Therapy in the Management of Benign Airway Stenosis: A Systematic Review and Meta-analysis[J]. Respiratory Research, 2021, 22(1): 282. doi: 10.1186/s12931-021-01879-6 [22] Emam W, Mostafa Y, Madkour A, Elgazzar T, Shehata M, Elbadrawy R, et al. Bronchoscopic management as an alternative treatment in non-operable benign tracheal stenosis. Int J Clin Pract. 2021;75(5): e14058. [23] Natale G, Reginelli A, Testa D, et al. The use of 3D printing model as tool for planning endoscopic treatment of benign airway stenosis[J]. Transl Cancer Res TCR, 2020, 9(3): 2117-2122. doi: 10.21037/tcr.2020.01.22 [24] GOLD Science Committee. Global Strategy for the Prevention, Diagnosis and Management of Chronic Obstructive Pulmonary Disease: 2025 Report - Executive Summary[J]. Am J Respir Crit Care Med, 2025, 211: 1-20. [25] Howdon D, van den Hout W, van der Linden Y, et al. Replacing performance status with a simple patient-reported outcome in palliative radiotherapy prognostic modelling[J]. Clin Transl Radiat Oncol, 2022, 37: 137-144. doi: 10.1002/1097-0142(19800415)45:8<2220::AID-CNCR2820450835>3.0.CO;2-Q [26] Mehta V, Gerchman L, Hacht JL, et al. Balloon bronchoplasty for benign airway strictures: systematic review and meta-analysis. Eur Respir J. 2023;61(2): 2201237. [27] Batra H, Yarmus L. Indications and complications of rigid bronchoscopy[J]. Expert Rev Respir Med, 2018, 12(6): 509-520. doi: 10.1080/17476348.2018.1473037 [28] Fiorelli A, Messina G, Santoriello C, et al. Endobronchial ultrasound for benign tracheal stenosis[J]. Thorac Cardiovasc Surg, 2019, 67(3): 232-234. doi: 10.1055/s-0038-1668597 [29] Bilaçeroğlu S, Aydoğdu Z, Takiguchi Y. Updates in Interventional Bronchoscopy for Benign Central Airway Obstruction[J]. Journal of Clinical Medicine, 2021, 10(17): 3940. doi: 10.3390/jcm10173940 [30] Verret D J, Chakraborty R K, Bailey L S, et al. Advanced Laser Techniques for Endoscopic Treatment of Benign Tracheal Stenosis: Long - Term Outcomes[J]. Otolaryngology - Head and Neck Surgery, 2022, 166(4): 762-769. [31] Russo E, Guarino E, Lopez C, et al. Benign airway stenosis: modern technological interventions. ERJ Open Res. 2022;8(4)00651-2022. [32] Oh D K, Kim S H, Koo H K, et al. Airway remodeling differences in post-tuberculosis and post-intubation tracheal stenosis: a prospective observational study. Scientific Reports, 2022, 12(1): 13546. [33] Akulian J A, Yarmus L, Wahidi M M, et al. Interventional Pulmonology: An Official American Thoracic Society/American College of Chest Physicians Clinical Practice Guideline. Chest. 2022;162(6): e363-e381. [34] Murgu S D, Colt H G. Airway Stenosis: Functional Classification and Interventional Bronchoscopy[J]. Eur Respir J, 2021, 58: 2100756. [35] Marwah V, Bhardwaj B, Vadlamudi KV, et al. Holistic approach to management of benign tracheobronchial stenosis: A retrospective single-center experience. Lung India, 2022, 39(3): 226-231. [36] Dutau H, Breen D P, Gomez C, et al. The integrated therapeutic bronchoscopy management of benign complex tracheobronchial stenosis: A pooled analysis. Respiratory Medicine, 2021, 176: 106280. [37] Kenn K, Foerster M, Hupertz S, et al. Clinical outcomes and follow-up approach in patients treated with multimodal bronchoscopic intervention for benign airway stenosis. Therapeutic Advances in Respiratory Disease, 2022, 16: 17534666221112403. [38] Qiu X, Liu Y, Zhang J, et al. Paclitaxel-loaded PLGA coating stents in the treatment of benign cicatricial airway stenosis[J]. J Clin Med, 2022, 11(3): 517. doi: 10.3390/jcm11030517 -





 下载:
下载: