Predictive Evaluation and Risk Factor Analysis of Delirium in Elderly Patients with Frailty Using FRAIL, CFS, and REFS
-
摘要:
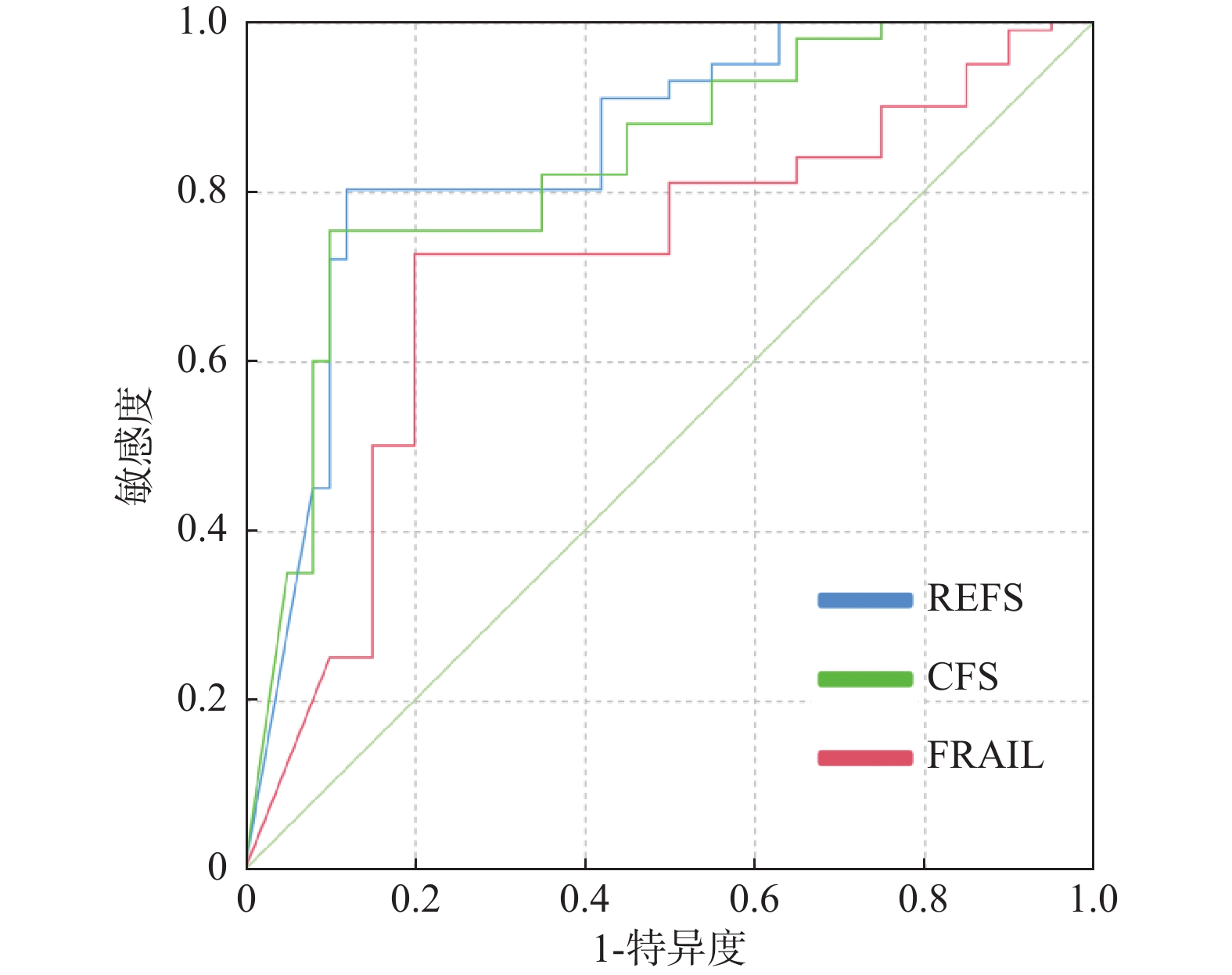
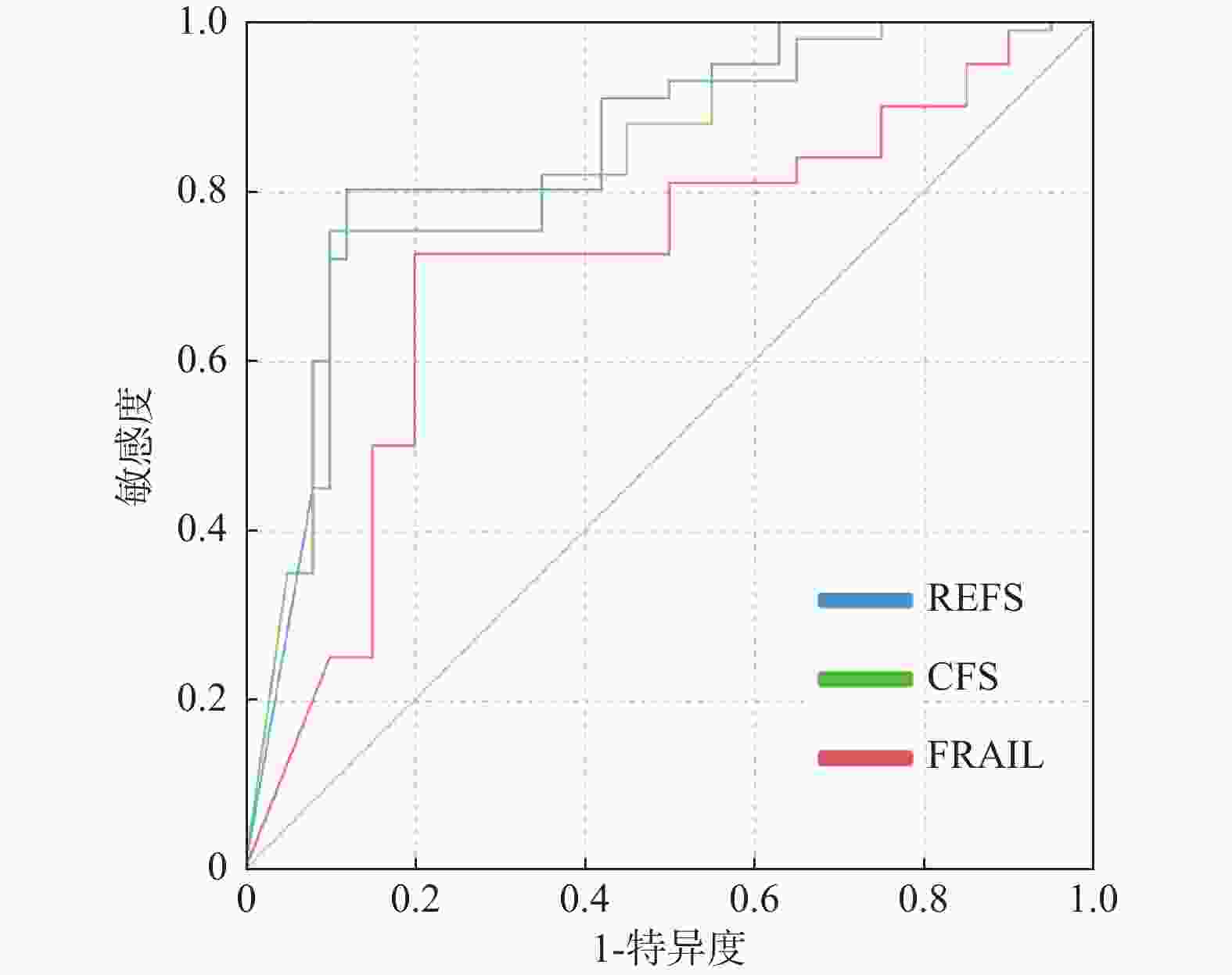
目的 探析衰弱筛查量表(frail scale,FRAIL)、临床衰弱量表(clinical frailty scale,CFS)、自我报告埃德蒙顿衰弱量表(reported edmonton frail scale,REFS)对老年衰弱患者谵妄的预测评估及风险因素分析。 方法 选择成都市第六人民医院2023年1月至12月老年医学科收治的187例老年衰弱住院患者作为研究对象。采用 FRAIL、CFS、REFS量表评估衰弱指数,收集患者各项资料资料并构建谵妄相关风险队列。记录谵妄发生率、发生持续时间及预后结局;分析发生与未发生谵妄患者的FRAIL、CFS、REFS量表;对比发生与未发生谵妄患者临床特征;采用Logistic回归分析老年衰弱患者发生谵妄的风险因素,ROC曲线分析FRAIL、CFS、REFS对老年衰弱患者谵妄发生的预测效能。 结果 187例老年衰弱住院患者中发生谵妄34例(18.18%),未发生谵妄153例(81.82%)。发生谵妄组患者FRAIL、CFS、REFS量表评分均高于未发生组(P < 0.05)。两组患者年龄、中风、营养不良、认知障碍、活动受限、重度疼痛特征对比有差异(P < 0.05)。Logistic结果显示,年龄≥75岁、中风、营养不良、认知障碍、活动受限、重度疼痛、FRAIL、CFS、REFS均为老年衰弱患者发生谵妄风险因素(P < 0.05)。ROC曲线显示,REFS对老年衰弱患者谵妄发生的ROC曲线下面积为0.813(0.739~0.843)较FRAIL、CFS更高。 结论 老年衰弱患者发生谵妄影响因素主要与年龄≥75岁、中风、营养不良、认知障碍、活动受限、重度疼痛、衰弱程度有关,且相较于FRAIL、CFS量表,REFS量表预测谵妄效能更高。 Abstract:Objective To explore the predictive assessment and risk factor analysis of the FRAIL Scale (Frailty), Clinical Frailty Scale (CFS), and Reported Edmonton Frail Scale (REFS) for delirium in elderly frail patients. Methods A total of 187 elderly frail hospitalized patients admitted to the Department of Geriatric Medicine at Chengdu Sixth People's Hospital from January to December 2023 were selected as research subjects. The FRAIL, CFS, and REFS scales were used to assess the frailty index. Patient data were collected and a delirium-related risk cohort was constructed. The incidence of delirium, duration of occurrence, and prognostic outcomes were recorded. The FRAIL, CFS, and REFS scale scores between patients with and without delirium were analyzed. Clinical characteristics were compared between the two groups. Logistic regression analysis was used to identify risk factors for delirium in elderly frail patients, and ROC curve analysis was performed to evaluate the predictive efficacy of FRAIL, CFS, and REFS for delirium occurrence in elderly frail patients. Results Among the 187 elderly frail hospitalized patients, 34 cases (18.18%) developed delirium, and 153 cases (81.82%) did not develop delirium. The FRAIL, CFS, and REFS scale scores in the delirium group were significantly higher than in the non-delirium group (P < 0.05). There were significant differences between the two groups in age, stroke history, malnutrition, cognitive impairment, activity limitation, and severe pain (P < 0.05). Logistic regression results showed that age ≥75 years, stroke, malnutrition, cognitive impairment, activity limitation, severe pain, FRAIL, CFS, and REFS were all risk factors for delirium in elderly frail patients (P < 0.05). ROC curve analysis demonstrated that REFS had a higher area under the ROC curve (AUC = 0.813, 95%CI: 0.739-0.843) for predicting delirium in elderly frail patients compared to FRAIL and CFS. Conclusions The main factors affecting delirium occurrence in elderly frail patients are related to age ≥75 years, stroke, malnutrition, cognitive impairment, activity limitation, severe pain, and degree of frailty. The REFS scale demonstrates superior predictive efficacy for delirium compared to the FRAIL and CFS scales. -
Key words:
- Elderly frailty /
- Delirium /
- FRAIL scale /
- CFS /
- REFS /
- Risk factor
-
表 1 分析发生与未发生谵妄患者的FRAIL、CFS、REFS量表($ \bar x \pm s $,分)
Table 1. Analysis of FRAIL,CFS,and REFS scales in patients with and without delirium ($ \bar x \pm s $,points)
组别 n FRAIL CFS REFS 发生组 34 4.67 ± 0.32 6.82 ± 0.59 14.32 ± 2.67 未发生组 153 3.52 ± 0.24 5.34 ± 0.27 8.84 ± 0.35 t - 23.683 22.349 24.673 P - <0.001* <0.001* <0.001* *P < 0.05。 表 2 对比发生与未发生谵妄患者临床特征
Table 2. Comparison of clinical characteristics between patients with and without delirium
特征 发生组(n =34) 未发生组(n =153) χ2 P 性别 0.097 0.756 男 19(55.88) 81(52.94) 女 15(44.12) 72(47.06) 年龄(岁) 5.659 0.017* 65~74 11(32.35) 84(54.90) ≥75 23(67.65) 69(45.10) 婚姻状态 0.401 0.526 已婚 25(73.53) 104(67.97) 丧偶/离异 9(26.47) 49(32.03) 文化状态 3.168 0.205 文盲 7(20.59) 28(18.30) 小学 12(35.29) 34(22.22) 中学及以上 15(44.12) 91(59.48) 吸烟史 10(29.41) 37(24.18) 0.404 0.525 饮酒史 11(32.35) 35(22.88) 1.347 0.246 慢性病 高血压 15(44.12) 64(41.83) 0.060 0.807 冠心病 10(29.41) 32(20.92) 1.153 0.283 2型糖尿病 12(35.29) 59(38.56) 0.126 0.722 慢性阻塞性肺病 7(20.59) 21(13.73) 1.029 0.310 中风 13(38.24) 18(11.76) 14.095 <0.001* 骨关节炎 6(17.65) 29(18.95) 0.031 0.860 营养不良 15(44.12) 26(16.99) 11.956 <0.001* 认知障碍 17(50.00) 23(15.03) 20.228 <0.001* 存在抑郁 17(50.00) 56(36.60) 2.099 0.147 存在焦虑 15(44.17) 48(31.37) 2.023 0.155 活动受限 24(70.59) 32(20.92) 32.719 <0.001* 重度疼痛 20(58.82) 41(26.80) 12.981 <0.001* 睡眠障碍 10(29.41) 32(20.92) 1.153 0.283 镇静药物使用 10(29.41) 34(22.22) 0.799 0.371 抗胆碱能药物使用 7(20.59) 28(18.30) 0.096 0.757 *P < 0.05。 表 3 分析老年衰弱患者发生谵妄的风险因素
Table 3. Analysis of risk factors for delirium in elderly patients with frailty
指标 调整前 调整后 β S.E. Waldχ2 OR(95%CI) P β S.E. Waldχ2 OR(95%CI) P 年龄(≥75岁) 0.400 0.335 4.899 1.431(0.941~2.262) 0.024* 0.377 0.223 4.274 1.394 (0.915~1.789) 0.028* 中风 0.537 0.423 5.187 1.589(1.108~2.937) 0.015* 0.408 0.331 4.863 1.517 (1.096~1.891) 0.019* 营养不良 0.515 0.420 5.008 1.518(1.083~1.905) 0.020* 0.385 0.329 4.717 1.435 (1.077~1.923) 0.023* 认知障碍 0.771 0.579 8.985 2.143(1.360~3.227) 0.000* 0.598 0.468 7.592 1.915 (1.252~3.107) 0.000* 活动受限 0.654 0.547 7.910 1.804(1.175~2.833) 0.005* 0.527 0.435 7.384 1.731 (1.047~2.326) 0.007* 重度疼痛 0.612 0.513 7.382 1.715(1.296~2.856) 0.008* 0.506 0.409 7.012 1.622 (1.245~2.783) 0.010* 注:调整后的调整因素主要为年龄、营养不良、认知障碍;*P < 0.05。 表 4 分析三个量表对老年衰弱患者发生谵妄的影响
Table 4. Analysis of the impact of three scales on delirium in elderly patients with frailty
指标 调整前 调整后 β S.E. Waldχ2 OR(95%CI) P β S.E. Waldχ2 OR(95%CI) P FRAIL 0.627 0.521 7.463 1.726(1.347~2.113) 0.007* 0.544 0.385 6.952 1.626 (1.005~2.645) 0.009* CFS 0.632 0.534 7.589 1.763(0.947~2.135) 0.006* 0.510 0.371 6.748 1.592 (0.946~2.683) 0.011* REFS 0.714 0.556 8.134 1.834(1.058~1.872) 0.002* 0.589 0.427 7.851 1.753 (1.032~2.987) 0.004* 注:调整后的调整因素主要为年龄、营养不良、认知障碍;*P < 0.05。 表 5 分析FRAIL、CFS、REFS对老年衰弱患者谵妄发生的预测效能
Table 5. Analysis of the predictive efficacy of FRAIL,CFS,and REFS for delirium occurrence in elderly patients with frailty
指标 AUC(95%CI) P cut-off值 敏感度(%) 特异度(%) 约登指数 FRAIL 0.713(0.695~0.796) 0.023* 4.14分 72.58 70.36 0.43 CFS 0.752(0.721~0.806) 0.012* 6.23分 75.34 72.14 0.47 REFS 0.813(0.739~0.843) 0.001* 12.57分 80.23 74.52 0.55 *P < 0.05。 -
[1] 曹成霖, 吴新春, 纪凯, 等. 老年衰弱研究进展[J]. 中国临床保健杂志, 2023, 26(2): 274-278. doi: 10.12114/j.issn.1007-9572.2023.0719 [2] 石婧, 石冰, 陶永康, 等. 基于衰弱指数评估的老年人衰弱状况与死亡风险的相关性分析[J]. 中华流行病学杂志, 2020, 41(11): 1824-1830. doi: 10.3760/cma.j.cn112338-20200506-00691 [3] 许丽, 张蒙, 韦靖怡, 等. 预防住院老年病人发生谵妄照护方案实施及效果评价[J]. 实用老年医学, 2023, 37(2): 204-208. [4] 陈敏, 宋清扬, 王爽, 等. 老年住院患者衰弱指数与谵妄的相关性研究[J]. 国际精神病学杂志, 2022, 49(2): 259-262+266. [5] 鲁云竹, 郭松青, 陈鑫, 等. 心脏手术衰弱老年患者术后谵妄的危险因素及其预测模型的建立[J]. 中华麻醉学杂志, 2022(11): 1316-1319. [6] 秦兰芳, 郭文熙, 王瑞, 等. 骨科住院老年患者衰弱评估工具的范围综述[J]. 中国全科医学, 2023, 26(23): 2864-2870. doi: 10.12114/j.issn.1007-9572.2022.0866 [7] 中华医学会老年医学分会. 老年人运动能力下降多学科决策模式中国专家共识(2024版)[J]. 中华医学杂志, 2024, 104(12): 893-905. doi: 10.3760/cma.j.cn112137-20230816-00238 [8] 中华医学会老年医学分会. 老年患者术后谵妄防治中国专家共识[J]. 中华老年医学杂志, 2016, 35(12): 1257-1262. doi: 10.3760/cma.j.cn321761-20220915-10005 [9] 高浪丽, 冯冬梅, 王荣海, 等. 意识模糊评估法简短量表的汉化及用于老年谵妄的信度和效度研究[J]. 实用老年医学, 2019, 33(2): 133-136. [10] Thompson M Q, Theou O, Tucker G R, et al. FRAIL scale: Predictive validity and diagnostic test accuracy[J]. Australas J Ageing, 2020, 39(4): e529-e536. [11] Fehlmann C A, Nickel C H, Cino E, et al. Frailty assessment in emergency medicine using the Clinical Frailty Scale: A scoping review[J]. Intern Emerg Med, 2022, 17(8): 2407-2418. doi: 10.1007/s11739-022-03042-5 [12] Roopsawang I, Thompson H, Zaslavsky O, et al. The reported Edmonton frail scale-Thai version: Development and validation of a culturally-sensitive instrument[J]. Nurs Health Sci, 2020, 22(3): 685-693. doi: 10.1111/nhs.12713 [13] Hersberger L, Bargetzi L, Bargetzi A, et al. Nutritional risk screening (NRS 2002) is a strong and modifiable predictor risk score for short-term and long-term clinical outcomes: Secondary analysis of a prospective randomised trial[J]. Clin Nutr, 2020, 39(9): 2720-2729. doi: 10.1016/j.clnu.2019.11.041 [14] Schönstein A, Wahl H W, Katus H A, et al. SPMSQ for risk stratification of older patients in the emergency department: An exploratory prospective cohort study[J]. Z Gerontol Geriatr, 2019, 52(Suppl 4): 222-228. [15] Costantini L, Pasquarella C, Odone A, et al. Screening for depression in primary care with Patient Health Questionnaire-9 (PHQ-9): A systematic review[J]. J Affect Disord, 2021, 279: 473-483. doi: 10.1016/j.jad.2020.09.131 [16] Toussaint A, Hüsing P, Gumz A, et al. Sensitivity to change and minimal clinically important difference of the 7-item Generalized Anxiety Disorder Questionnaire (GAD-7)[J]. J Affect Disord, 2020, 265: 395-401. doi: 10.1016/j.jad.2020.01.032 [17] Bouwstra H, Smit E B, Wattel E M, et al. Measurement properties of the Barthel index in geriatric rehabilitation[J]. J Am Med Dir Assoc, 2019, 20(4): 420-425. e1. [18] Bielewicz J, Daniluk B, Kamieniak P. VAS and NRS, same or different? Are visual analog scale values and numerical rating scale equally viable tools for assessing patients after microdiscectomy?[J]. Pain Res Manag, 2022, 2022: 5337483. doi: 10.1155/2022/5337483 [19] Okajima I, Miyamoto T, Ubara A, et al. Evaluation of severity levels of the Athens insomnia scale based on the criterion of insomnia severity index[J]. Int J Environ Res Public Health, 2020, 17(23): 8789. doi: 10.3390/ijerph17238789 [20] 陶二存, 刘琴, 杨昌龙, 等. 改良衰弱指数与睡眠质量预测老年患者术后谵妄发生的价值[J]. 国际精神病学杂志, 2024, 51(2): 571-575. doi: 10.13479/j.cnki.jip.2024.02.036 [21] 张真真, 周晓艳, 曹林, 等. 术前衰弱对行膝髋关节置换手术老年患者术后谵妄的影响[J]. 医学研究生学报, 2021, 34(4): 371-374. doi: 10.16571/j.cnki.1008-8199.2021.04.007 [22] 王佳, 孙莹, 王春玲, 等. 骨科老年手术患者老年综合征情况及术后并发症的影响因素分析[J]. 中华全科医师杂志, 2023, 22(10): 1068-1072. doi: 10.3760/cma.j.cn114798-20230726-00707 [23] 杨梦娇, 高梅. 三种衰弱评估方法对老年骨科患者术后谵妄的预测作用[J]. 国际老年医学杂志, 2023, 44(5): 548-555. doi: 10.3969/j.issn.1674-7593.2023.05.007 -





 下载:
下载: