Studies on the Correlation between Esophageal Manometry and Short-Term Efficacy of Endoscopic Myomectomy in Patients with Achalasia
-
摘要:
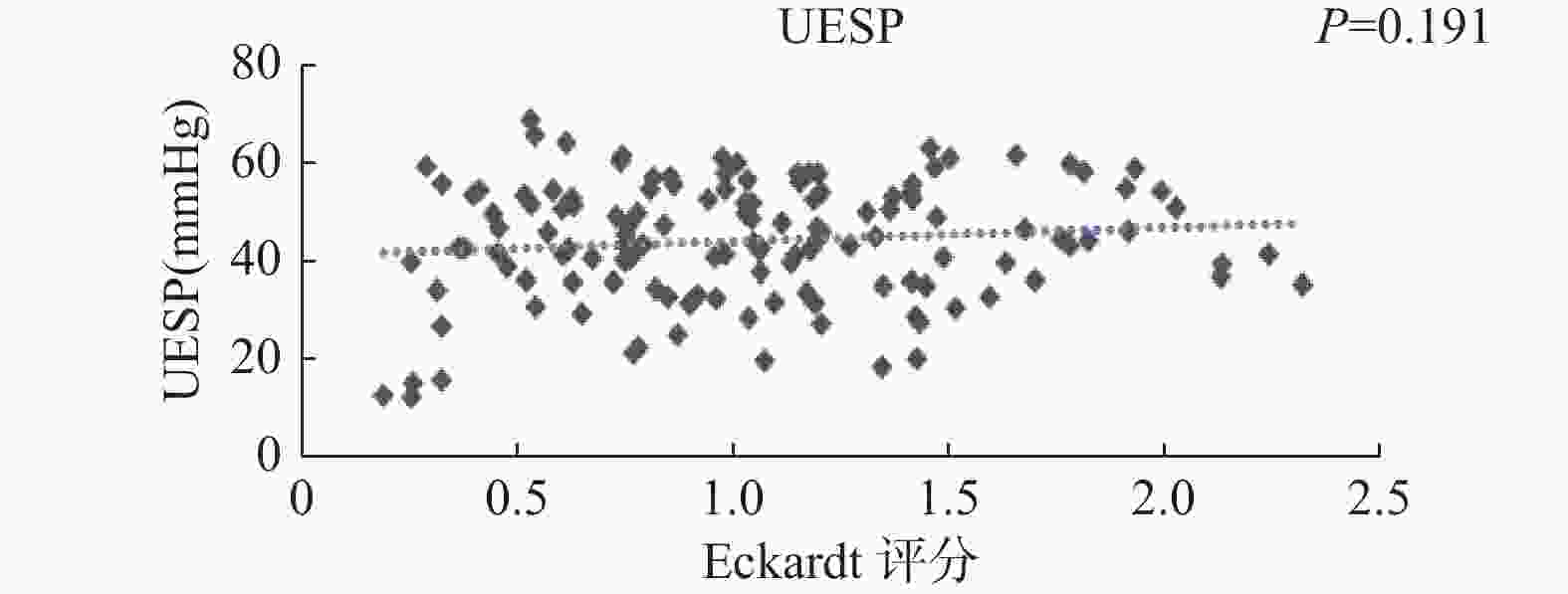
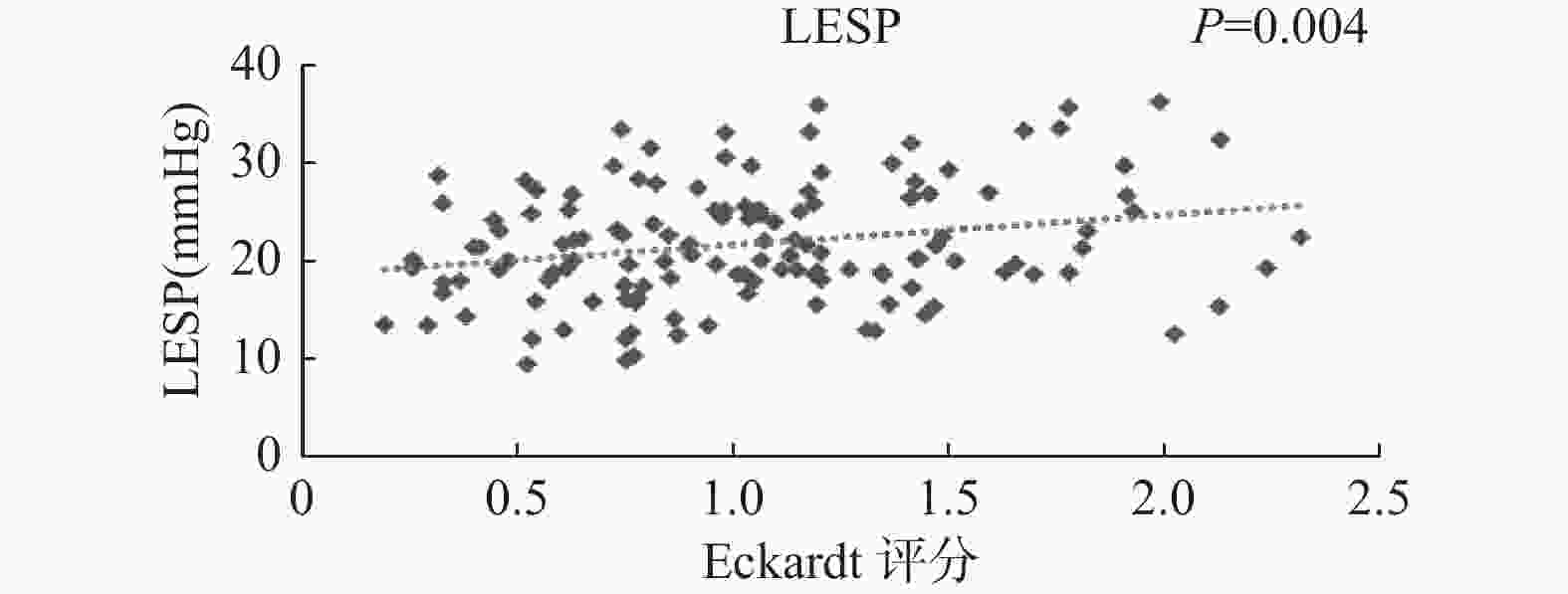
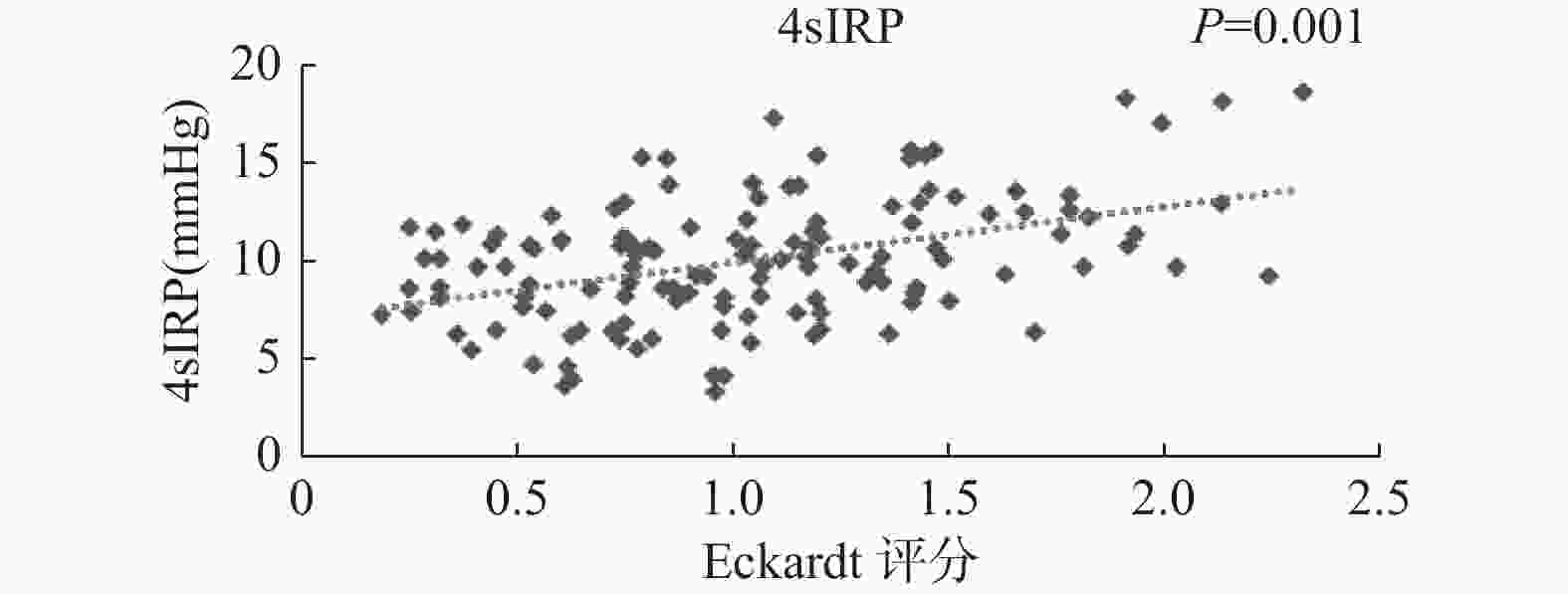
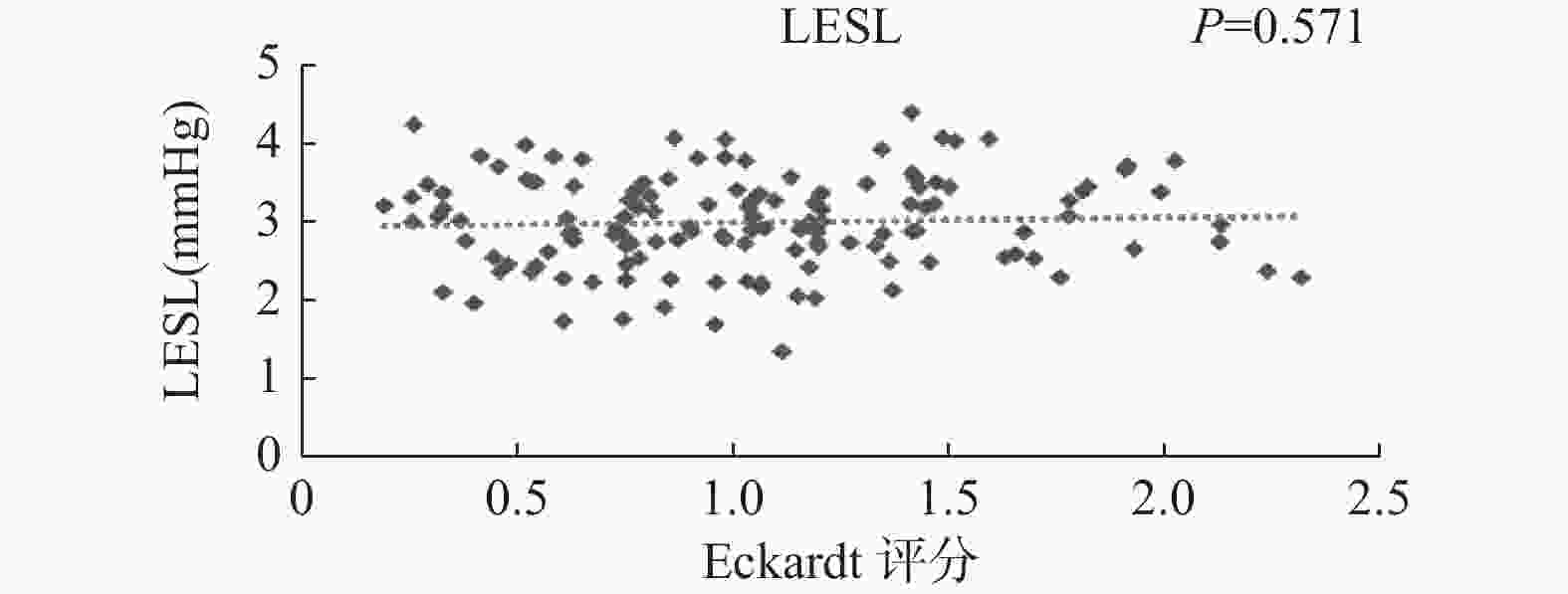
目的 探讨贲门失迟缓症患者食管测压与经口内镜下肌切开术短期疗效的相关性。 方法 选取2019年01月至2024年09月在苏州大学附属第一医院消化科首次行POEM治疗的272例AC患者的临床资料。依据2020年芝加哥4.0分型和Ling分型进行分组。分析所有患者的基线资料和手术缓解率,比较不同分组患者的Eckardt评分和食管测压数据,并分析食管测压数据和术后临床疗效的相关性。 结果 (1)本研究共纳入272例患者,手术成功率为100%。272例患者的术前Eckardt评分(6.65±1.48)分,术后3个月后的Eckardt评分为(1.05±0.56)分,272例患者POEM术后的Eckardt评分较术前显著下降,差异有统计学意义(t = 19.823,P < 0.001)。芝加哥分型三组患者及Ling分型五组患者的术后Eckardt评分均显著低于术前,差异比较均有统计学意义(P均 < 0.05);(2)芝加哥分型三组患者的术后LESP及4sIRP均较术前显著降低,差异均有统计学意义(P均 < 0.05)。且三组患者术后的LESP及4sIRP比较差异也有统计学意义(P < 0.05);进一步采用Bonferroni法进行两两比较显示II组的LESP及4sIRP均低于I组和III组(P均 < 0.05),但I组和III组间比较差异无统计学意义(P均 > 0.05)。Ling分型五组患者的术后五组患者的术后LESP及4sIRP也均低于术前,均有统计学意义(P均 < 0.05)。五组患者术后的LESP及4sIRP比较差异也有统计学意义(P < 0.05);进一步采用Bonferroni法进行两两比较显示IIa组、IIb组、IIc组及III组的LESP和4sIRP均显著低于I组(P均 < 0.05),但IIa组、IIb组、IIc组及III组两两之间差异无统计学意义(P均 > 0.05);(3)4sIRP和Eckardt评分的严重程度具有中等相关性(r = 0.428,P = 0.001);LESP和Eckardt评分的严重程度具有轻度相关性(r = 0.245,P = 0.004)。 结论 POEM治疗AC短期临床疗效显著,其中芝加哥Ⅱ型AC患者对POEM治疗反应最好,Ling分型中IIa、IIb、IIc及III型效果也好于I型;且HRM参数中4sIRP与Eckardt评分中度相关,对于POEM术后疗效具有较好的评估价值。 Abstract:Objective To investigate the correlation between esophageal manometry and short-term efficacy of Preoral endoscopic myotomy in patients with achalasia of cardia (AC). Methods Clinical data of AC patients who underwent POEM treatment for the first time in the Department of Gastroenterology at The First Affiliated Hospital of Soochow University from January 2019 to September 2024 were selected and grouped based on the 2020 Chicago 4.0 and Ling classifications. Baselin e data and surgical response rates of the patients were analyzed so as to compare Eckardt scores and esophageal manometry data of patients in different groupsand analyze the correlation between esophageal manometry data and postoperative clinical efficacy. Results (1) , The surgical success rate of 272 patients included in this study was 100%. The preoperative Eckardt score was (6.65 ± 1.48) points, and the Eckardt score 3 months after the surgery was (1.05 ± 0.56) points. The Eckardt score after POEM surgery decreased significantly compared to preoperative levels, and the difference was statistically significant (t = 19.823, P < 0.001). The postoperative Eckardt scores of the three groups of patients classified by Chicago and the five groups of patients classified by Ling were significantly lower than those before the surgery, and the differences were statistically significant (P < 0.05). (2) The postoperative LESP and 4SIRP of the three groups of patients classified by Chicago were significantly reduced compared with preoperative levels, and the differences were statistically significant (P < 0.05). And there was a statistically significant difference in the postoperative LESP and 4SIRP among the three groups of patients (P < 0.05); Further comparison using Bonferroni method showed that the LESP and 4SIRP of Group II were lower than those of Group I and Group III (both P < 0.05), but there was no statistically significant difference between Group I and Group III (both P > 0.05). The postoperative LESP and 4SIRP of the five groups of patients classified by Ling were also lower than those before the surgery, and the comparison was statistically significant (P < 0.05). There was also a statistically significant difference (P < 0.05) in the postoperative LESP and 4SIRP among the five groups of patients; Further comparison using Bonferroni method showed that the LESP and 4SIRP of groups IIa, IIb, IIc, and III were significantly lower than those of group I (all P < 0.05), but there was no statistically significant difference between groups IIa, IIb, IIc, and III (all P > 0.05). (3) The severity of 4SIRP and Eckardt scores showed a moderate correlation (r = 0.428, P = 0.001); The severity of LESP and Eckardt scores showed a mild correlation (r = 0.245, P = 0.004). Conclusion The short-term clinical efficacy of POEM treatment for AC is significant, with Chicago type II AC patients showing the best response to POEM treatment. Ling’ s classification of type IIa, IIb, IIc, and III shows better efficacy than type I; Moreover, there is a moderate correlation between the 4SIRP and Eckardt scores in the HRM parameters, which has good evaluation value for the postoperative efficacy of POEM. -
表 1 贲门失弛缓症临床症状评分系统(Eckardt评分)
Table 1. Clinical symptom scoring system of achalasia (Eckardt score)
评分 症状 体重减轻(kg) 吞咽困难 胸骨后疼痛 反流 0 无 无 无 无 1 < 5 偶尔 偶尔 偶尔 2 5~10 每天 每天 每天 3 > 10 每餐 每餐 每餐 表 2 患者基线资料特征[n(%)/($\bar x \pm s$)]
Table 2. Characteristics of patient baseline data [n(%)/($\bar x \pm s$)]
资料项目 资料数据特征 性别 男 128(47.06) 女 152 (52.94) 年龄(岁) 46.78 ± 17.1 BMI(kg/m2) 22.21 ± 2.79 病程(年) 4.56 ± 1.12 合并疾病 高血压 20 (27.78) 糖尿病 24 (33.33) 冠心病 12 (16.67) 慢性支气管炎 4 (5.56) 术前Eckardt评分(分) 6.65 ± 1.48 芝加哥分型 I 32(11.76) II 224(82.35) III 16(5.88) Ling分型 I 92(33.82) IIa 68(25.00) IIb 76(27.94) IIc 28(10.29) IIIl 4(1.47) IIIr 4(1.47) 注:BMI为体重指数。 表 3 不同亚组患者术前术后Eckardt评分比较[($\bar x \pm s $),分]
Table 3. Comparison of Eckardt scores of patients in different subgroups before and after operation [($\bar x \pm s $), points]
分型 组别 术前Eckardt评分 术后Eckardt评分 t P 芝加哥分型 I型组(n = 32) 6.25 ± 1.44 0.94 ± 0.48 17.721 < 0.001* II型组(n = 224) 6.72 ± 1.49 1.08 ± 0.57 15.892 < 0.001* III型组(n = 16) 6.98 ± 1.53 1.16 ± 0.62 18.305 < 0.001* F 0.377 1.073 P 0.735 0.166 Ling分型 I型组(n = 92) 6.24 ± 1.48 0.93 ± 0.45 15.912 < 0.001* IIa型组(n = 76) 6.55 ± 1.48 1.02 ± 0.58 16.831 < 0.001* IIb型组(n = 68) 6.73 ± 1.48 1.05 ± 0.60 18.032 < 0.001* IIc型组(n = 28) 6.71 ± 1.48 1.07 ± 0.61 18.830 < 0.001* III型组(n = 8) 7.02 ± 1.48 1.18 ± 0.64 19.883 < 0.001* F 0.970 1.674 P 0.196 0.089 *P < 0.001。 表 4 芝加哥分型五组患术前术后食管测压情况比较($\bar x \pm s $)(1)
Table 4. Comparison of preoperative and postoperative esophageal manometry in five groups of patients with Chicago classification($\bar x \pm s $)(1)
组别 UESP(mmHg) LESP(mmHg) 术前 术后 t P 术前 术后 t P I型(n = 32) 50.42 ± 15.28 45.90 ± 11.32 1.345 0.089 31.05 ± 10.18 23.21 ± 7.54 3.890 < 0.001* II型(n = 224) 51.58 ± 15.54 46.21 ± 12.67 1.424 0.078 32.37 ± 10.84 18.73 ± 6.05 5.931 < 0.001* III型(n = 16) 52.04 ± 15.97 46.97 ± 15.82 1.783 0.061 33.81 ± 10.38 21.51 ± 6.53 6.843 < 0.001* F 0.784 0.376 0.938 2.477 P 0.345 0.728 0.126 0.039 表 4 芝加哥分型五组患术前术后食管测压情况比较($\bar x \pm s $) (2)
Table 4. Comparison of preoperative and postoperative esophageal manometry in five groups of patients with Chicago classification($\bar x \pm s $)(2)
组别 4sIRP(mmHg) LESL(cm) 术前 术后 t P 术前 术后 t P I型(n = 32) 22.23 ± 7.36 11.93 ± 4.12 8.941 < 0.001* 3.02 ± 0.58 3.01 ± 0.81 0.082 0.949 II型(n = 224) 23.81 ± 7.23 9.16 ± 3.79 11.210 < 0.001* 3.07 ± 0.48 3.05 ± 0.54 0.075 0.956 III型(n = 16) 23.75 ± 7.64 10.37 ± 3.12 14.536 < 0.001* 3.09 ± 0.54 3.11 ± 0.69 0.084 0.945 F 0.508 2.351 0.289 0.310 P 0.596 0.043 0.863 0.757 *P < 0.001。 表 5 Ling分型五组患术前术后食管测压情况比较($\bar x \pm s $)(1)
Table 5. Comparison of preoperative and postoperative esophageal manometry in five groups of patients with Ling classification($\bar x \pm s $)(2)
组别 UESP(mmHg) LESP(mmHg) 术前 术后 t P 术前 术后 t P I型(n = 92) 50.57 ± 14.74 45.93 ± 11.56 1.247 0.093 31.01 ± 10.13 23.43 ± 5.54 3.994 < 0.001* IIa型(n = 76) 51.21 ± 16.35 46.24 ± 13.62 1.420 0.079 31.18 ± 10.79 18.54 ± 6.58 5.554 < 0.001* IIb型(n = 68) 51.14 ± 15.58 46.39 ± 14.86 1.698 0.086 31.78 ± 10.36 17.46 ± 5.91 6.742 < 0.001* IIc型(n = 28) 51.26 ± 16.19 46.84 ± 14.63 1.579 0.068 32.37 ± 10.76 17.14 ± 6.17 6.821 < 0.001* III型(n = 8) 52.55 ± 16.70 47.13 ± 15.81 1.698 0.086 33.56 ± 10.93 16.86 ± 6.28 7.073 < 0.001* F 0.862 0.456 1.011 0.477 P 0.241 0.645 0.107 0.484 表 5 Ling分型五组患术前术后食管测压情况比较($\bar x \pm s $)(2)
Table 5. Comparison of preoperative and postoperative esophageal manometry in five groups of patients with Ling classification($\bar x \pm s $)(2)
组别 4sIRP(mmHg) LESL(cm) 术前 术后 t P 术前 术后 t P I型(n = 92) 22.76 ± 7.24 11.91 ± 4.15 8.8721 < 0.001* 3.03 ± 0.59 3.02 ± 0.83 0.065 0.981 IIa型(n = 76) 23.12 ± 7.06 9.10 ± 3.83 10.821 < 0.001* 3.06 ± 0.47 3.04 ± 0.56 0.079 0.950 IIb型(n = 68) 23.09 ± 6.95 8.97 ± 3.57 9.935 < 0.001* 3.08 ± 0.55 3.12 ± 0.68 0.085 0.946 IIc型(n = 28) 23.10 ± 7.03 8.89 ± 3.45 10.391 < 0.001* 3.03 ± 0.57 3.02 ± 0.82 0.091 0.932 III型(n = 8) 23.11 ± 7.14 8.15 ± 3.09 15.823 < 0.001* 3.05 ± 0.49 3.06 ± 0.55 0.080 0.949 F 0.761 3.751 0.511 0.699 P 0.316 0.014 0.454 0.208 *P < 0.001。 -
[1] 中华医学会消化病学分会胃肠动力学组,胃肠功能性疾病协作组,食管疾病协作组. 中国贲门失弛缓症诊疗规范[J]. 中华消化杂志,2023,43(10):657-664. doi: 10.3760/cma.j.cn311367-20230704-00299 [2] 孙家宁,许青芃,马亦凡,等. 经口内镜下肌切开术及其衍生技术应用的研究进展[J]. 中华消化内镜杂志,2023,40(11):940-945. doi: 10.3760/cma.j.cn321463-20221122-00450 [3] 中国医师协会消化医师分会胃食管反流病专业委员会. 中国高分辨率食管测压临床操作指南(成人)[J]. 中华消化杂志,2020,40(1):3-8. doi: 10.3760/cma.j.issn.0254-1432.2020.01.002 [4] Fox M R,Sweis R,Yadlapati R,et al. Chicago classification version 4.0© technical review:Update on standard high-resolution manometry protocol for the assessment of esophageal motility[J]. Neurogastroenterol Motil,2021,33(4):e14120. doi: 10.1111/nmo.14120 [5] 李泽宇,黄留业. 高分辨率食管测压在经口内镜下肌切开术治疗贲门失弛缓症中的应用价值[J]. 中国内镜杂志,2021,27(2):55-60. doi: 10.12235/E20200286 [6] 陈棒,刘曼,徐红,等. 贲门失弛缓症经口内镜下肌切开术后食管动力类型分析[J]. 胃肠病学,2022,27(8):449-455. [7] Khan A,Yadlapati R,Gonlachanvit S,et al. Chicago classification update (version 4.0):Technical review on diagnostic criteria for achalasia[J]. Neurogastroenterol Motil,2021,33(7):e14182. doi: 10.1111/nmo.14182 [8] 李惠凯,令狐恩强,王向东,等. Ling分型对经口内镜下肌切开术手术并发症的影响[J]. 中华腔镜外科杂志(电子版),2012,5(5):4-6. doi: 10.3877/cma.j.issn.1674-6899.2012.05.003 [9] Provenza C G,Romanelli J R. Achalasia:Diagnosis and management[J]. Surg Clin North Am,2025,105(1):143-158. doi: 10.1016/j.suc.2024.06.011 [10] Fetzner U K,Trujillo M,Dimopoulos I,et al. Update achalasie[J]. Ther Umsch,2022,79(3-4):133-140. [11] Azahar Z A,Ab Rahim M F,Ahmad N,et al. Achalasia in pregnancy[J]. BMJ Case Rep,2024,17(5):e257698. doi: 10.1136/bcr-2023-257698 [12] 狄育竹,徐洪雨. 贲门失弛缓症的诊断与治疗进展[J]. 胃肠病学和肝病学杂志,2018,27(1):92-95. [13] 张莉莉,王彬,晋弘,等. 贲门失弛缓症的病因和治疗进展[J]. 胃肠病学,2019,24(12):745-749. [14] Nabi Z,Ramchandani M,Basha J,et al. POEM is a durable treatment in children and adolescents with achalasia cardia[J]. Front Pediatr,2022,25(10):812201. [15] 庄羽骁,胡颖. 经口内镜下肌切开术治疗贲门失弛缓症的现状和进展[J]. 胃肠病学和肝病学杂志,2019,28(8):942-946. [16] 张元,崔子瑾,王鼎鑫,等. 贲门失弛缓症患者食管测压与Eckardt评分的相关性分析[J]. 中国临床医生杂志,2023,51(10):1172-1176. [17] 杨燕,马美雪,王艳. 不同亚型贲门失弛缓症患者食管测压特征比较及经口内镜下肌切开术后食管功能改变分析[J]. 临床和实验医学杂志,2021,20(21):2303-2307. doi: 10.3969/j.issn.1671-4695.2021.21.018 [18] 张含花,方莹,任晓侠,等. 高分辨率食管测压评估经口内镜下肌切开术治疗儿童贲门失弛缓症的临床研究[J]. 中华消化内镜杂志,2021,38(1):57-61. [19] Leung L J,Ma G K,Lee J K,et al. Successful design and implementation of a POEM program for achalasia in an integrated healthcare system[J]. Dig Dis Sci,2023,68(6):2276-2284 doi: 10.1007/s10620-023-07839-y [20] 李清,陈秀秉,宁静,等. 热活检钳法与传统法经口内镜食管下括约肌切开术治疗贲门失弛缓症的疗效比较[J]. 中国内镜杂志,2023,29(4):50-56. doi: 10.12235/E20220579 [21] Yadlapati R,Kahrilas P J,Fox M R,et al. Esophageal motility disorders on high-resolution manometry:Chicago classification version 4.0©[J]. Neurogastroenterol Motil,2024,36(2):e14179. doi: 10.1111/nmo.14179 [22] Jin H,Zhao W,Zhang L,et al. Is integrated relaxation pressure a promising predictor of effectiveness of peroral endoscopic myotomy for achalasia?[J]. Z Gastroenterol,2018,56(2):111-116. doi: 10.1055/s-0043-120348 [23] 谢忱,汤玉蓉,王美峰,等. 30例贲门失弛缓症的临床症状与其食管测压相关性[J]. 中华消化杂志,2015,35(5):319-322. [24] 马永芬,鞠辉,张翠萍,等. 食管测压在评价和预测经口内镜下肌切开术治疗贲门失弛缓症疗效中的作用[J]. 中华消化内镜杂志,2015,32(12):808-812. doi: 10.3760/cma.j.issn.1007-5232.2015.12.007 [25] 李蒙,吕宾,张璐,等. 食管高分辨率测压观察经口内镜下肌切开术对33例不同亚型贲门失弛缓症的疗效评价[J]. 中华消化杂志,2016,36(4):254-258. -





 下载:
下载: