Epidemiological Characteristics of Venomous Snakebite in Yunnan Province
-
摘要:
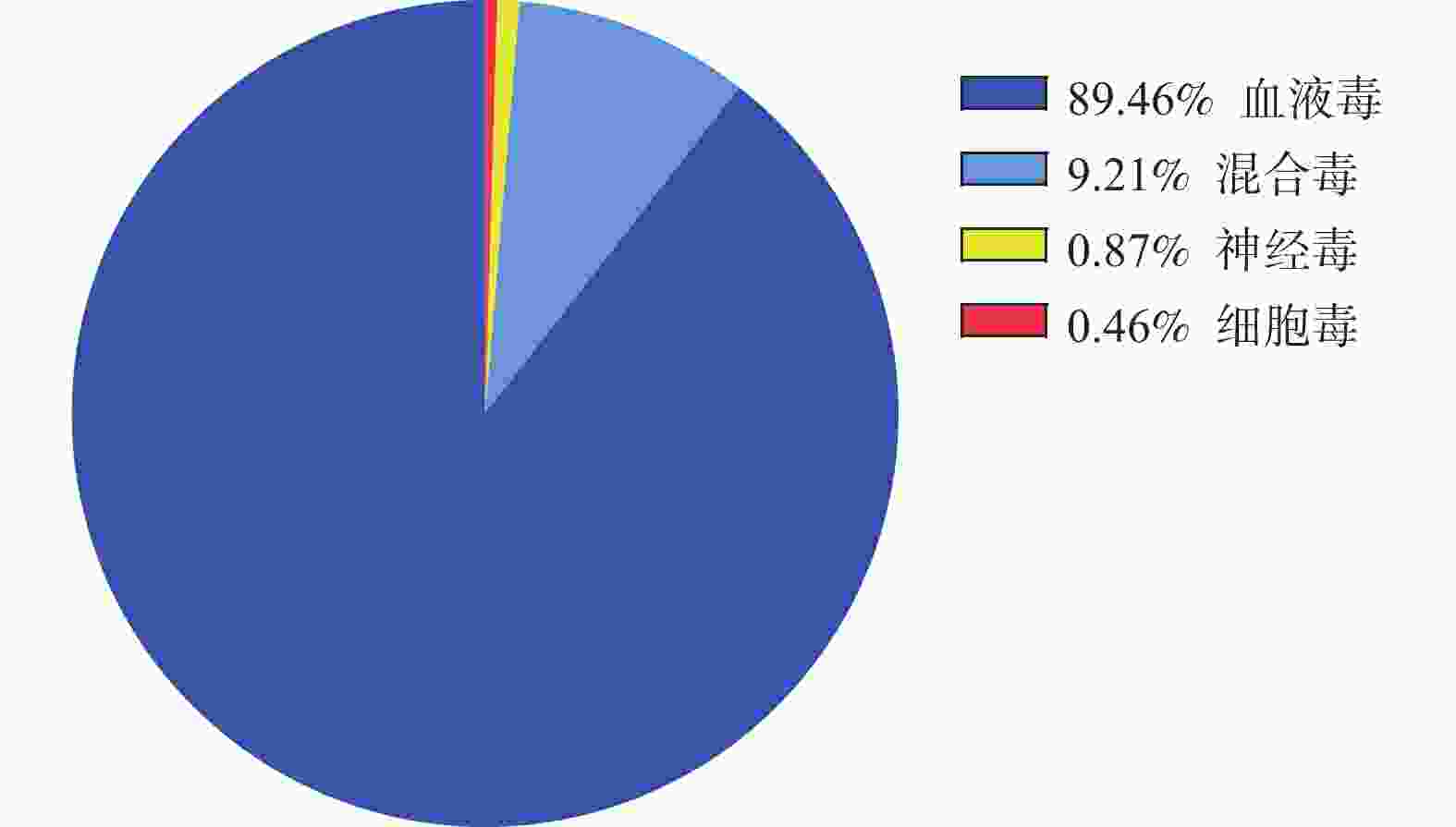
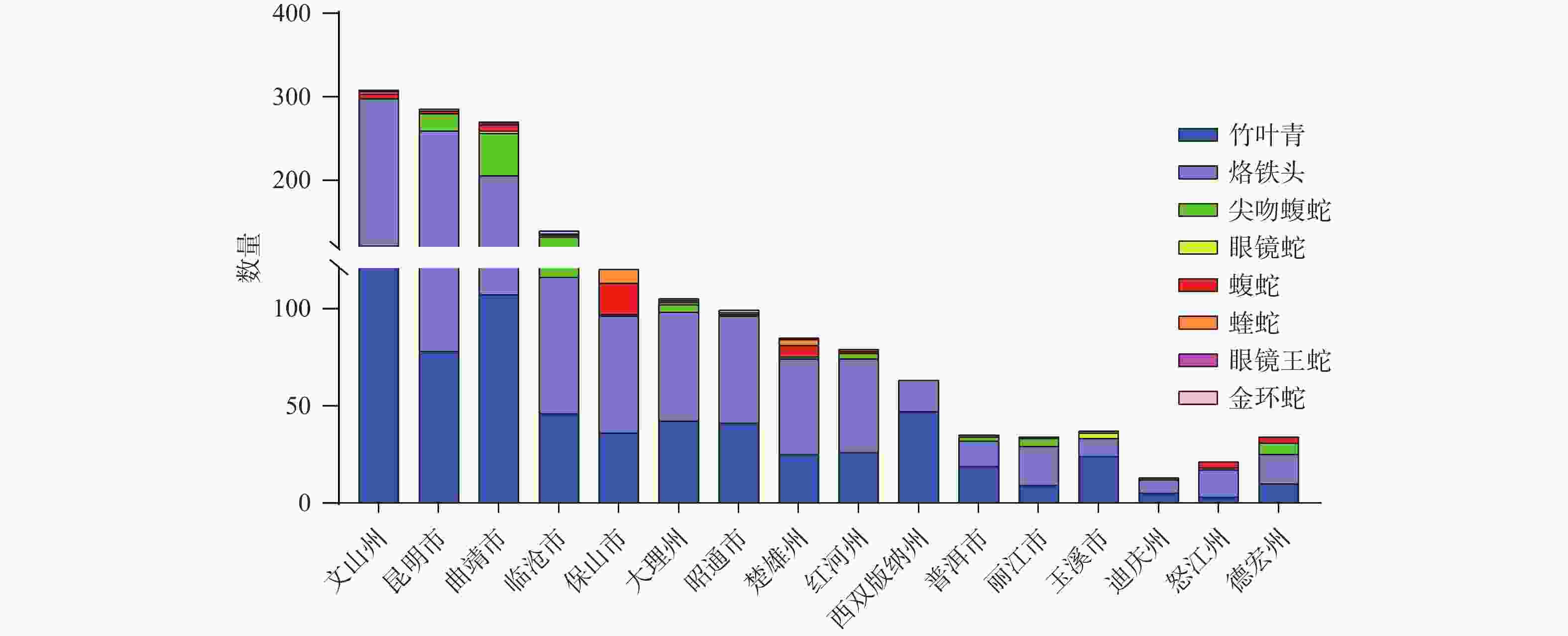
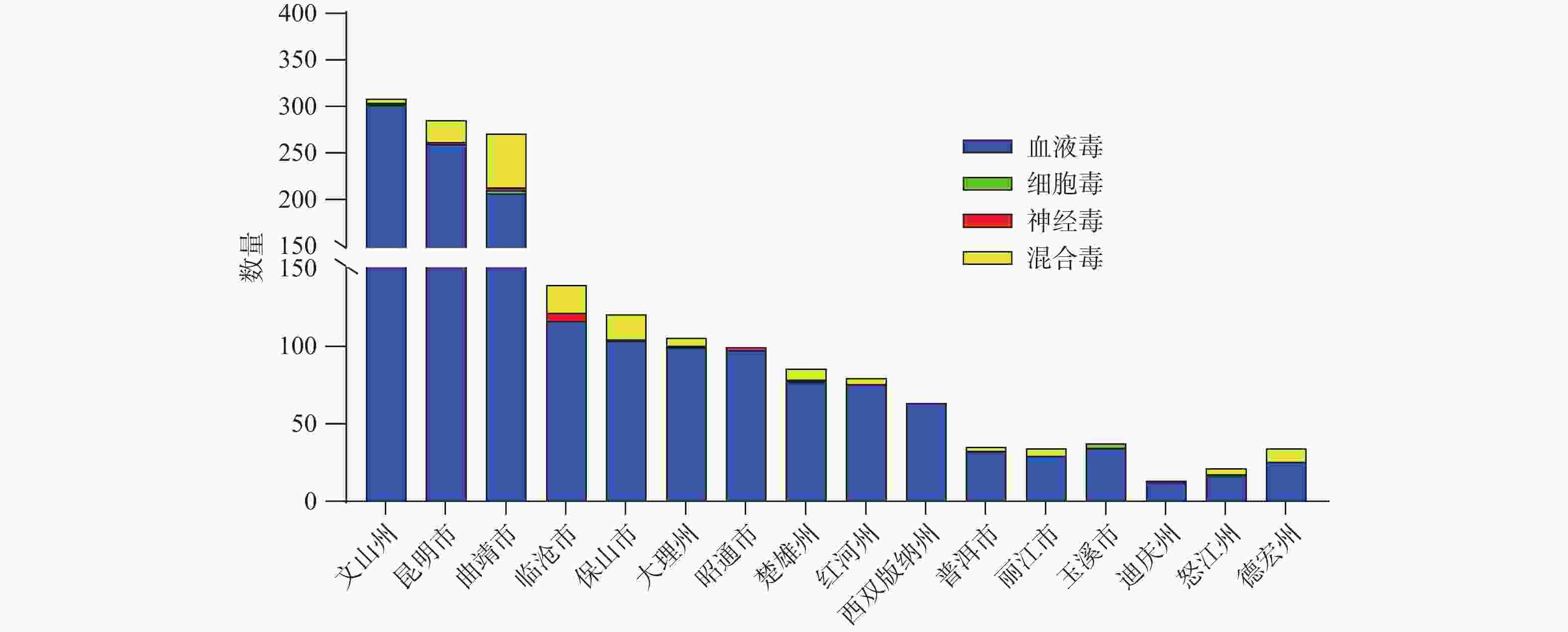
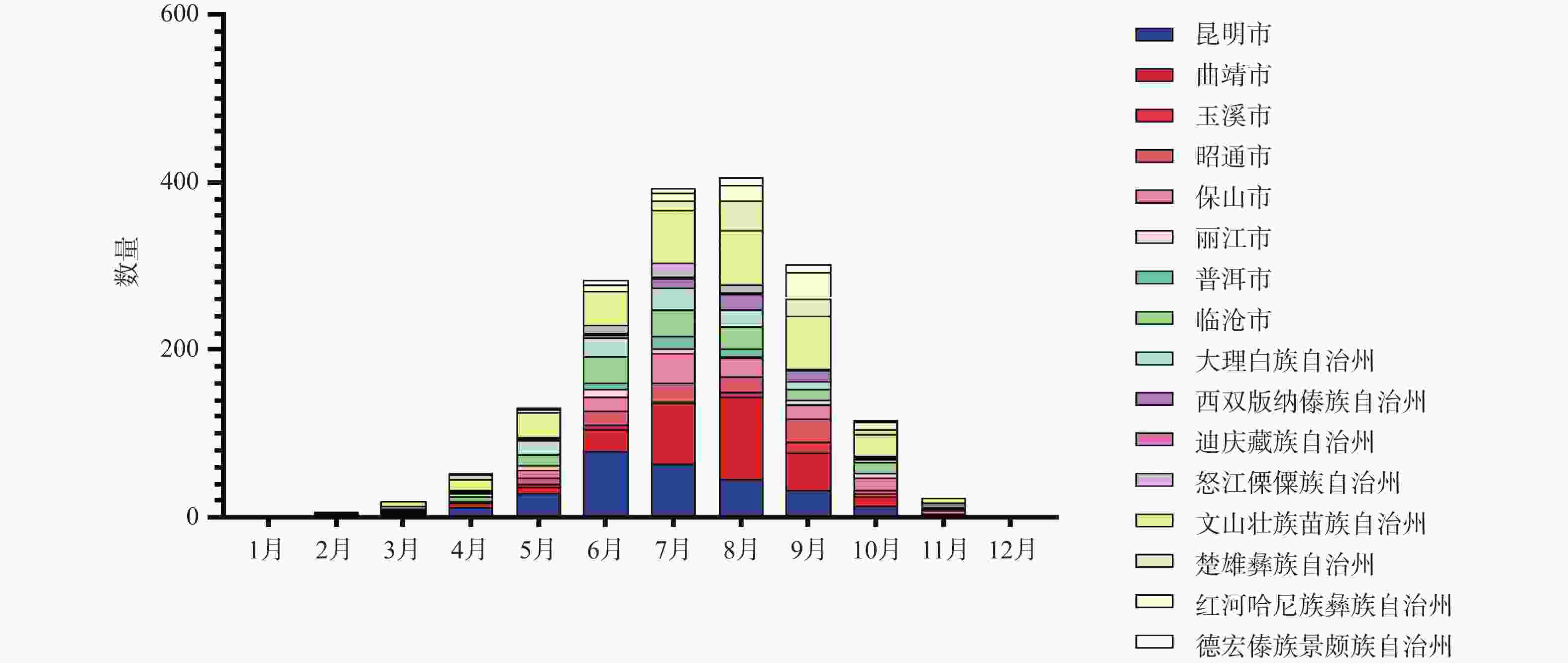
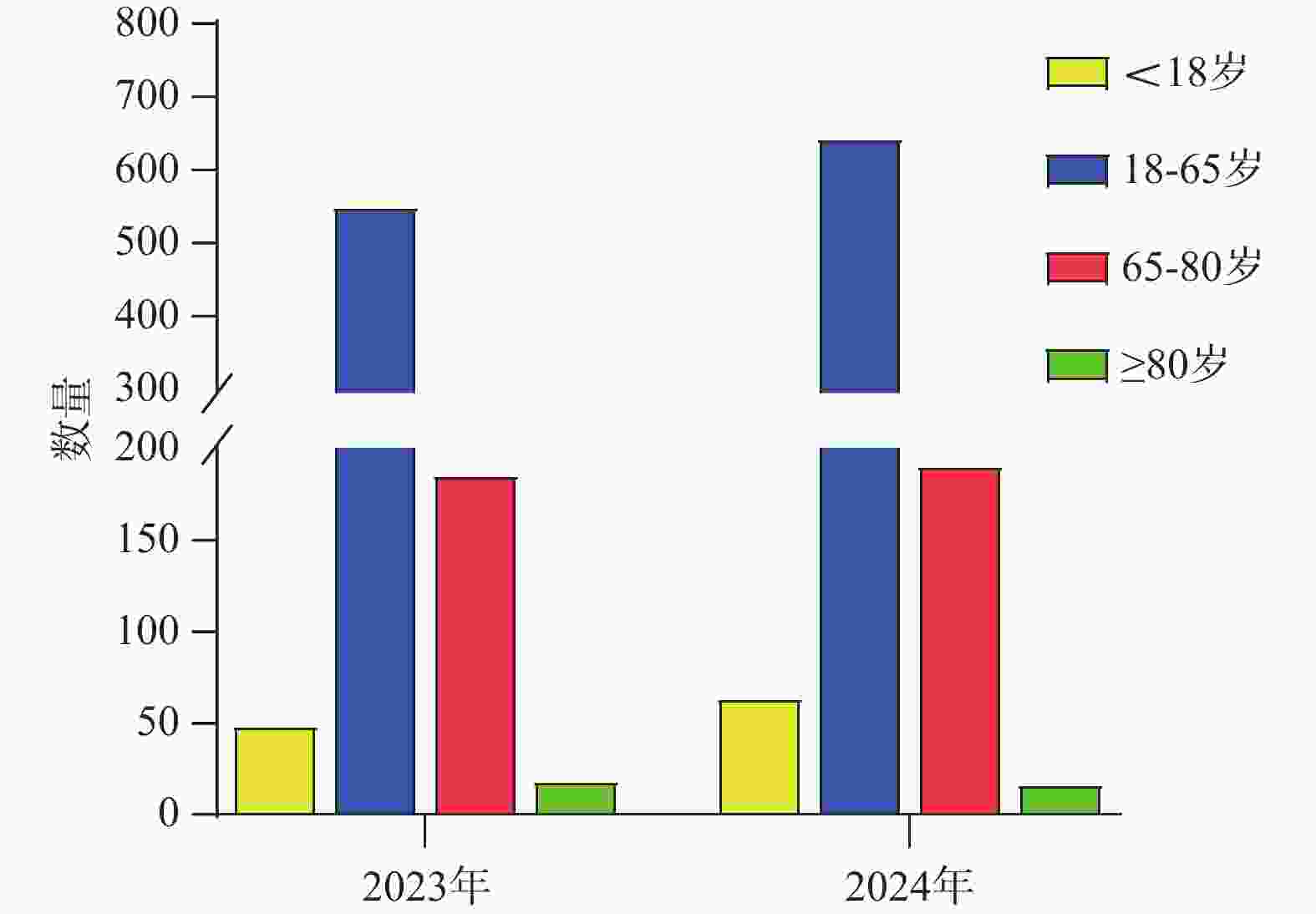
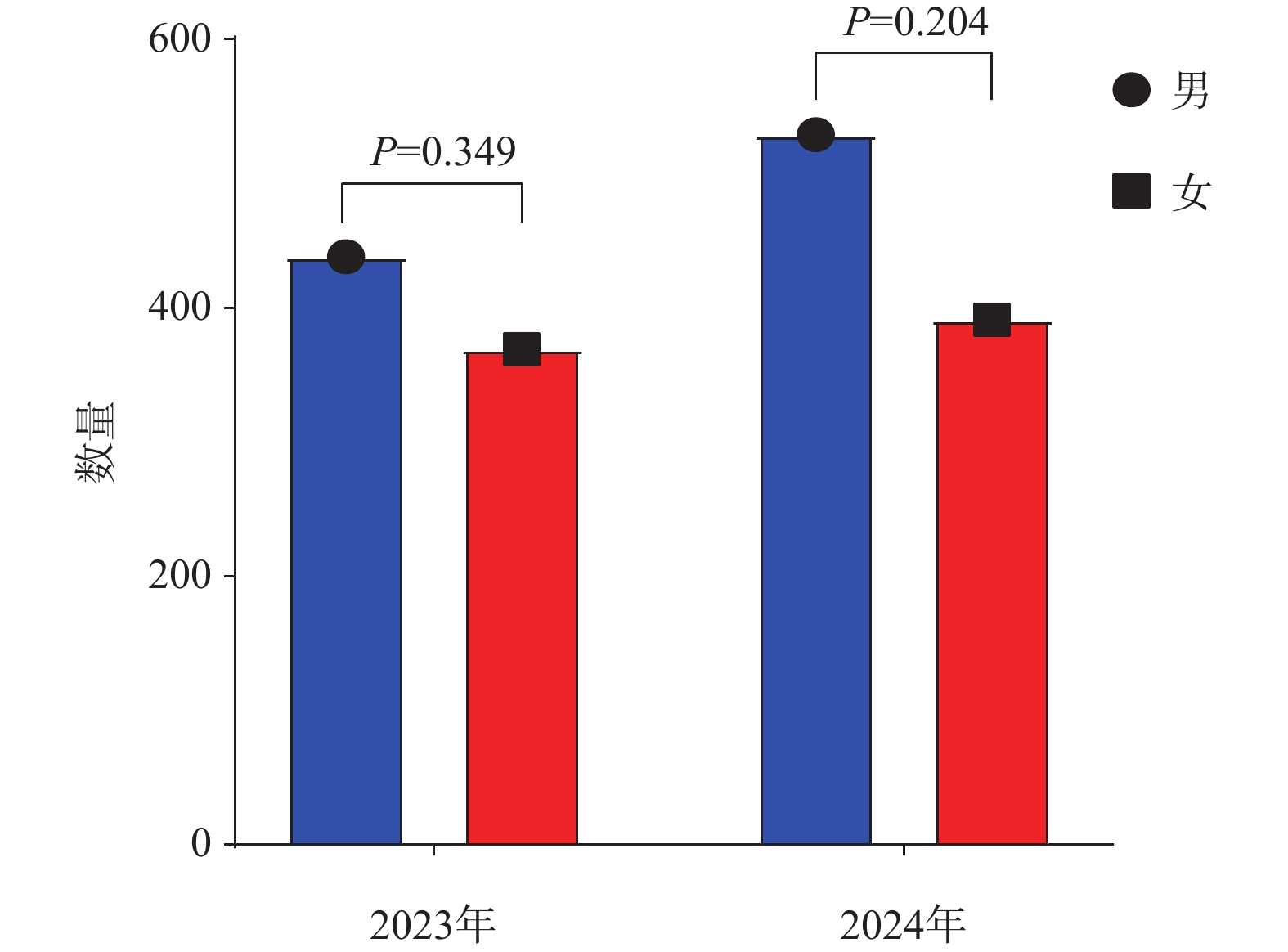
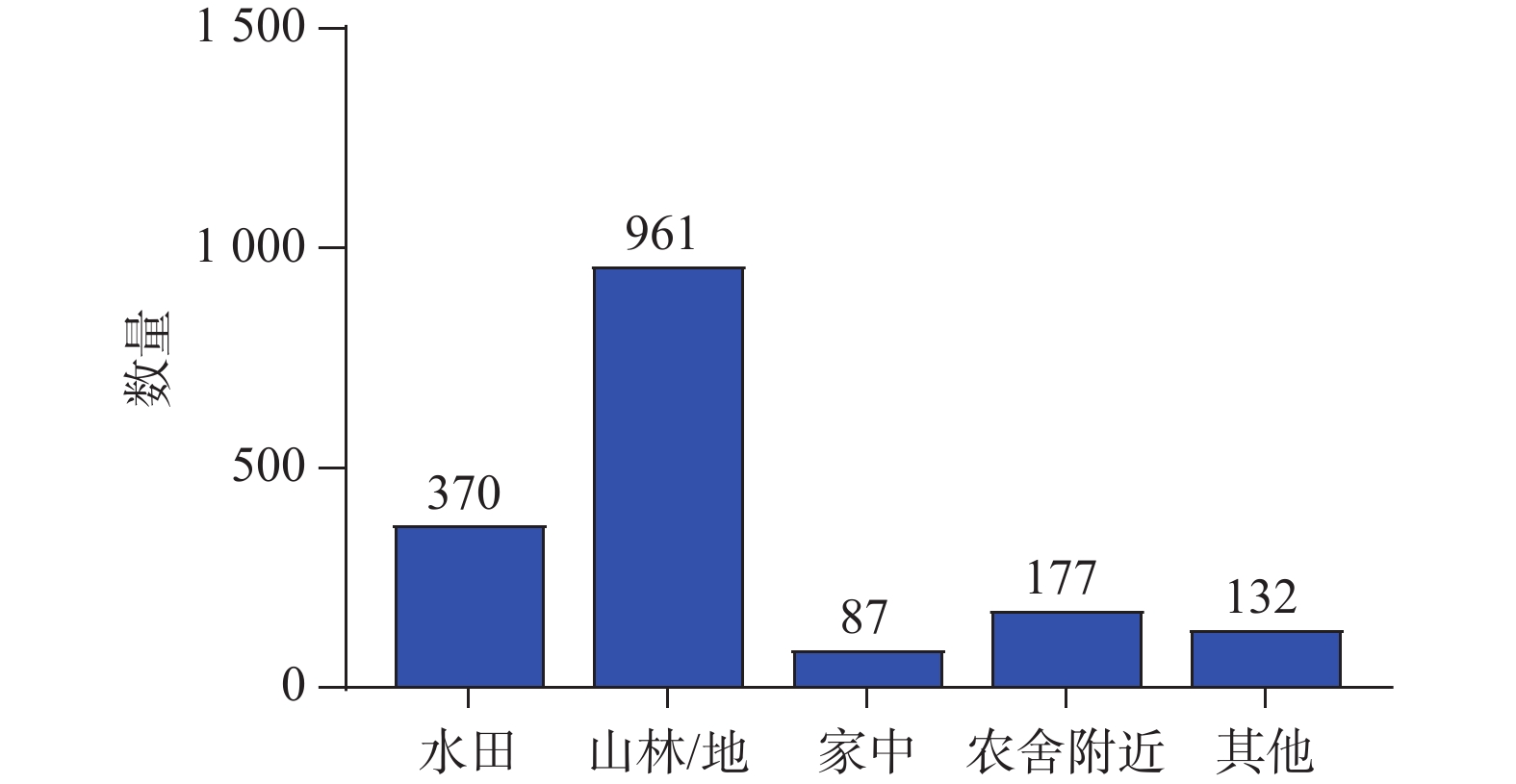
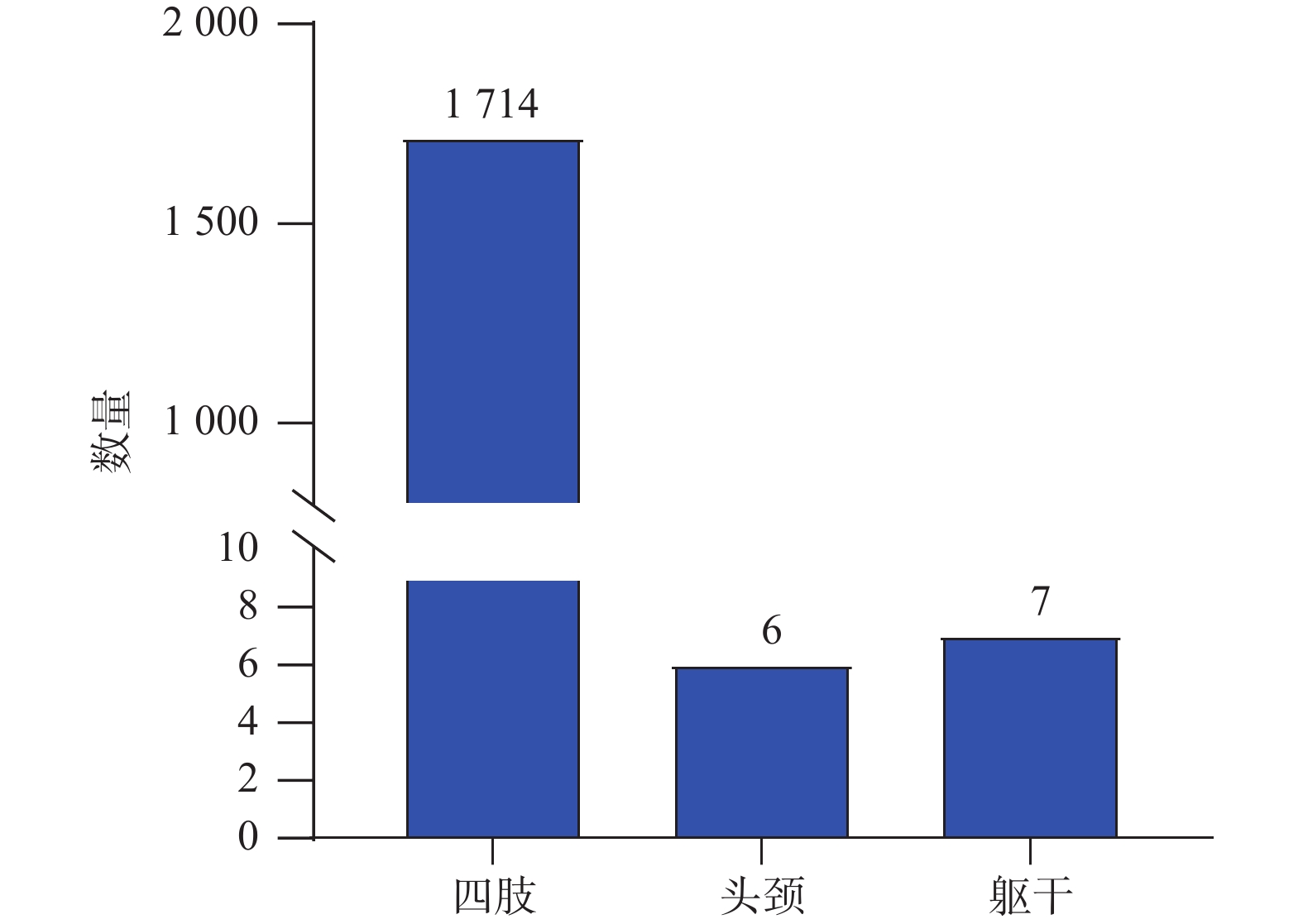
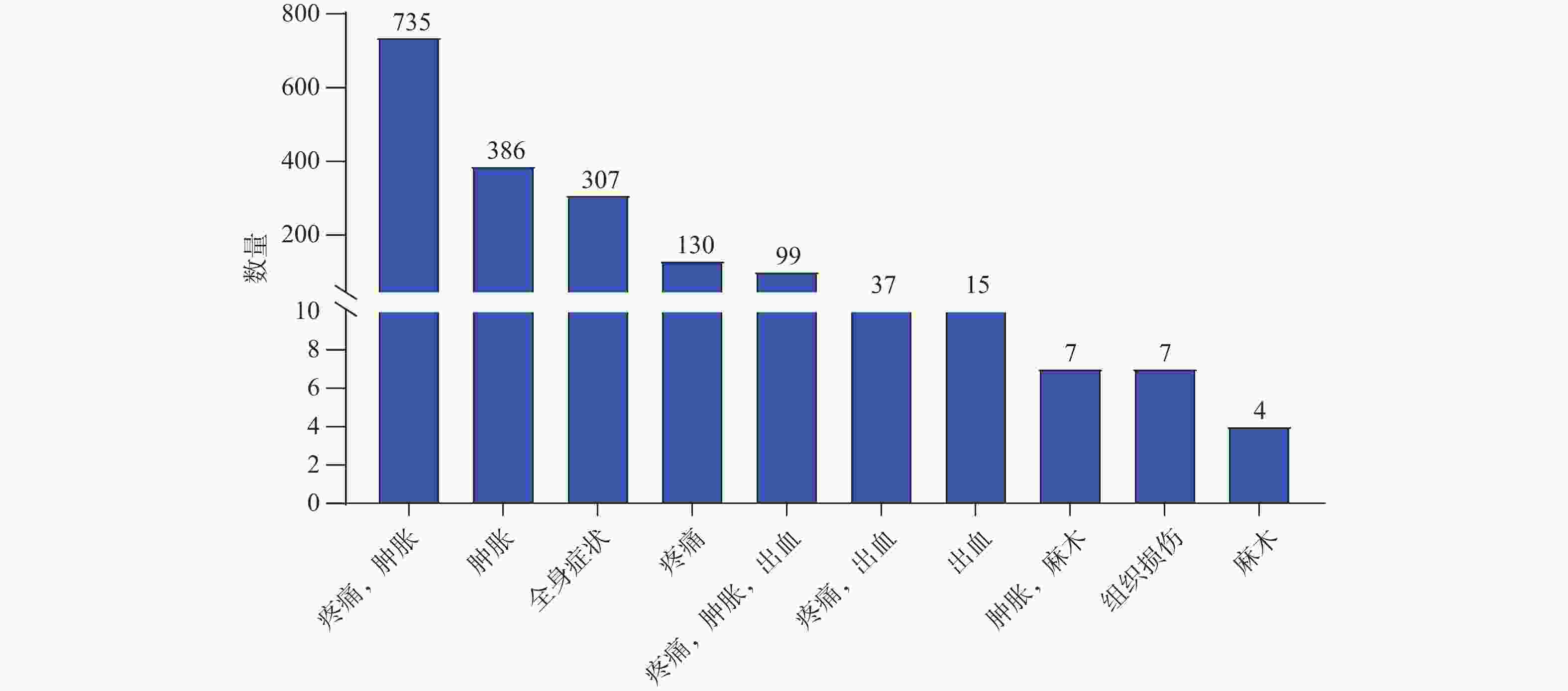
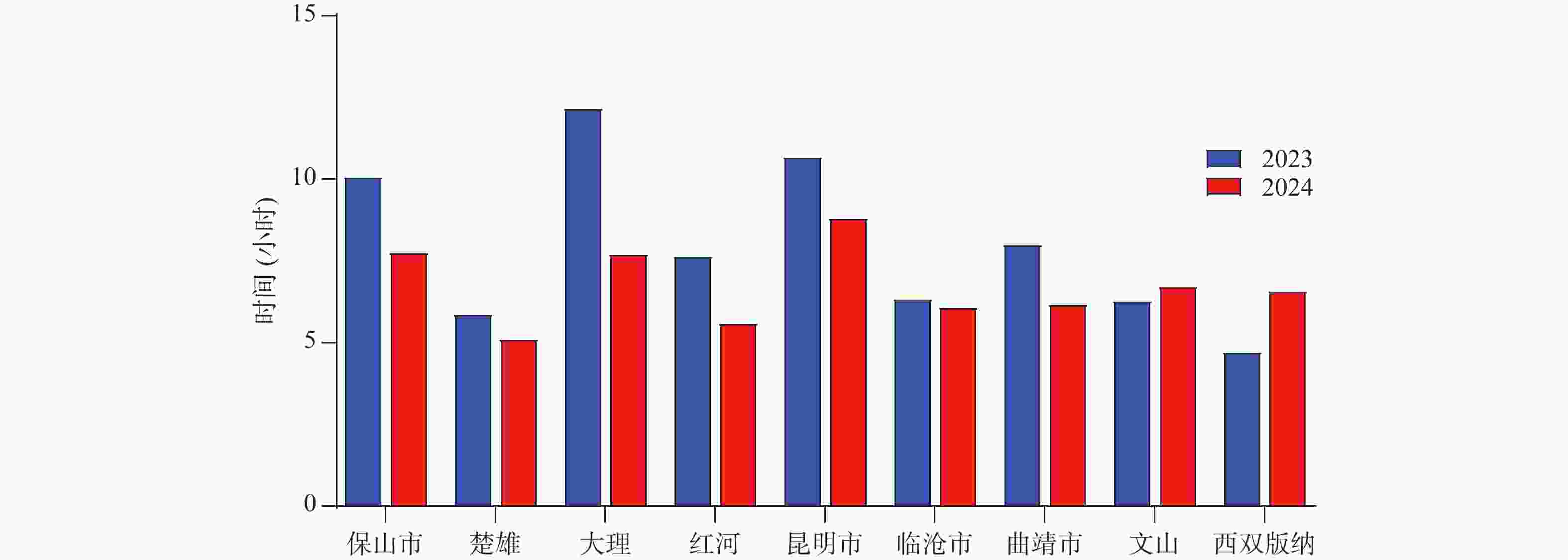
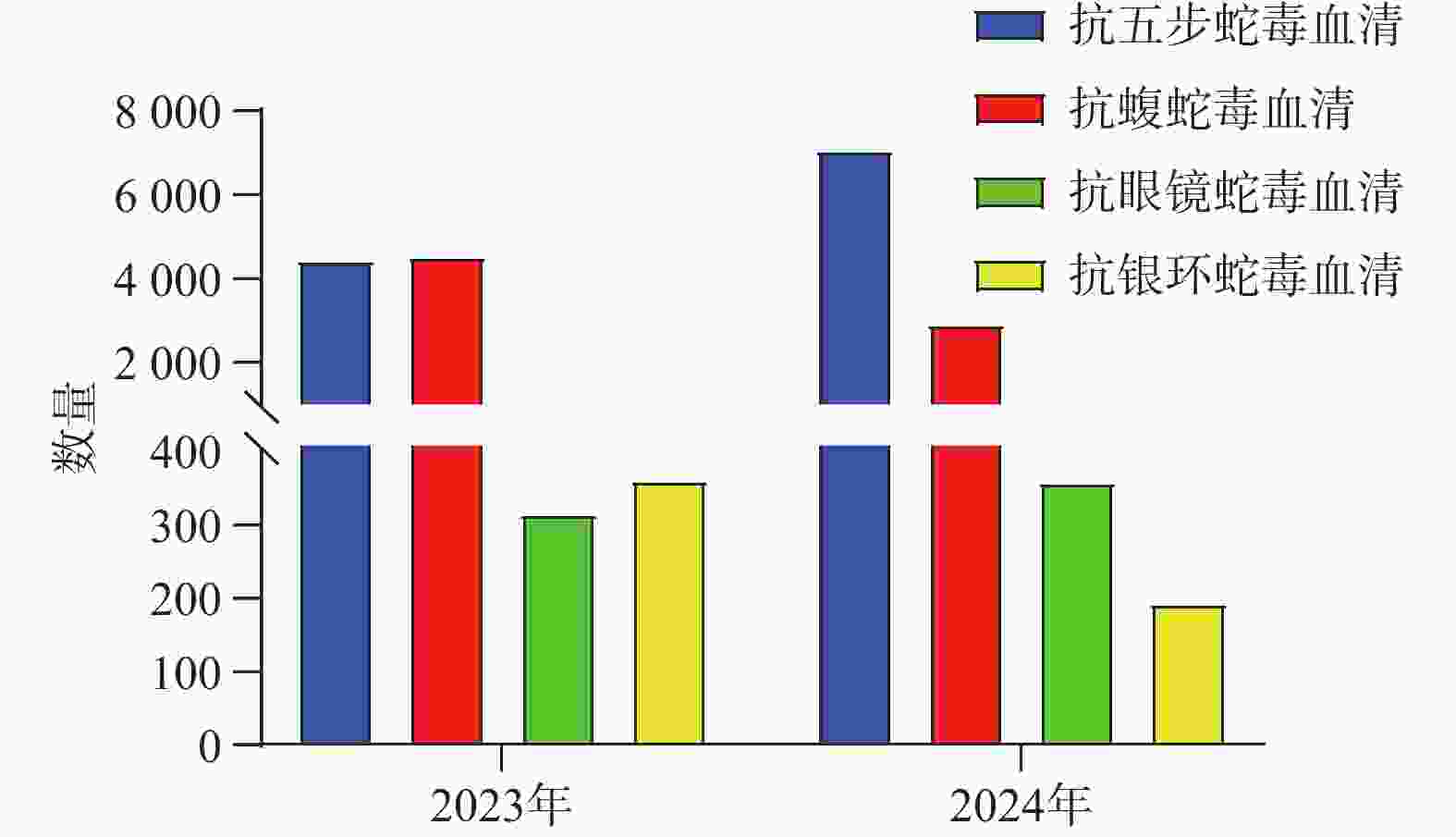
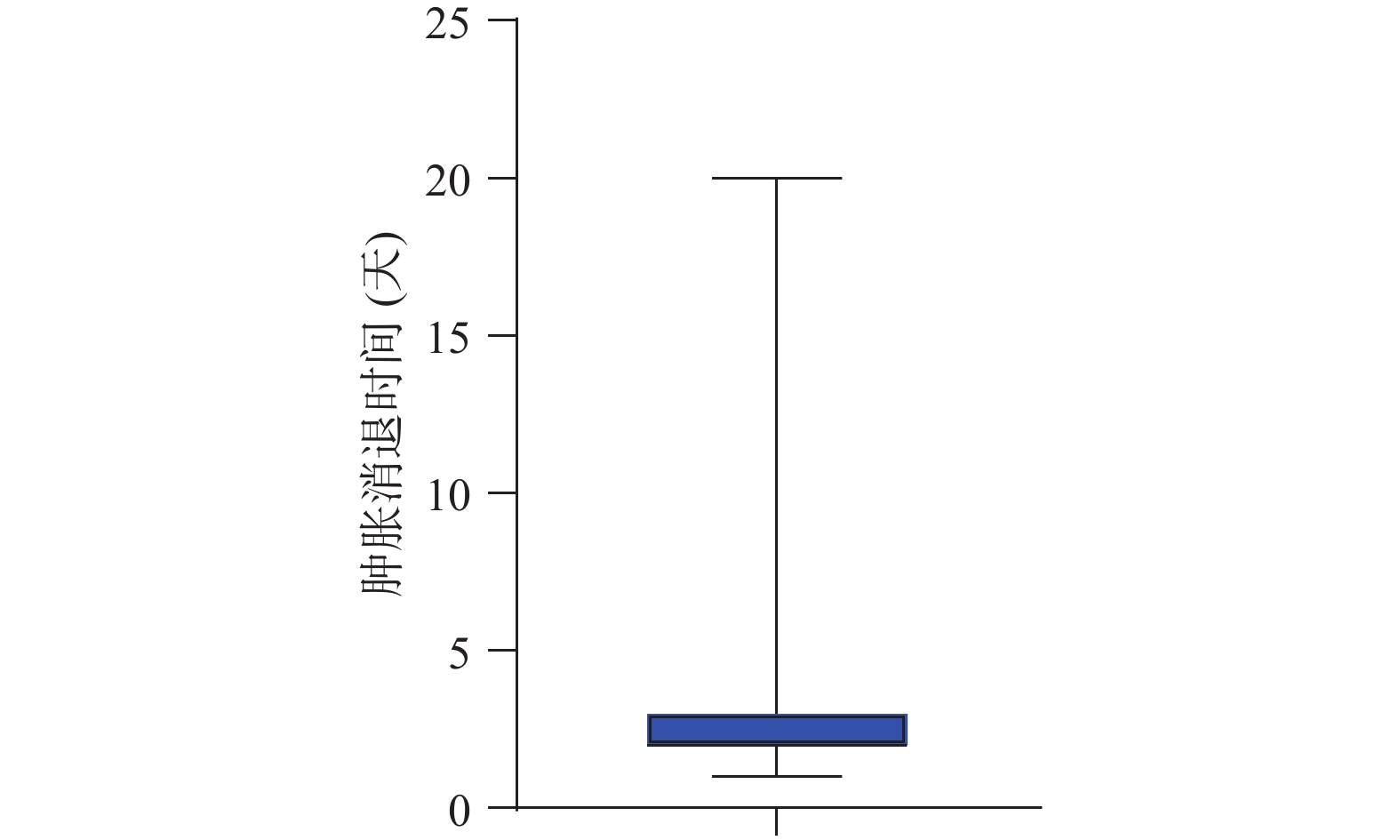
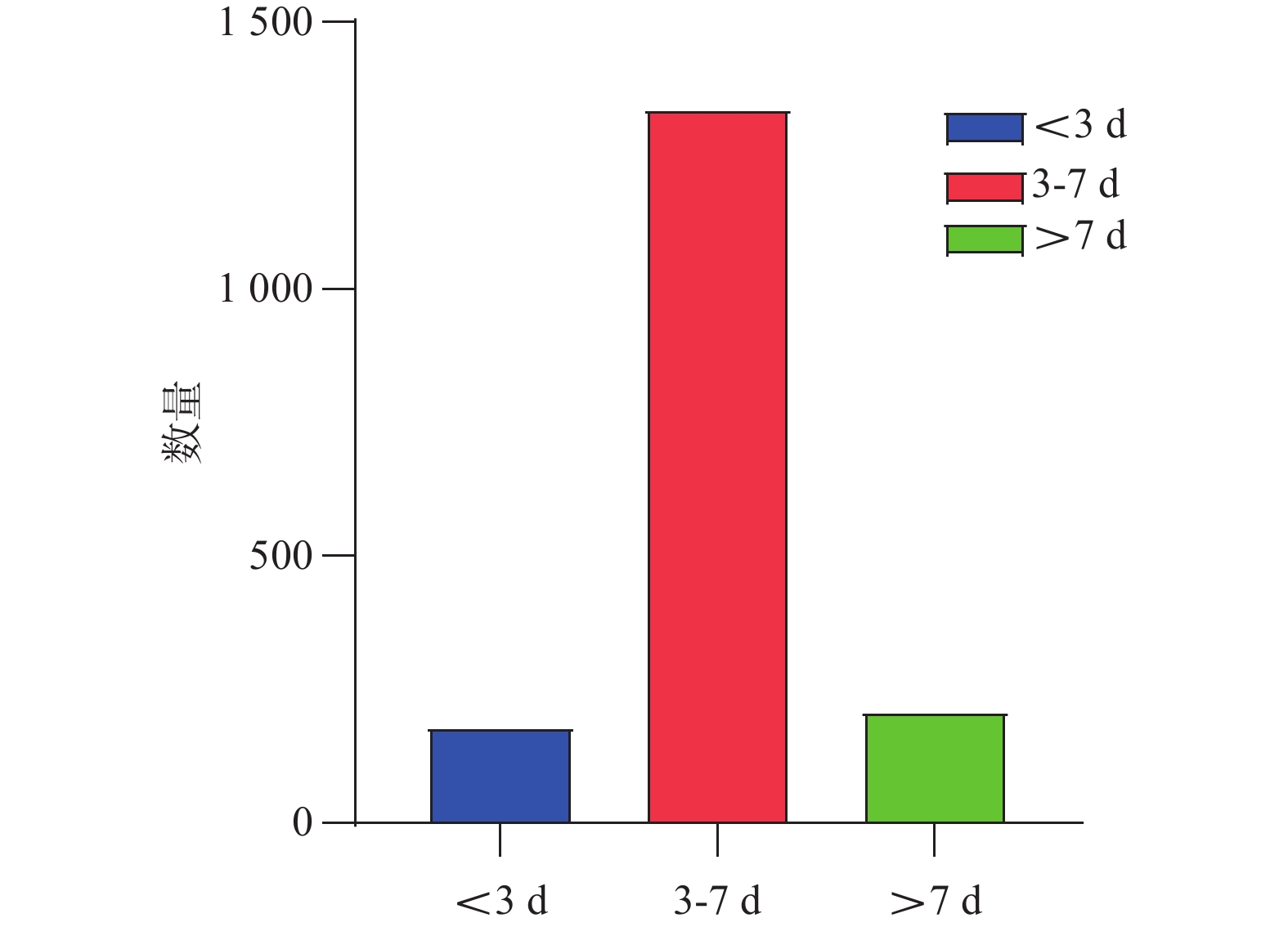
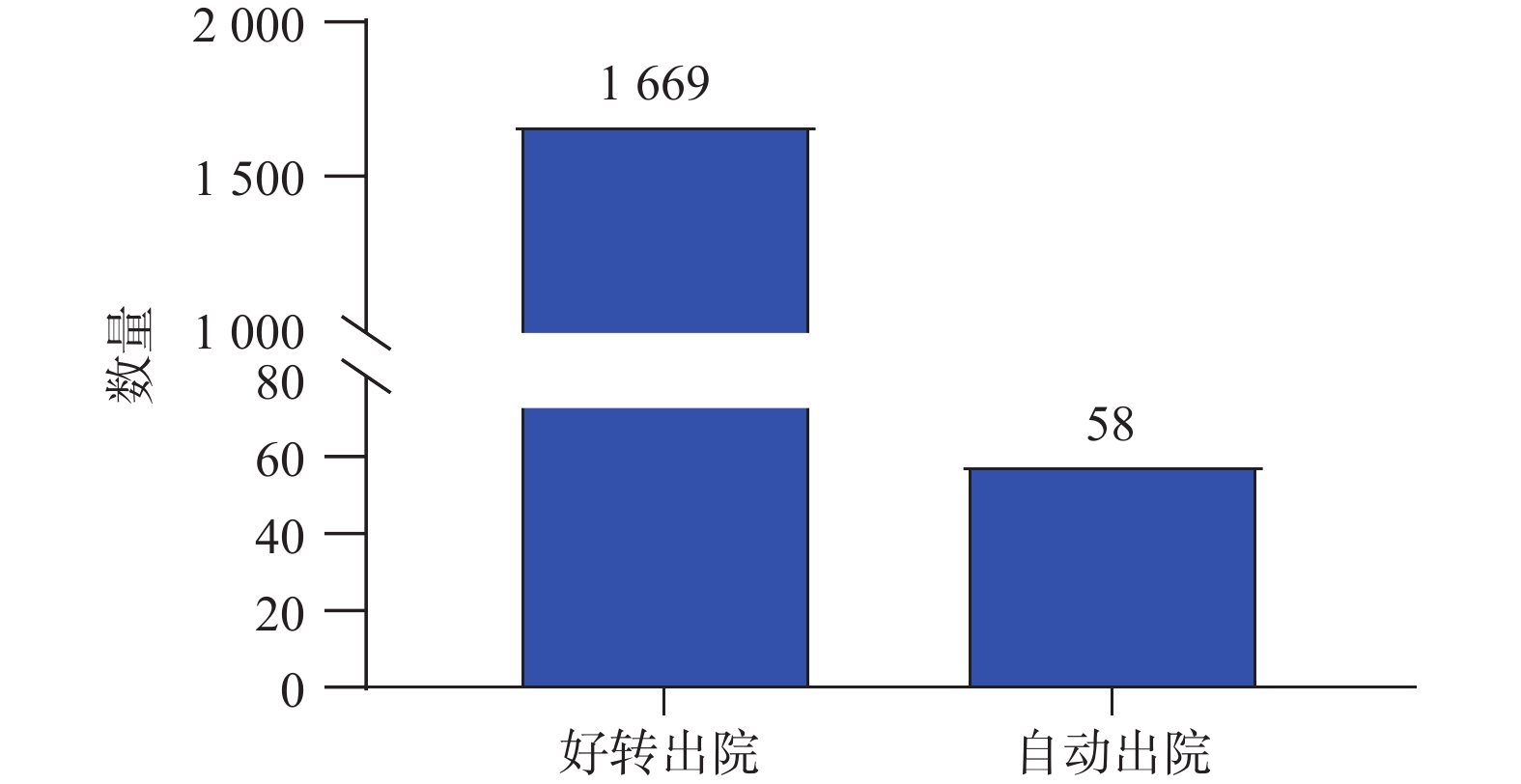
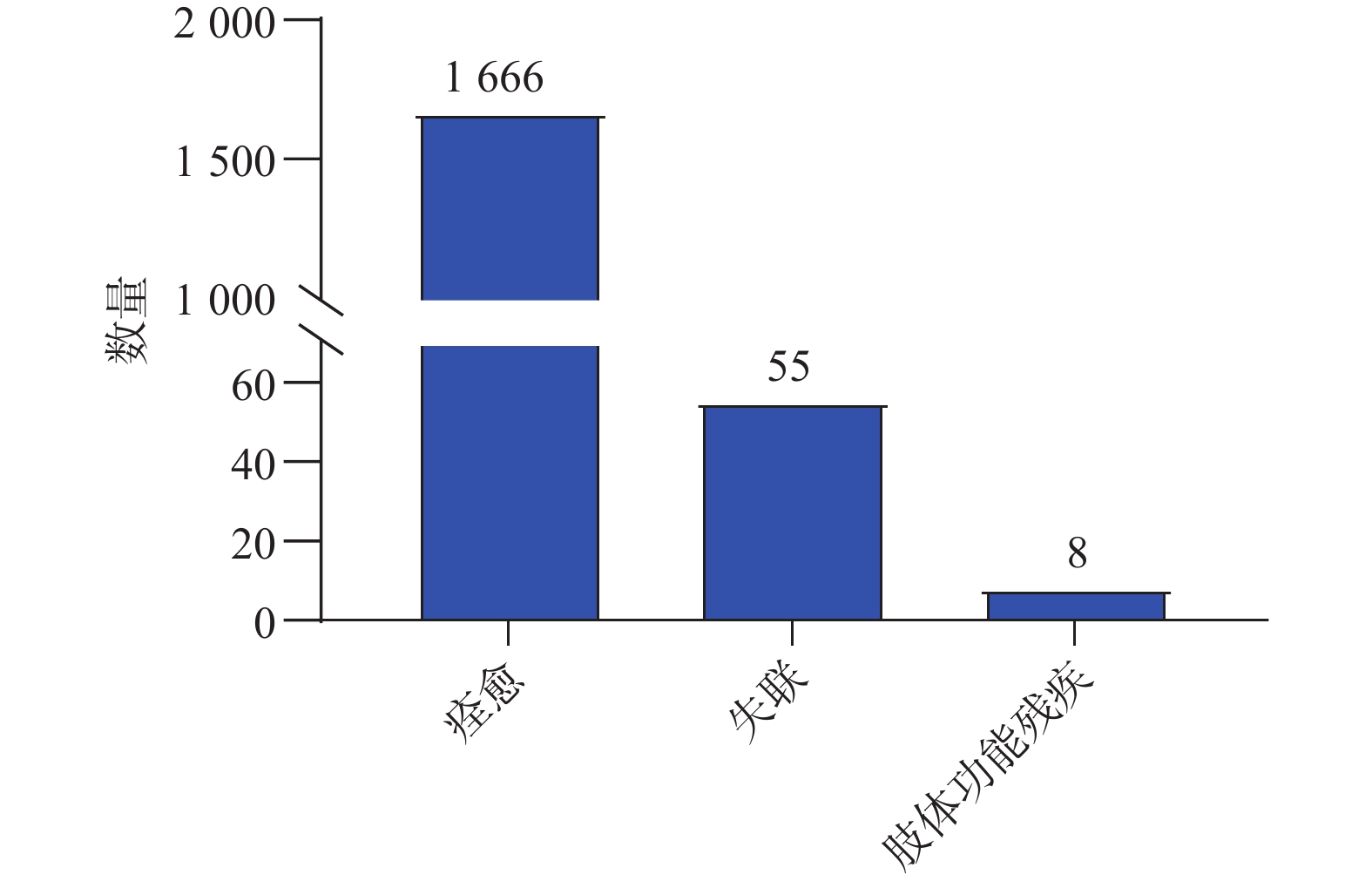
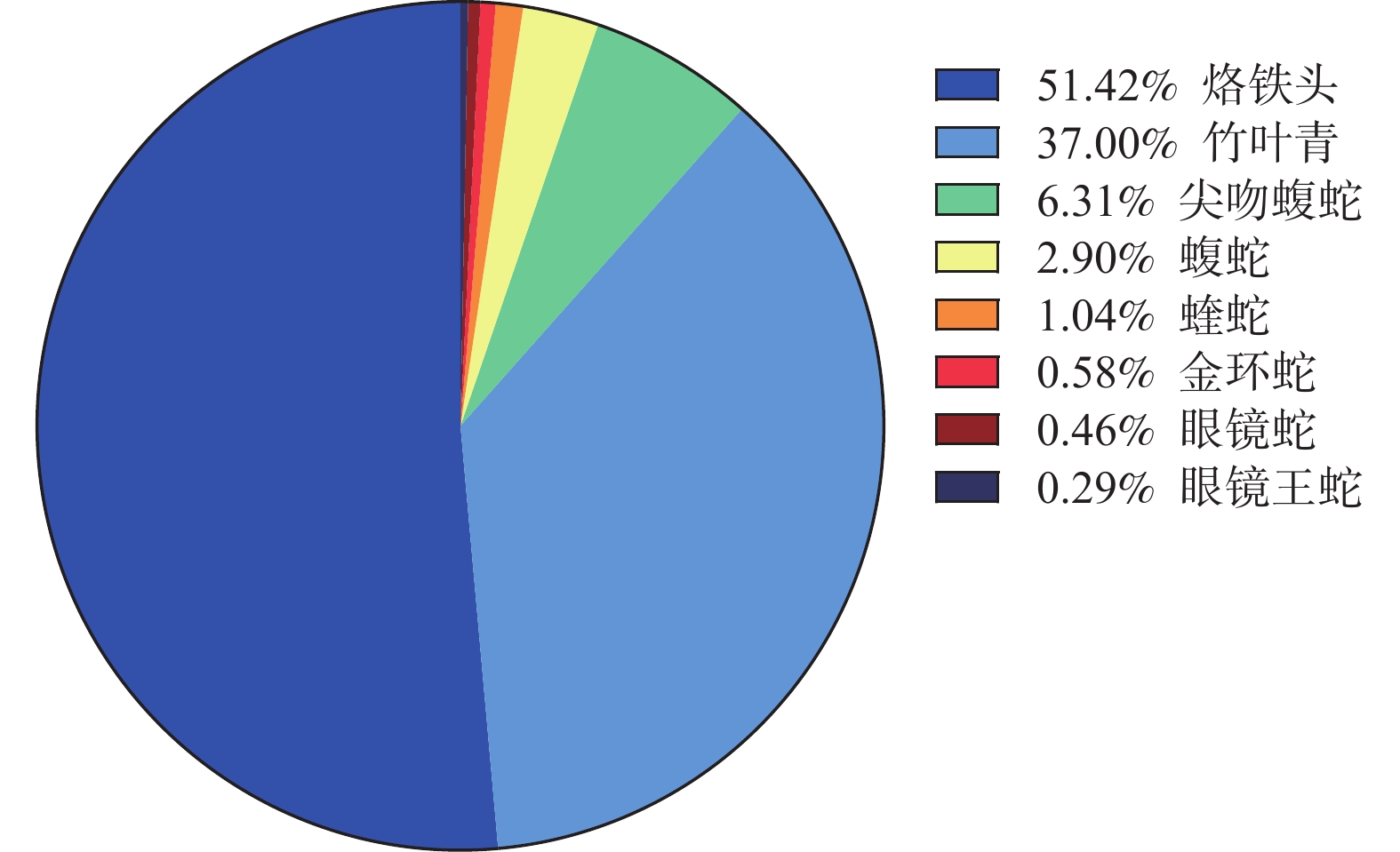
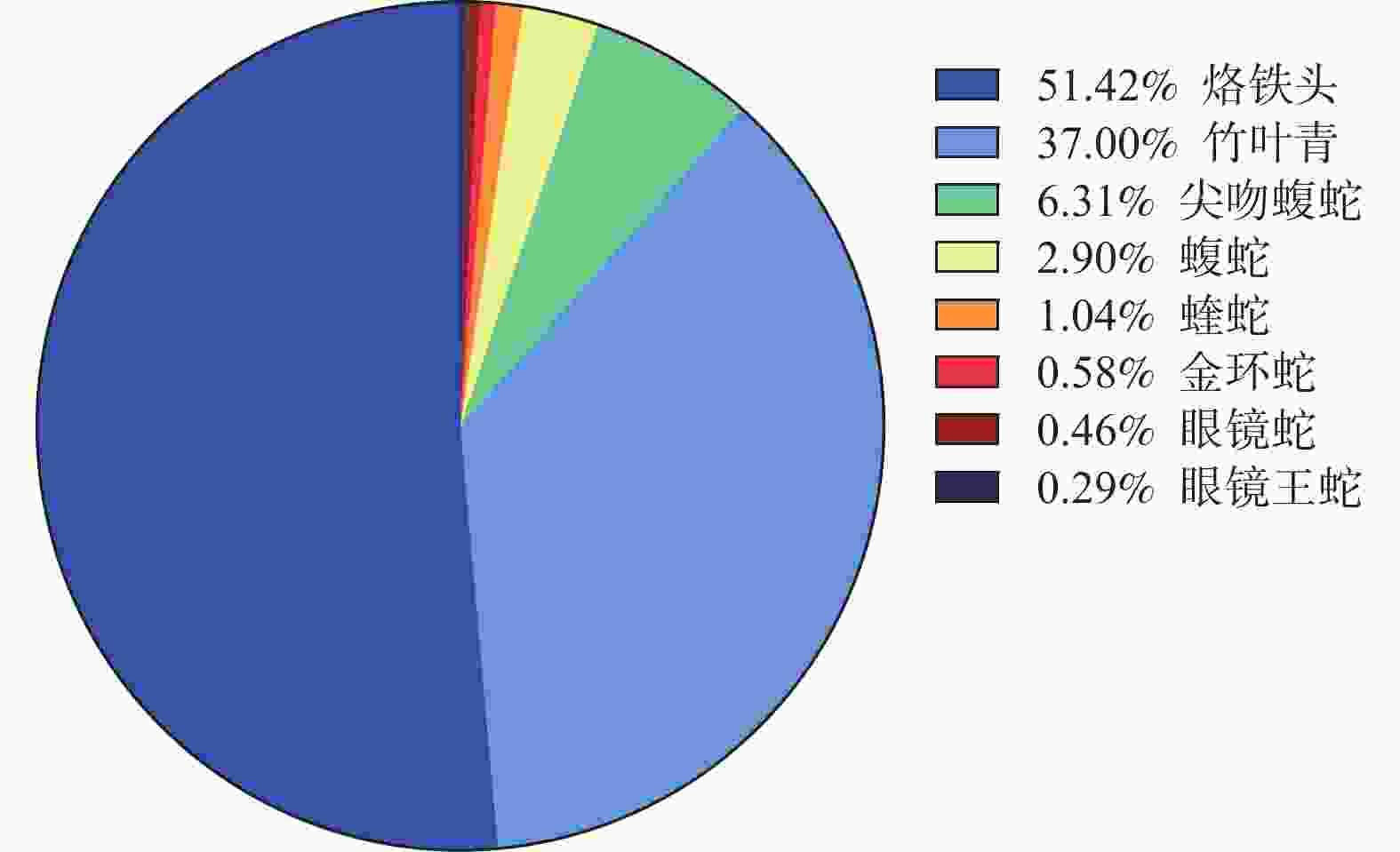
目的 探究2023-2024年云南省毒蛇咬伤的流行病学特点及治疗效果。 方法 收集云南省16个地级行政区2023年1月至2024年12月收治的 1727 例蛇伤病例资料,采用回顾性分析方法,重点考察以下指标:(1)人口学特征(年龄、性别分布);(2)伤害事件特征(发生地点、时间分布、受伤部位);(3)毒蛇种类构成;(4)临床特征与处置方案;(5)疗效评价指标(局部症状缓解时间、住院天数及随访结果)。结果 云南省蛇咬伤事件高发地区为文山(308/ 1727 )、昆明(285/1727 )、曲靖(270/1727 )、临沧(139/1727 )、保山(120/1727 )、大理(105/1727 )等,主要发生在6~9月份;最常见的毒蛇种类为以血液毒毒素为主的烙铁头蛇(Ovophis)和竹叶青蛇(Trimeresurus);咬伤人群大部分为青年;临床表现主要为疼痛和肿胀;咬伤部位主要为四肢;咬伤地点主要为山林/山地;抗蛇毒血清使用以抗五步蛇蛇毒血清为主;肿胀消退时间大多为2(2,3)d,平均住院时长为4(3,5)d;96.46%接受正规诊疗的蛇伤患者基本痊愈,随访0.35%的致残率。结论 云南省毒蛇咬伤事件具有显著的地域与季节集中性,文山、昆明、曲靖等地为高发区域,夏季6—9月是事件高峰期,且致伤蛇类以含血液毒的蛇为主;受害群体以青年为主,咬伤多发生于四肢,疼痛与肿胀为典型症状;治疗以抗五步蛇血清为主;接受正规诊疗的蛇伤患者痊愈率较高,随访致残率较低,但仍需要提高公众对蛇咬伤规范诊疗的认识。 Abstract:Objective To explore the epidemiological characteristics and treatment outcomes of venomous snake bites in Yunnan Province from 2023 to 2024. Methods A retrospective analysis was performed on 1, 727 snakebite cases collected from 16 administrative regions in Yunnan Province between January 2023 and December 2024, focusing on the following indicators: (1) demographic characteristics (age and gender distribution); (2) characteristics of injury events (location, time distribution, and affected body parts); (3) composition of venomous snake species; (4) clinical features and treatment protocols; (5) efficacy evaluation indicators (time for local symptom relief, duration of hospital stay, and follow-up results). Results High-incidence areas for snake bites in Yunnan Province included Wenshan (308/ 1727 ), Kunming (285/1727 ), Qujing (270/1727 ), Lincang (139/1727 ), Baoshan (120/1727 ), and Dali (105/1727 ), with incidents primarily occurring from June to September. The most frequently encountered venomous snake species were Ovophis and Trimeresurus, known for their hemotoxic venom. Bite victims were mainly young adults. Clinical manifestations primarily included pain and swelling, with bites mainly occurring on limbs and in mountainous or forested areas. Anti-venom treatment concentrated on anti-ancistrodon acutus serum. Swelling generally subsided within 2 (2, 3) days, with an average hospital stay of 4 (3, 5) days. 96.46% of patients receiving standardized treatment fully recovered, with a follow-up disability rate of 0.35%.Conclusion The incidents of venomous snake bites in Yunnan Province have significant regional and seasonal concentration, with Wenshan, Kunming, Qujing and other areas being high-risk areas. The peak period of incidents is from June to September in summer, and the main types of snakes causing injuries are those containing blood toxins; The victim group is mainly young people, and bites often occur in the limbs, with typical symptoms of pain and swelling; The main treatment is anti snake serum; Snake bite patients who receive formal diagnosis and treatment have a higher recovery rate and a lower follow-up disability rate, but there is still a need to raise public awareness of standardized diagnosis and treatment for snake bites. -
Key words:
- Venomous snakebite /
- Epidemiology /
- Treatment
-
表 1 2023年—2024年云南省16个州市蛇咬伤病例统计
Table 1. Statistics of snakebite cases in 16 prefectures of Yunnan Province from 2023 to 2024
地区 海拔(m) 病例(n) 性别(男/女) 昆明市 746~ 4344 285 151/134 曲靖市 695~ 4017 270 173/97 玉溪市 1500 ~1800 37 18/19 昭通市 267~ 4041 99 66/33 保山市 643~ 3655 120 43/77 丽江市 1015 ~5596 34 15/19 普洱市 317~ 3370 35 18/17 临沧市 450~ 3429 139 86/53 大理白族自治州 1340 ~4097 105 72/33 西双版纳傣族自治州 477~ 2429 63 32/31 迪庆藏族自治州 1486 ~6740 13 9/4 怒江傈僳族自治州 738~ 4000 21 12/9 文山壮族苗族自治州 400~ 2700 308 185/123 楚雄彝族自治州 691~ 2916 85 50/35 红河哈尼族彝族自治州 76~ 3074 79 46/33 德宏傣族景颇族自治州 210~ 3404 34 14/2 -
[1] Alcoba G, Sharma S K, Bolon I, et al. Snakebite epidemiology in humans and domestic animals across the Terai region in Nepal: A multicluster random survey[J]. Lancet Glob Health, 2022, 10(3): e398-e408. doi: 10.1016/S2214-109X(22)00028-6 [2] Afroz A, Siddiquea B N, Chowdhury H A, et al. Snakebite envenoming: A systematic review and meta-analysis of global morbidity and mortality[J]. PLoS Negl Trop Dis, 2024, 18(4): e0012080. doi: 10.1371/journal.pntd.0012080 [3] Ahmed S M, Ahmed M, Nadeem A, et al. Emergency treatment of a snake bite: Pearls from literature[J]. Emerg Trauma Shock, 2008, 1(2): 97-105. doi: 10.4103/0974-2700.43190 [4] Kasturiratne A, Wickremasinghe A R, De Silva N, et al. The global burden of snakebite: A literature analysis and modelling based on regional estimates of envenoming and deaths[J]. PLoS Med, 2008, 5(11): e218. doi: 10.1371/journal.pmed.0050218 [5] Liang M, Liang P, Luo W, Wu Y, et al. Epidemiological analysis of 952 venomous snake bite in Wuzhou City of Guangxi Zhuang Autonomous Region[J]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue, 2022, 34(1): 85-90. [6] Minghui R, Malecela M N, Cooke E, et al. WHO's Snakebite envenoming strategy for prevention and control[J]. Lancet Glob Health, 2019, 7(7): e837-e838. doi: 10.1016/S2214-109X(19)30225-6 [7] 李稳, 方庆, 李兴华, 等. 湖北地区毒蛇咬伤流行病学调查及随访分析[J]. 临床急诊杂志, 2023, 24(3): 131-136. [8] 王剀, 吕植桐, 王健, 等. 云南省爬行动物名录和地理区划更新[J]. 生物多样性, 2022, 30(4): 123-153. [9] Zhong G H, Chen W D, Liu Q, et al. Valid or not? Yunnan mountain snake Plagiopholis unipostocularis (Serpentes: Colubridae: Pseudoxenodontinae)[J]. Zootaxa, 2015, 4020(2): 390-396. [10] Alirol E, Sharma S K, Bawaskar H S, et al. Snake bite in South Asia: A review[J]. PLoS Negl Trop Dis, 2010, 4(1): e603. doi: 10.1371/journal.pntd.0000603 [11] 中华医学会急诊医学分会, 国家急诊质控中心, 中国医师协会急诊医师分会, 等. 中国蛇伤救治指南[J]. 中华急诊医学杂志, 2024, 33(7): 891-906. [12] 李其斌, 吕传柱, 梁子敬, 等. 2018年中国蛇伤救治专家共识[J]. 中国急救医学, 2018, 38(12): 1026-1034. [13] Hua Z. Biogeographical divergence of the flora of Yunnan, southwestern China initiated by the uplift of Himalaya and extrusion of Indochina block[J]. PLoS One, 2012, 7(9): e45601. doi: 10.1371/journal.pone.0045601 [14] Lai R, Yan S, Wang S, et al. The Chinese guideline for management of snakebites[J]. World J Emerg Med, 2024, 15(5): 333-355. doi: 10.5847/wjem.j.1920-8642.2024.076 [15] Hou S B, Yuan Z Y, Wei P F, et al. Molecular phylogeny and morphological comparisons of the genus Hebius Thompson, 1913 (Reptilia: Squamata: Colubridae) uncover a new taxon from Yunnan Province, China, and support revalidation of Hebius septemlineatus (Schmidt, 1925)[J]. Zool Res, 2021, 42(5): 620-625. doi: 10.24272/j.issn.2095-8137.2021.093 [16] 丁利, 史静耸, 王馨. 蝮蛇中国毒蛇的第一旺族[J]. 森林与人类, 2025, 5(2): 38-47. [17] Li K E, Yu M, Wu Y Y, et al. A new species of the genus Achalinus (Squamata: Xenodermatidae) from southeastern Yunnan Province, China[J]. Zootaxa, 2020, 4860(1): 4860-4866. [18] 高琴芬, 张玮, 马静怡, 等. 竹叶青蛇咬伤所致的功能障碍及诊疗策略进展[J]. 中国急救医学, 2025, 45(4): 359-364. [19] Iliyasu G, Tiamiyu A B, Daiyab F M, et al. Effect of distance and delay in access to care on outcome of snakebite in rural north-eastern Nigeria[J]. Rural Remote Health, 2015, 15(4): 3496. [20] Dehghani R, Rabani D, Panjeh Shahi M, et al. Incidence of snake bites in Kashan, Iran during an eight year period (2004-2011)[J]. Arch Trauma Res, 2012, 1(2): 67-71. doi: 10.5812/atr.6445 [21] Kumar K S, Narayanan S, Udayabhaskaran V, et al. Clinical and epidemiologic profile and predictors of outcome of poisonous snake bites - an analysis of 1, 500 cases from a tertiary care center in Malabar, North Kerala, India[J]. Int J Gen Med, 2018, 11: 209-216. doi: 10.2147/IJGM.S136153 [22] 陈伟, 俞点, 彭张玲. 福建武夷山毒蛇咬伤流行病学特征分析[J]. 蛇志, 2025, 37(2): 148-151. [23] 刘安平, 薛植瑞, 陈江华, 等. 贵州遵义地区毒蛇咬伤流行病学分析及预防救治体会[J]. 创伤外科杂志, 2025, 27(6): 430-436. [24] 李学红, 高继伟, 任魁, 等. 云南省普洱市802例毒蛇咬伤流行病学分析[J]. 蛇志, 2024, 36(2): 121-125. [25] 王长久. 季德胜蛇药治疗毒蛇咬伤的效果观察[J]. 当代医药论丛, 2019, 17(6): 173-174. [26] Seifert S A, Armitage J O, Sanchez E E. Snake envenomation[J]. Reply N Engl J Med, 2022, 386(11): 1100. [27] Hifumi T, Yamamoto A, Morokuma K, et al. Clinical efficacy of antivenom and cepharanthine for the treatment of Mamushi (Gloydius blomhoffii) bites in tertiary care centers in Japan[J]. Jpn J Infect Dis, 2013, 66(1): 26-31. doi: 10.7883/yoken.66.26 [28] Silva A, Hifumi T, Sakai A, et al. Rhabdophis tigrinus is not a pit viper but its bites result in venom-induced consumptive coagulopathy similar to many viper bites[J]. J Intensive Care, 2014, 2(1): 43. doi: 10.1186/s40560-014-0043-6 [29] Tan C H, Palasuberniam P, Tan K Y. Snake venom proteomics, immunoreactivity and toxicity neutralization studies for the asiatic mountain pit vipers, Ovophis convictus, Ovophis tonkinensis, and Hime habu, Ovophis okinavensis[J]. Toxins (Basel), 2021, 13(8): 6-13. [30] Maduwage K, Isbister G K. Current treatment for venom-induced consumption coagulopathy resulting from snakebite[J]. PLoS Negl Trop Dis, 2014, 8(10): e3220. doi: 10.1371/journal.pntd.0003220 [31] Margono F, Outwater A H, Lowery Wilson M, et al. Snakebite treatment in Tanzania: Identifying gaps in community practices and hospital resources[J]. Int J Environ Res Public Health, 2022, 19(8): 19084701. [32] Isbister G K. Antivenom availability, delays and use in Australia[J]. Toxicon X, 2023, 17(8): 100145. [33] Jeon Y J, Kim J W, Park S, et al. Risk factor, monitoring, and treatment for snakebite induced coagulopathy: A multicenter retrospective study[J]. Acute Crit Care, 2019, 34(4): 269-275. doi: 10.4266/acc.2019.00591 [34] Navaeifar M R, Zakariaei Z, Ghadiri A, et al. Compartment syndrome following snakebite in a boy: A case report and literature review[J]. Int J Surg Case Rep, 2023, 10(5): 108050. [35] Canas C A. Is the acute compartment syndrome diagnosed in snake bites true?: A review[J]. Medicine (Baltimore), 2024, 103(40): e40008. [36] Luo Y, Zhang J, Zhai C, et al. Clinical study on the application of covered vacuum sealing drainage technology to the bite of venomous snakes of trimeresurus stejnegeri in Guangxi[J]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue, 2020, 32(10): 1241-1246. [37] 林起庆, 何斌, 李峥. 小切口负压治疗对竹叶青蛇咬伤后肢体肿胀和凝血功能的影响[J]. 蛇志, 2018, 30(3): 396-398. [38] Faisal T, Tan K Y, Tan N H, et al. Proteomics, toxicity and antivenom neutralization of Sri Lankan and Indian Russell's viper (Daboia russelii) venoms[J]. J Venom Anim Toxins Incl Trop Dis, 2021, 27(30): e20200177. [39] Abraham S V, Hakkeem B, Mathew D, et al. Hematotoxic snakebite victim with trauma: The role of guided transfusion, rotational thromboelastometry, and tranexamic acid[J]. Wilderness Environ Med, 2020, 31(4): 470-481. doi: 10.1016/j.wem.2020.08.003 [40] Holla S K, Rao H A, Shenoy D, et al. The role of fresh frozen plasma in reducing the volume of anti-snake venom in snakebite envenomation[J]. Trop Doct, 2018, 48(2): 89-93. doi: 10.1177/0049475518756083 [41] Qian X H, Ma L. Fibrinolytic enzyme from Agkistrodon halys brevicaudus (Korean mamushi) snake venom[J]. Toxicon, 1991, 29(11): 1381-1386. doi: 10.1016/0041-0101(91)90125-B -





 下载:
下载: