Survey on Mental Disorders in HIV/AIDS Patients with End-stage Renal Disease on Hemodialysis
-
摘要:
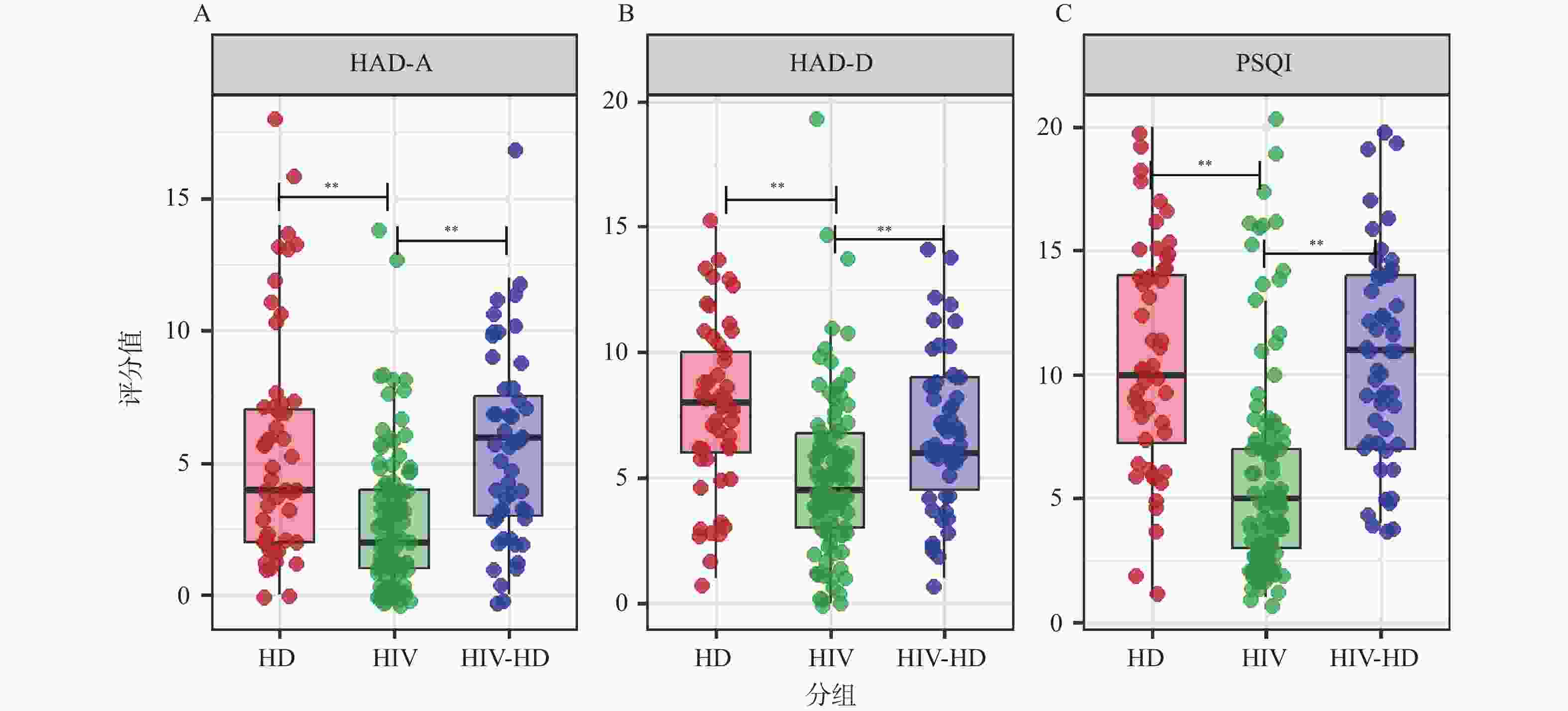
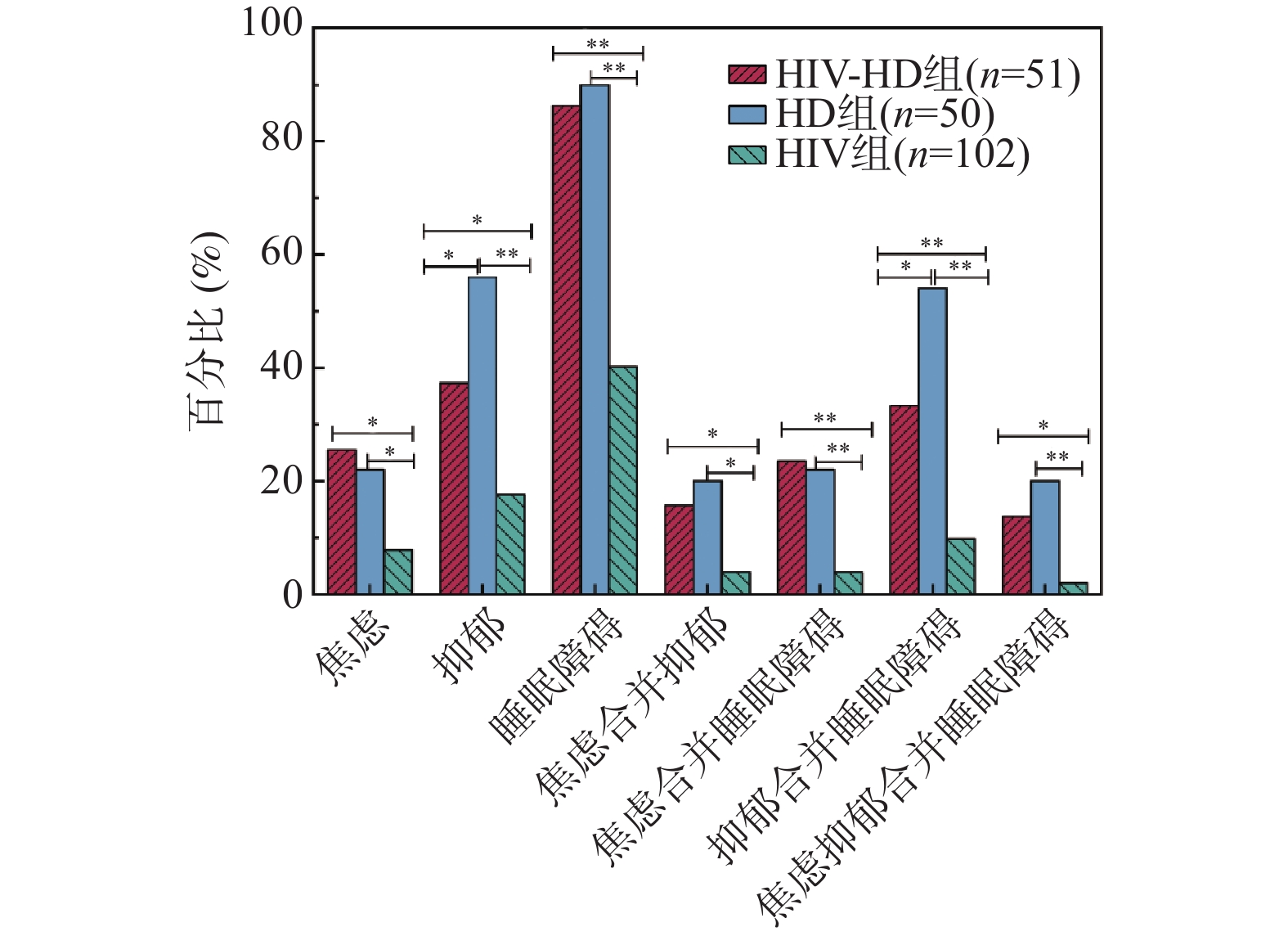
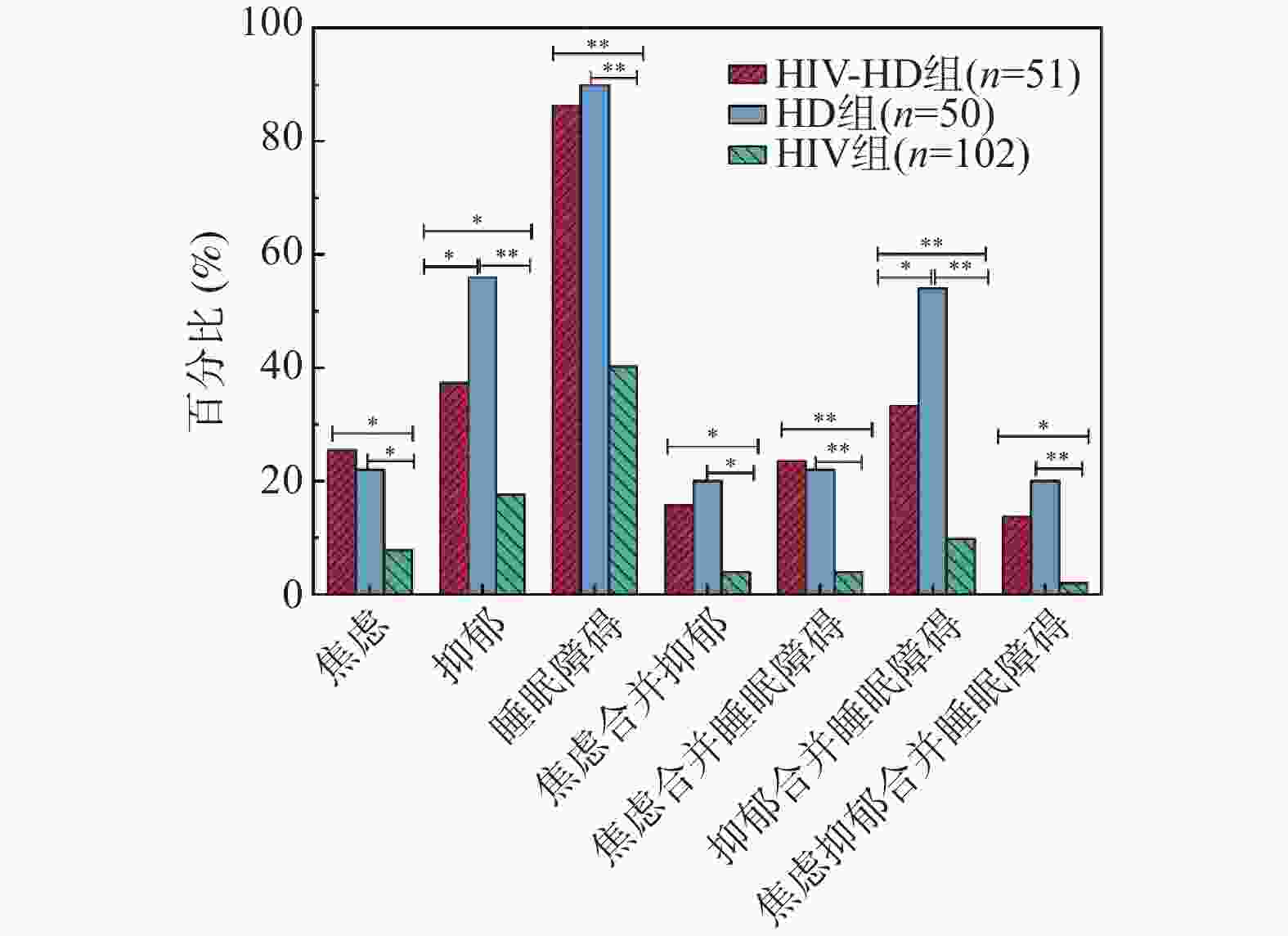
目的 了解HIV/AIDS合并终末期肾病(end-stage renal disease,ESRD)患者行维持性血液透析(maintenance hemodialysis,MHD)期间焦虑、抑郁及睡眠障碍的发病情况及临床特征。 方法 采用横断面研究设计,连续纳入2024年8月至12月在昆明市第三人民医院治疗的51例HIV/AIDS合并ESRD行MHD患者为HIV-HD组、50例普通ESRD行MHD患者为HD组及按1∶2随机抽取的102例未透析HIV感染者为HIV组。使用医院焦虑抑郁量表(hospital anxiety and depression scale,HADS)和匹兹堡睡眠质量指数(Pittsburgh sleep quality index,PSQI)分别评估患者的焦虑抑郁及睡眠障碍,比较三组发病情况。 结果 共纳入203例患者。HIV-HD组、HD组、HIV组精神障碍发病率分别为:焦虑(25.5% vs. 22.0% vs. 7.8%)、抑郁(37.3% vs. 56.0% vs. 17.6%)、睡眠障碍(86.3% vs. 90.0% vs. 40.2%)、焦虑合并抑郁(15.7% vs. 20.0% vs. 3.9%)、焦虑合并睡眠障碍(23.5% vs. 22.0% vs. 3.9%)、抑郁合并睡眠障碍(33.3% vs. 54.0% vs. 9.8%)、焦虑抑郁合并睡眠障碍(13.7% vs. 20.0% vs. 2.0%),HIV-HD组与HD组上述精神障碍发生率均显著高于HIV组(P < 0.05)。临床特征显示,HIV-HD组与HD组严重合并症(CCI≥5分)、高血压比例显著高于HIV组,HD组糖尿病患病率高于HIV组(P均< 0.05)。 结论 HIV/AIDS血液透析患者存在较高的焦虑、抑郁发病率,且睡眠质量极差。 Abstract:Objective To investigate the incidence and clinical characteristics of anxiety, depression, and sleep disorders in people living with HIV (PLWH) and end-stage renal disease (ESRD) on maintenance hemodialysis (MHD). Methods A cross-sectional study was conducted at Kunming Third People’ s Hospital from August to December 2024. We consecutively enrolled 51 HIV/AIDS patients with ESRD receiving MHD (HIV-HD group), 50 non-HIV ESRD patients receiving MHD (HD group), and randomly selected 102 non-dialysis PLWH at a 1∶2 ratio (HIV group). The hospital anxiety and depression scale (HADS) was used to assess anxiety and depression, and the Pittsburgh sleep quality index (PSQI) was used to evaluate sleep quality. The incidence rates of these conditions were compared among the three groups. Results A total of 203 patients were included. The incidence rates of psychiatric disorders in HIV-HD, HD , and HIV groups were as follows: anxiety (25.5% vs. 22.0% vs. 7.8%), depression (37.3% vs. 56.0% vs. 17.6%), sleep disorders (86.3% vs. 90.0% vs. 40.2%), comorbid anxiety and depression (15.7% vs. 20.0% vs. 3.9%), comorbid anxiety and sleep disorders (23.5% vs. 22.0% vs. 3.9%), comorbid depression and sleep disorders (33.3% vs. 54.0% vs. 9.8%), and comorbid anxiety, depression, and sleep disorders (13.7% vs. 20.0% vs. 2.0%). The incidence of these psychiatric disorders was significantly higher in both the HIV-HD and HD groups compared to the HIV group (P < 0.05). Clinical characteristics revealed that the proportions of severe comorbidities (CCI≥5) and hypertension were significantly higher in the HIV-HD and HD groups than in the HIV group, while the prevalence of diabetes was higher in the HD group than in the HIV group (all P < 0.05). Conclusion People living with HIV on hemodialysis have a higher incidence of anxiety and depression, and extremely poor sleep quality. -
Key words:
- HIV/AIDS /
- Maintenance hemodialysis /
- Anxiety /
- Depression /
- Sleep disorders
-
表 1 三组患者一般社会人口学资料对比[($\bar x \pm s$)/n(%)]
Table 1. Comparison of general sociodemographic characteristics among the three patient groups[($\bar x \pm s$)/n(%)]
项目 占比 HIV-HD组(n=51) HD组(n=50) HIV组(n=102) χ2/t/F P 性别 男 133(65.5) 31(60.8) 40(80.0) 62(60.8) 6.159 0.046* 女 70(34.5) 20(39.2) 10(20.0) 40(39.2) 年龄(岁) 50.34 ± 10.43 48.31 ± 9.32 51.82 ± 13.80 50.63 ± 8.893 1.492 0.23 民族 汉族 166(81.8) 34(66.7) 43(86.0) 89(87.3) 10.465 0.005* 少数民族 37(18.2) 17(33.3) 7(14.0) 13(12.7) BMI(kg/m2) 22.37 ± 3.59 22.03 ± 4.07 22.55 ± 3.90 22.45 ± 3.17 0.323 0.724 文化程度 小学及以下 71(35.0) 24(47.1) 11(22.0) 36(35.3) 9.543 0.145 初中 69(34.0) 14(27.5) 17(34.0) 38(37.3) 高中及中专 34(16.7) 8(15.7) 12(24.0) 14(13.7) 本科及以上 29(14.3) 5(9.8) 10(20.0) 14(13.7) 婚姻状况 未婚/离异 62(30.5) 15(29.4) 14(28.0) 33(32.4) 0.341 0.843 已婚 141(69.5) 36(70.6) 36(72.0) 69(67.6) 家庭人均月收入(元) ≤ 3000 148(72.9) 44(86.3) 37(74.0) 67(65.7) 7.336 0.026* > 3000 55(27.1) 7(13.7) 13(26.0) 35(34.3) 居住地 农村 68(33.5) 20(39.2) 12(24.0) 36(35.3) 2.921 0.232 城市 135(66.5) 31(60.8) 38(76.0) 66(64.7) 职业 无稳定工作 88(43.3) 30(58.8) 20(40.0) 38(37.3) 6.744 0.034* 有稳定工作 115(56.7) 21(41.2) 30(60.0) 64(62.7) 吸烟史 是 111(54.7) 26(51) 30(60.0) 55(53.9) 0.876 0.645 否 92(45.3) 25(49) 20(40.0) 47(46.1) 饮酒史 是 63(31.0) 19(37.3) 17(34.0) 27(26.5) 2.12 0.346 否 140(69.0) 32(62.7) 33(66.0) 75(73.5) 吸毒史 是 30(14.8) 8(15.7) 2(4.0) 20(19.6) 6.534 0.038* 否 173(85.2) 43(84.3) 48(96.0) 82(80.4) 就诊期间是否有人陪同 是 49(24.1) 11(21.6) 14(28.0) 24(23.5) 0.612 0.736 否 154(75.9) 40(78.4) 36(72.0) 78(76.5) CCI(分) 0~2 89(43.8) 8(15.7) 5(10.0) 76(74.5) 85.115 <0.001** 3~4 35(17.2) 8(15.7) 17(34.0) 10(9.8) ≥5 79(38.9) 35(68.6) 28(56.0) 16(15.7) 高血压 是 85(41.9) 28(54.9) 31(62.0) 26(25.5) 23.127 <0.001** 否 118(58.1) 23(45.1) 19(38.0) 76(74.5) 糖尿病 是 31(15.3) 10(19.6) 13(26.0) 8(7.8) 9.539 0.008* 否 172(84.7) 41(80.4) 37(74.0) 94(92.2) 高脂血症 是 26(12.8) 3(5.9) 3(6.0) 20(19.6) 8.498 0.014* 否 177(87.2) 48(94.1) 47(94.0) 82(80.4) 高尿酸血症 是 45(22.2) 23(45.1) 19(38.0) 29(28.4) 4.42 0.11 否 158(77.8) 28(54.9) 31(62.0) 73(71.6) *P < 0.05;**P < 0.001。 表 2 HIV-HD组和HD组临床特征对比[($\bar x \pm s$)/n(%)]
Table 2. Comparison of clinical characteristics between the HIV-HD group and the HD group[($\bar x \pm s$)/n(%)]
项目 HIV-HD组(n=51) HD组(n=50) χ2/t P 充血性心力衰竭 是 22(43.1) 17(34.0) 0.889 0.346 否 29(56.9) 33(66.0) 周围血管疾病 是 3(5.9) 2(4.0) 0.191 0.662 否 48(94.1) 48(96.0) 脑血管疾病 是 1(2.0) 2(4.0) 0.371 0.543 否 50(98.0) 48(96.0) 慢性肺部疾病 是 22(43.1) 20(40.0) 0.102 0.749 否 29(56.9) 30(60.0) 轻度肝脏疾病 是 8(15.7) 9(18.0) 0.097 0.756 否 43(84.3) 41(82.0) 糖尿病伴器官损害 是 2(3.9) 3(6.0) 0.233 0.629 否 49(96.1) 47(94.0) 中度和重度肝脏疾病 是 4(7.8) 7(14.0) 0.986 0.321 否 47(92.2) 43(86.0) 透析龄(年) 2.63 ± 2.753 2.10 ± 1.930 1.25 0.266 透析频率 1~2次/周 22(43.1) 29(58.0) 2.231 0.135 3次及以上/周 29(56.9) 21(42.0) 表 3 HIV-HD组和HIV组临床特征对比[($\bar x \pm s$)/n(%)]
Table 3. Comparison of clinical characteristics between the HIV-HD group and the HIV group[($\bar x \pm s$)/n(%)]
项目 HIV-HD组(n=51) HIV组(n=102) χ2/t P 抗病毒治疗时间(年) 7.55 ± 4.356 9.15 ± 4.896 −1.973 0.049* 抗病毒治疗药物(第三类药物) INSTI 38(74.5) 34(33.3) − <0.001** NNRTI 4(7.8) 51(50.0) PI 6(11.8) 17(16.7) INSTI+PI 2(3.9) 0(0.0) NNRTI+PI 1(2.0) 0(0.0) 感染途径 性传播 44(86.3) 82(80.4) 0.81 0.368 注射吸毒 7(13.7) 20(19.6) HIVRNA 低于检测限 40(78.4) 87(85.3) 1.135 0.287 高于检测限 11(21.6) 15(14.7) CD4+T细胞计数(个/μL) <350 25(49.0%) 29(28.4%) 6.311 0.012* ≥350 26(51.0%) 73(71.6%) *P < 0.05;**P < 0.001;NNRTI:非核苷类反转录酶抑制剂;INSTI:整合酶抑制剂;PI:蛋白酶抑制剂。 -
[1] UNAIDS. Global HIV Statistics 2023 [Internet][EB/OL]. (2024 Jul 15) https://www.unaids.org/sites/default/files/media_asset/UNAIDS-global-report-2023_en.pdf. [2] 中国疾病预防控制中心性病艾滋病预防控制中心. 2024年12月全国艾滋病性病疫情[J]. 中国艾滋病性病, 2025, 31(3): 225. [3] Lucas A, Wyatt C M. HIV at 40: Kidney disease in HIV treatment, prevention, and cure[J]. Kidney Int, 2022, 102(4): 740-749. doi: 10.1016/j.kint.2022.06.021 [4] Duan J Y, Duan G C, Wang C J, et al. Prevalence and risk factors of chronic kidney disease and diabetic kidney disease in a central Chinese urban population: A cross-sectional survey[J]. BMC Nephrol, 2020, 21(1): 115. doi: 10.1186/s12882-020-01761-5 [5] Yang Y, Liang W, Gong W, et al. Establishment and evaluation of a nomogram prediction model for the risk of vascular calcification in stage 5 chronic kidney disease patients[J]. Sci Rep, 2024, 14(1): 1025. doi: 10.1038/s41598-023-48275-2 [6] Mazuecos A, Rodriguez Benot A, Moreno A, et al. Renal replacement therapy in patients with HIV infection in a European region: Outcomes following renal transplantation[J]. Transplantation Proceedings, 2012, 44(7): 2053-2056. doi: 10.1016/j.transproceed.2012.07.082 [7] Yan H, Li X, Li J, et al. Association between perceived HIV stigma, social support, resilience, self-esteem, and depressive symptoms among HIV-positive men who have sex with men (MSM) in Nanjing, China[J]. AIDS Care, 2019, 31(9): 1069-1076. doi: 10.1080/09540121.2019.1601677 [8] Zaragoza-Fernandez G M, De La Flor J C, Fernandez Abreu V, et al. Comparison of depression in hemodialysis, peritoneal dialysis, and kidney transplant patients: A systematic review with meta analysis[J]. J Pers Med, 2025, 15(5): 179. doi: 10.3390/jpm15050179 [9] 张洋, 孙广强, 贾琳. 中国成人HIV感染合并抑郁的诊疗与管理专家共识[J]. 中国艾滋病性病, 2025, 31(2): 113-126. [10] Anderson A M, Ma Q, Letendre S L, et al. Soluble biomarkers of cognition and depression in adults with HIV infection in the combination therapy era[J]. Curr HIV/AIDS Rep, 2021, 18(6): 558-568. doi: 10.1007/s11904-021-00581-y [11] Turon-Skrzypinska A, Tomska N, Mosiejczuk H, et al. Impact of virtual reality exercises on anxiety and depression in hemodialysis[J]. Sci Rep, 2023, 13(1): 12435. doi: 10.1038/s41598-023-39709-y [12] 周张青, 崔龚臻, 汪雪芬, 等. AIDS血液透析患者抑郁影响因素分析[J]. 中国现代医生, 2024, 62(36): 56-59. doi: 10.3969/j.issn.1673-9701.2024.36.012 [13] Bedaso A, Abraham Y, Temesgen A, et al. Quality of sleep and associated factors among people living with HIV/AIDS attending ART clinic at Hawassa University comprehensive specialized Hospital, Hawassa, SNNPR, Ethiopia[J]. PLoS One, 2020, 15(6): 23-28. [14] 谭旭妍, 张雪, 李央, 等. 维持性血液透析病人睡眠质量现状及其影响因素调查[J]. 全科护理, 2024, 22(13): 2532-2535. doi: 10.12104/j.issn.1674-4748.2024.13.037 [15] 沈银忠. 中国艾滋病诊疗指南(2024版)[J]. 中国病毒病杂志, 2025, 15(1): 4-32. [16] Gong Y, Zhao Y, Ran L, et al. Comparison between hemodialysis and peritoneal dialysis in the risks for disease activity in LN-ESRD patients: A systematic review and meta-analysis[J]. Altern Ther Health Med, 2022, 28(6): 144-149. [17] 陈美凤, 程小娟. 家属参与下的护理模式对慢性肾衰竭血液透析患者心态及睡眠质量的影响[J]. 基层医学论坛, 2025, 29(12): 86-89. [18] Remien R H, Stirratt M J, Nguyen N, et al. Mental health and HIV/AIDS: The need for an integrated response[J]. Aids, 2019, 33(9): 1411-1420. doi: 10.1097/QAD.0000000000002227 [19] 詹思延. 流行病学[M]. 第8版. 北京: 人民卫生出版社, 2017: 83-85. [20] 王丽军. 经典型骨髓增殖性肿瘤患者焦虑抑郁障碍发生及影响因素研究[D]. 山西: 山西医科大学, 2023. [21] 黄小捷. 患者健康问卷与医院焦虑抑郁量表在抑郁人群中的适用性及其等值性研究[D]. 广州: 南方医科大学, 2022. [22] Farah N M, Saw Yee T, Mohd Rasdi H F. Self-reported sleep quality using the malay version of the Pittsburgh sleep quality index (PSQI-M) in malaysian adults[J]. Int J Environ Res Public Health, 2019, 16(23): 4750. doi: 10.3390/ijerph16234750 [23] 张永海. 基于匹兹堡睡眠质量指数探究睡眠状况对冠心病的影响及相关因素分析[D]. 宁夏: 宁夏医科大学, 2024. [24] 刘云峰, 刘红艳, 孙静, 等. 中央型肺栓塞短期不良预后危险因素及Charlson合并症指数的预测价值[J]. 安徽医科大学学报, 2024, 59(9): 1643-1647. [25] 严涓, 陈海平, 喻剑华, 等. 杭州市艾滋病患者的抑郁和焦虑情绪[J]. 中国心理卫生杂志, 2022, 36(4): 308-312. doi: 10.3969/j.issn.1000-6729.2022.04.006 [26] Ayano G, Demelash S, Abraha M, et al. The prevalence of depression among adolescent with HIV/AIDS: A systematic review and meta-analysis[J]. AIDS Res Ther, 2021, 18(1): 23. doi: 10.1186/s12981-021-00351-1 [27] 马荣荣, 邓思妍, 赵娟, 等. 维持性血液透析患者睡眠质量的潜在类别分析及影响因素探讨[J]. 中国血液净化, 2025, 24(2): 172-176. [28] Wang J, Wu J, Liu J, et al. Prevalence of sleep disturbances and associated factors among Chinese residents: A web-based empirical survey of 2019[J]. J Glob Health, 2023, 13: 04-07. [29] Muvenda T, Williams A A, Williams M E. Transactivator of transcription (Tat)-induced neuroinflammation as a key pathway in neuronal dysfunction: A scoping review[J]. Mol Neurobiol, 2024, 61(11): 9320-9346. doi: 10.1007/s12035-024-04173-w [30] Bossola M, Picconi B. Uremic toxins and the brain in chronic kidney disease[J]. J Nephrol, 2024, 37(5): 1391-1395. doi: 10.1007/s40620-024-01929-4 [31] Yang Y, Chen B, Zhang H, et al. Global prevalence of depressive symptoms among people living with HIV/AIDS: A systematic review and meta-analysis of the past five years[J]. AIDS Care, 2024, 36(2): 153-164. doi: 10.1080/09540121.2023.2285733 [32] 曾点点, 金永梅, 田波, 等. 艾滋病抗病毒治疗患者焦虑、抑郁及睡眠障碍发生情况及影响因素分析[J]. 大理大学学报, 2023, 8(4): 86-91. doi: 10.3969/j.issn.2096-2266.2023.04.017 [33] Jorgensen J R, Mohr W, Rischer M, et al. Stability and intrinsic dissolution of vacuum compression molded amorphous solid dispersions of efavirenz[J]. Int J Pharm, 2023, 63(2): 122564. [34] Wang N, Wang M, Xin X, et al. Exploring the relationship between anxiety, depression, and sleep disturbance among HIV patients in China From a network perspective[J]. Front Psychiatry, 2021, 12(7): 46-64. [35] Ranzani A, Castelli F, Di Biagio A, et al. Influence of efavirenz and 8-hydroxy-efavirenz plasma levels on cognition and central nervous system side effects[J]. HIV Med, 2024, 25(4): 491-497. doi: 10.1111/hiv.13600 [36] Elendu C, Aguocha C M, Okeke C V, et al. HIV-related neurocognitive disorders: Diagnosis, treatment, and mental health implications: A Review[J]. Medicine (Baltimore), 2023, 102(43): 35-52. [37] 路畅. 终末期肾脏病不同透析方式患者抑郁情况及相关因素的研究[D]. 长春: 长春中医药大学, 2023. [38] Squillace N, Ricci E D, Orofino G, et al. Neuropsychiatric adverse events in people with HIV initiating a new integrase strand transfer inhibitor-based regimen in Italy: findings from the NEURO-INSTI study[J]. BMC Infect Dis, 2025, 25(1): 763. doi: 10.1186/s12879-025-11090-3 [39] Tang X, Wang L, Ni S, et al. Feasibility and effect of emotional freedom therapy on sleep quality in patients with end-stage renal disease receiving maintenance hemodialysis: A pilot study[J]. Geriatr Nurs, 2023, 51(1): 112-120. -





 下载:
下载: