Clinical Characteristics and Polymorphism of UGT1A1 Gene in 53 Cases of Congenital Hyperbilirubinemia in Yunnan
-
摘要:
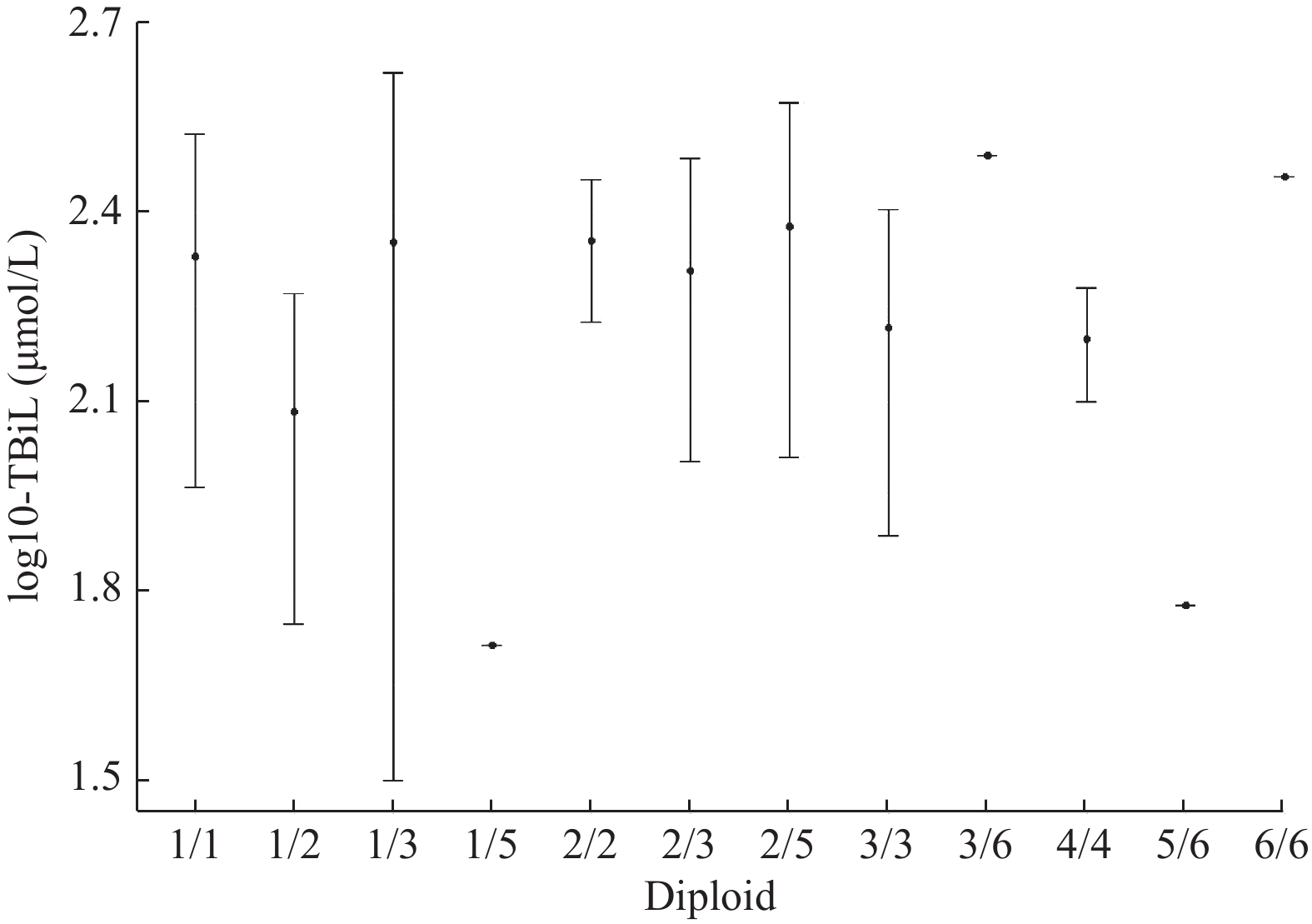
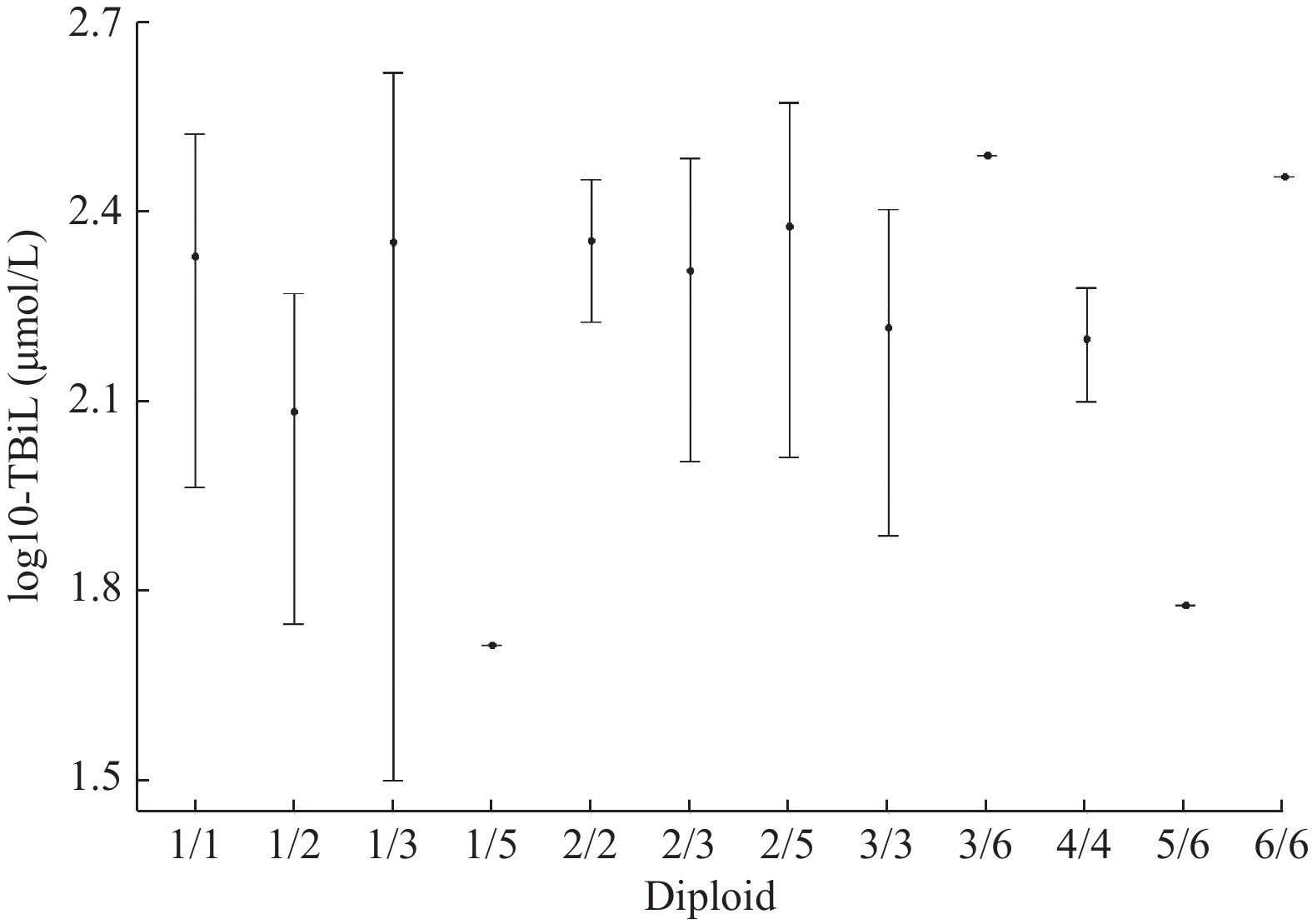
目的 探讨云南地区53例UGT1A1基因突变所致的先天性高胆红素血症(Gilbert 综合征、Crigler - Najjar 综合征)的临床特征及UGT1A1基因突变特点。 方法 选取2017年1月至2022年12月间昆明市儿童医院消化内科53例Gilbert 综合征(GS组)、 Crigler - Najjar Ⅱ 型综合征(CN-2组)患儿的临床数据、UGT1A1基因突变结果,回顾性分析患儿的临床特征、实验室检查结果和基因多态性。 结果 少数民族患儿均在2组中发病率较高,CN-2组中女性比例比GS高。肝脏系统方面,CN-2组TBil、IDB水平较GS组更高,差异均有统计学意义(P < 0.05),GS组肝脏结构正常,CN-2组有3例患者肝胆结构有异常。肝外系统方面,血液系统、糖代谢无异常,血脂、甲状腺功能代谢有异常,GS组有维生素D不足,CN-2组存在维生素A、D缺乏及维生素E水平下降。2组患儿均存在心脏结构异常,但CN-2组较GS组发病率高。在所有患者中,突变频率最高的为发生在5号外显子上的c.1456T>G(32例,60.37%),其次为c.1091C>T(14例,26.42%)、1号外显子c.211G>A(6例,11.32%)和c.1198A>C(4例,7.55%)。c.1456T>G位点突变在GS组和CN-2组的频率分别为69.23%和57.5%(9例和23例),2组间差异无统计学意义(P > 0.05)。2组中,其次突变频率较高的为c.1091C>T(4例和10例),2组间差异无统计学意义(P > 0.05)。UGT1A1基因单倍型1、3、4在GS 组和CN-2组间的频率差异均有统计学意义 ( P < 0.05) 。UGT1A1基因的4种主要突变形式,在性别和不同民族间,差异无统计学意义(P > 0.05)。 结论 GS 组和CN-2组在肝脏系统、肝外系统的临床表现存在不同,UGT1A1基因突变频率最高的为发生在5号外显子上的c.1456T>G。 -
关键词:
- Gilbert综合征 /
- Crigler-Najjar综合征 /
- 血清总胆红素 /
- UGT1A1 /
- 基因型
Abstract:Objective To investigate the clinical characteristics of 53 cases of congenital hyperbilirubinemia (Gilbert syndrome, Crigler-Najjar syndrome) caused by UGT1A1 gene mutation in Yunnan Province and the characteristics of UGT1A1 gene mutation. Methods 53 cases were selected from the Department of Gastroenterology of Kunming Children’ s Hospital from January 2017 to December 2022 and divided into Gilbert syndrome (GS) group and Crigler-Najjar-2 (GN-2)group. The clinical data and genetic test results of children with type I1 syndrome (CN-2 group)and the clinical manifestations, laboratory test results and gene polymorphisms of the children were retrospectively analyzed. Results Children from the ethnic minority had the higher incidence in both groups. The proportion of females in CN-2 group was higher than that in GS group. In terms of liver system, the levels of TBil and IDB in CN-2 group were higher than those in GS group, with statistical significance (all P values < 0.05). The liver structure in GS group was normal, while 3 patients in CN-2 group had the abnormal liver and biliary structure. In the extra-hepatic system, there were no abnormalities in blood system and glucose metabolism, abnormal blood lipids and thyroid function metabolism, vitamin D deficiency in GS group, vitamin A and D deficiency and vitamin E decreased in CN-2group. There were cardiac structural abnormalities in both groups, but the incidence of CN-2 group was higher than that of GS group. Among all the patients, the mutation frequency of c.1456T>G in exon 5 was the highest (32 cases, 60.37%), followed by c.1091C>T (14 cases, 60.37%). Exon 1, C.211g>A (6 cases, 11.32%), and C.1198a >C (4 cases, 7.55%). The frequency of c.1456T>G mutation in GS group and CN-2 group was 69.23% and 57.5%(9 and 23 cases), respectively, and there was no significant difference between the two groups (P > 0.05). Among the two groups, the second most frequent mutation was c.1091C>T (4 cases and 10 cases), and there was no statistical significance between the two groups (P > 0.05).The frequencies of UGT1A1 haplotypes 1、3 and 4 were statistically significant between GS group and CN-2 group (P < 0.05). There is no significant difference in gender and ethnic groups among the four major mutation forms of UGT1A1 (P > 0.05). Conclusion The clinical manifestations of the liver system and extrahepatic system are different between GS group and CN-2 group. The highest mutation frequency of UGT 1A1 gene is c.1456T>G in exon 5. -
表 1 GS组与CN-2临床资料对比[n(%)/($\bar x \pm s $),n=53]
Table 1. Comparison of clinical data between GS group and CN-2 group [n(%)/($\bar x \pm s $),n=53]
资料 GS组(n=13) CN-2组(n=40) t/χ2 P 发病年龄(d) 3.00(5.00) 3.00(1.00) −0.240 0.811 胎龄(周) 37.33±3.39 39.20±1.37 −1.941 0.074 出生体重(kg) 2.85±0.68 3.19±0.28 −1.760 0.101 性别 男 9(69.2) 19(47.5) 1.859 0.173 女 4(30.8) 21(52.5) 喂养方式 母乳喂养 7(50.0) 21(50.0) 1.780 0.411 代乳品 3(25.0) 4(10.0) 混合喂养 3(25.0) 15(40.0) 民族 汉族 6(46.2) 19(47.5) 0.467 0.495 少数民族 7(53.8) 21(52.5) 表 2 GS组与CNS-2生化检测结果及对比[($\bar x \pm s $)/n(%),n=53]
Table 2. Results of biochemical detection and comparison between GS group and CNS-2 [($\bar x \pm s $)/n(%),n=53]
资料 GS组(n=13) CN-2组(n=40) t/z P 血红蛋白(g/L) 119.42±18.57 120.53±19.64 −0.173 0.863 WBC(×109/L) 8.03±2.69 8.37±2.64 −0.408 0.685 C 反应蛋白(mg/L) 0.50(0) 0.50(0.05) −0.958 0.338 网织红细胞绝对值(×109/L) 0.037(0.049) 0.045(0.042) −1.319 0.187 ALT( U/L) 25.50(69.50) 19.00(27.00) −0.796 0.426 TBil( μmol /L) 61.85±22.09 231.44±88.20 −10.621 <0.001* IDB( μmol /L) 50.20(46.40) 198.65(124.90) −5.292 <0.001* DB( μmol /L) 8.3(7.5) 9.30(6.3) −0.145 0.885 AKP(μmol /L) 336.00(173.5) 294.50(173.3) −1.044 0.296 TBA(g/L) 11.50(49.2) 10.95(20.6) −0.538 0.591 ALB(g/L) 41.42±3.95 40.54±4.15 0.678 0.501 APTT(S) 41.33±5.79 37.59±8.13 1.352 0.184 PT(S) 13.83±2.42 13.26±2.74 0.588 0.560 FIB(g/L) 2.23±0.61 2.25±0.42 −0.107 0.915 总胆固醇(mmol/L) 3.57±0.94 3.28±0.82 0.880 0.385 甘油三酯(mmol/L) 1.04(1.05) 0.63(0.78) −1.666 0.096 血糖(mmol/L) 4.54±0.58 4.82±0.78 −1.131 0.264 血氨(μmol/L) 29.83±9.40 34.96±17.01 −0.944 0.351 甲胎蛋白(ng/mL) 190.02(463.11) 52.24(740.80) −0.643 0.520 T3(nmol/L) 2.50(0.75) 2.26(0.40) −1.757 0.079 游离T4(pmol/L) 17.54±3.44 20.45±11.32 −0.871 0.388 TSH(mIU/L) 3.82±2.17 3.91±2.42 −0.124 0.902 维生素A(μmol/L) 2.05(5.87) 1.78(1.15) −0.415 0.678 维生素D(nmol/L) 121.16±49.45 90.66±41.53 1.896 0.066 维生素E(μmol/L) 30.40±11.75 29.40±7.47 0.245 0.808 心脏彩超 正常 9(69.2) 21(30.8) 1.118 0.29 异常 4(30.8) 19(47.5) 肝脏B超 正常 13(100) 37(90.0) − 0.567 异常 0(0) 3(10.0) *P < 0.001。 表 3 2组UGT1A1 基因突变位点基因型与等位基因频率分布比较[n(%)]
Table 3. Comparison of genotype and allele frequency distribution of DGTIA1 gene mutation sites between the two groups [n(%)]
突变位点 GS组(n=13) CN-2组(n=40) χ2 P c.1456T>G 9(69.23) 23(57.5) 0.18053 0.6709 c.1305-229A>C 1(7.69) 0 c.1198A>C 2(15.38) 2(5) 0.39326 0.5306 c.1091C>T 4(30.77) 10(25) 0.002287 0.9619 c.686C>A 1(7.69) 0 c.626G>A 1(7.69) 0 c.211G>A 1(7.69) 5(12.5) 5.90E-30 1 c.1348C>G 1(7.69) 0 c.1012C>T 0 1(2.5) c.1047delG 0 1(2.5) c.1115_1116insC 0 1(2.5) c.1211T>A 0 1(2.5) c.1352C>T 0 1(2.5) c.1447T>G 0 1(2.5) c.1454_1459delins
TGGTACCAGTCCA0 1(2.5) c.1461-1462del 0 1(2.5) c.1462G>A 0 1(2.5) c.1470C>T 0 1(2.5) c.1471G>A 0 1(2.5) c.164A>G 0 1(2.5) c.527C>T 0 1(2.5) c.610A>G 0 1(2.5) c.715C>T 0 1(2.5) c.865-157C>A 0 1(2.5) c.997-37T>C 0 1(2.5) 表 4 UGT1A1基因不同变异间的 LD 分析
Table 4. LD analysis between different variants of UGTIA1 gene
项目 c.1456T>G c.1198A>C c.1091C>T c.211G>A |D' |值
c.1456T>G0.9962 0.9991 0.1845 c.1198A>C 0.988 0.0792 c.1091C>T 0.9954 c.211G>a r2 c.1456T>G 0.0404 0.1980 0.0034 c.1198A>C 0.0073 0.0023 c.1091C>T 0.0197 c.211G>a 表 5 UGT1A1基因单倍型分布
Table 5. Haplotype of UGTIA1 gene
单倍型 c.1456T>G c.1198A>C c.1091C>T c.211G>A 1 G A C G 2 T A C G 3 T A T G 4 G A C A 5 T C C G 6 T A C A 表 6 不同性别的UGT1A1基因变异频谱[n(%)]
Table 6. UGT1A1 gene variation spectrum of different sex [n(%)]
突变位点 组别 性别 X-squared P 男(n=28) 女(n=25) c.1456T>G 野生型(TT) 13(0.46) 8(0.32) 2.1548 0.3405 杂合突变型(TG) 6(0.21) 4(0.16) 纯合突变型(GG) 9(0.32) 13(0.52) c.1198A>C 野生型(AA) 2(0.85) 25(1.00) NA NA 杂合突变型(AC) 4(0.85) 0(0.00) 纯合突变型(CC) 0(0.00) 0(0.00) c.1091C>T 野生型(CC) 19(0.67) 20(0.80) 2.4698 0.2909 杂合突变型(CT) 8(0.28) 3(0.12) 纯合突变型(TT) 1(0.03) 2(0.08) c.211G>A 野生型(GG) 26(0.92) 21(0.84) 6.3826 0.0411* 杂合突变型(GA) 2(0.92) 0(0.00) 纯合突变型(AA) 0(0.00) 4(0.16) 表 7 不同民族的UGT1A1基因变异频谱[n(%)]
Table 7. UGT1A1 gene variation spectrum of different ethnic groups[n(%)]
基因突变位点 组别 民族 X-squared P 汉族(n=25) 少数民族(n=28) c.1456T>G 野生型(TT) 14(0.56) 7(0.25) 6.7305 0.0345* 杂合突变型(TG) 5(0.20) 5(0.17) 纯合突变型(GG) 6(0.24) 16(0.57) c.1198A>C 野生型(AA) 24(0.96) 25(0.89) NA NA 杂合突变型(AC) 1(0.04) 3(0.10) 纯合突变型(CC) 0(0.00) 0(0.00) c.1091C>T 野生型(CC) 16(0.64) 23(0.82) 4.1909 0.1230 杂合突变型(CT) 6(0.24) 5(0.17) 纯合突变型(TT) 3(0.12) 0(0.00) c.211G>A 野生型(GG) 23(0.92) 24(0.85) 0.8542 0.6524 杂合突变型(GA) 1(0.04) 1(0.03) 纯合突变型(AA) 1(0.04) 3(0.10) -
[1] Sun L,Li M,Zhang L,et al. Differences in UGT1A1 gene mutations and pathological liver changes between Chinese patients with Gilbert syndrome and Crigler-Najjar syndrome type II[J]. Medicine (Baltimore),2017,96(45):e8620. [2] Canu G,Minucci A,Zuppi C,et al. Gilbert and Crigler Najjar syndromes: An update of the UDP-glucuronosyltransferase 1A1 (UGT1A1) gene mutation database[J]. Blood Cells Mol Dis,2013,50(4):273-280. doi: 10.1016/j.bcmd.2013.01.003 [3] Li L,Deng G,Tang Y,et al. Spectrum of UGT1A1 variations in Chinese patients with Crigler-Najjar syndrome type II[J]. PLoS One,2015,10(5):e0126263. doi: 10.1371/journal.pone.0126263 [4] Chen H L,Wu S H,Hsu S H,et al. Recent advances in the diagnosis and treatment of inherited cholestatic liver diseases[J]. J Biomed Sci,2018,25(1):75. doi: 10.1186/s12929-018-0475-8 [5] Ivanov A,Semenova E. Bilirubin level and UGT1A1 28 genotype in men of north-west region of Russia[J]. J Clin Exp Hepatol,2021,11(6):691-699. doi: 10.1016/j.jceh.2021.01.006 [6] Trabelsi N,Chaouch L,Haddad F,et al. Novel mutations in Uridyl-diphosphate-glucuronosyl-transferase 1A1 (UGT1A1) gene in Tunisian patients with unconjugated hyperbilirubinemia[J]. Eur J Med Genet,2021,64(2):104-139. [7] Shiu T Y,Huang H H,Lin H H,et al. Restriction fragment length polymorphism effectively identifies exon 1 mutation of UGT1A1 gene in patients with Gilbert's Syndrome[J]. Liver Int,2015,35(8):2050-2056. doi: 10.1111/liv.12785 [8] Maruo Y,Nakahara S,Yanagi T,et al. Genotype of UGT1A1 and phenotype correlation between Crigler-Najjar syndrome type II and Gilbert syndrome[J]. J Gastroenterol Hepatol,2016,31(2):403-408. doi: 10.1111/jgh.13071 [9] Li Y,Qu Y J,Zhong X M,et al. Two novel mutations and a patient with loss of heterozygosity of UGT1A1 gene[J]. J Zhejiang Univ Sci B,2014,15(5):474-481. doi: 10.1631/jzus.B1300233 [10] Xiong Q F,Zhong Y D,Feng X N,et al. Study on spectrum of UGT1A1 mutations in connection with inherited non-hemolytic unconjugated hyperbilirubinemia[J]. Zhonghua Gan Zang Bing Za Zhi,2018,26(12):898-902. [11] Abuduxikuer K,Fang L J,Li L T,et al. UGT1A1 genotypes and unconjugated hyperbilirubinemia phenotypes in post-neonatal Chinese children[J]. Medicine (Baltimore),2018,97(49):e13576. [12] Sampietro M,Lolascon A. Molecular pathology of Crigler-Najjar type I and II and Gilbert's syndromes[J]. Haematologica,1999,84(2):150-157. [13] 陈伟,林美丽,王玉,等. UGT1A1基因多态性与新生儿不明原因非结合性高胆红素血症相关性研究[J]. 中华新生儿科杂志,2019,34(2):81-86. -





 下载:
下载: